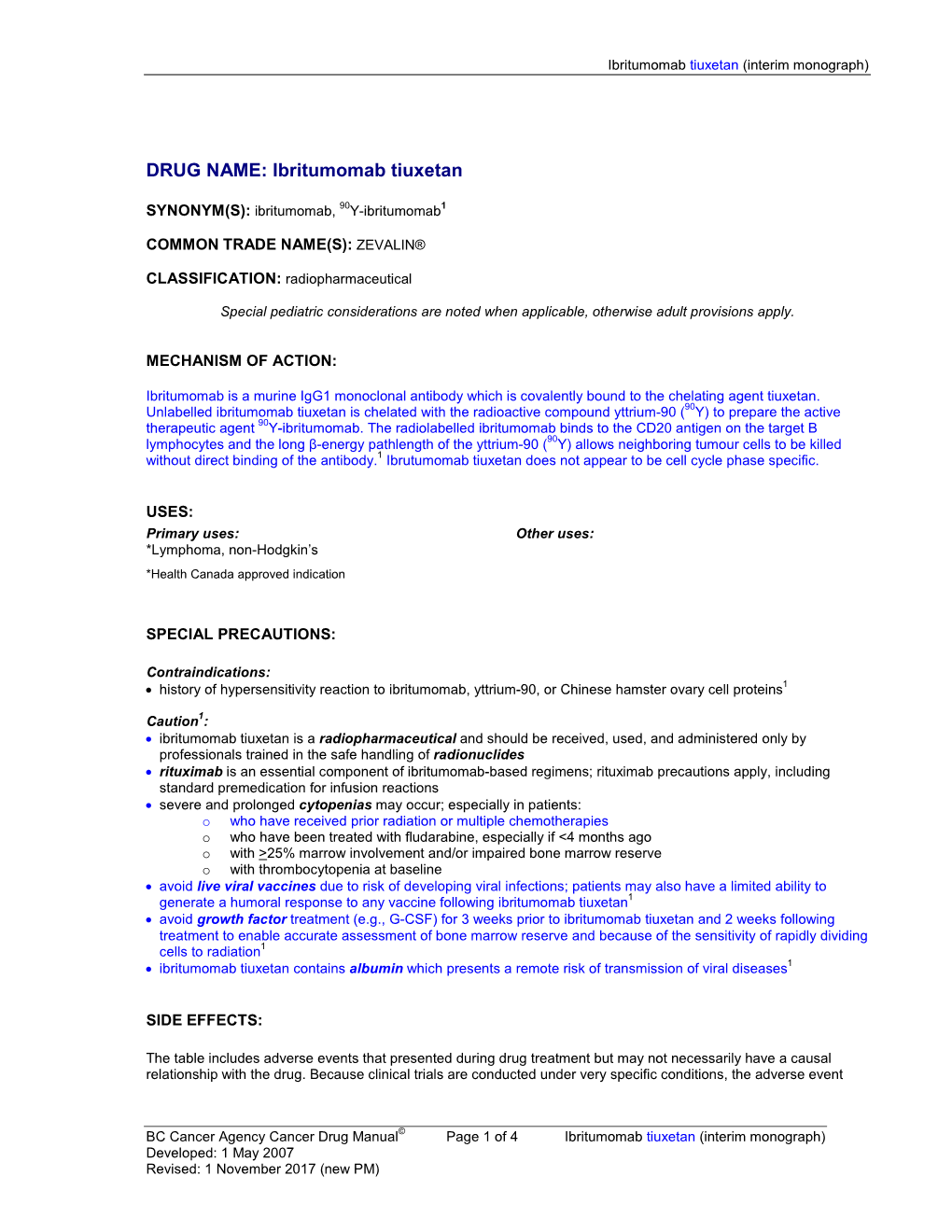
Ibritumomab Tiuxetan (Interim Monograph)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Activity of Rituximab and Ofatumumab Against Mantle
ACTIVITY OF RITUXIMAB AND OFATUMUMAB AGAINST MANTLE CELL LYMPHOMA(MCL) IN VITRO IN MCL CELL LINES BY COMPLEMENT DEPENDENT CYTOTOXICITY (CDC)AND ANTIBODY-DEPENDENT CELL MEDIATED CYTOTOXICITY ASSAYS(ADCC) Dr. Gopichand Pendurti M.B.B.S Mentor: Dr. Francisco J. Hernandez-Ilizaliturri MD Overview of presentation •Introduction to mantle cell lymphoma. •Concept of minimal residual disease. •Anti CD 20 antibodies. •51Cr release assays. •Flow cytometry on cell lines. •Results. •Future. MANTLE CELL LYMPHOMA •Mantle cell lymphoma is characterized by abnormal proliferation of mature B lymphocytes derived from naïve B cells. •Constitutes about 5% of all patients with Non Hodgkin's lymphoma. •Predominantly in males with M:F ratio 2.7:1 with onset at advanced age (median age 60yrs). •It is an aggressive lymphoma with median survival of patients being 3-4 years. •Often presents as stage III-IV with lymphadenopathy, hepatosplenomegaly, gastrointestinal involvement, peripheral blood involvement. Pedro Jares, Dolors Colomer and Elias Campo Genetic and molecular pathogenesis of mantle cell lymphoma: perspectives for new targeted therapeutics Nature revision of cancer 2007 October:7(10):750-62 •Genetic hallmark is t(11:14)(q13:q32) translocation leading to over expression of cyclin D1 which has one of the important pathogenetic role in deregulating the cell cycle. •Other pathogentic mechanisms include molecular and chromosomal alterations that Target proteins that regulate the cell cycle and senecense (BMI1,INK4a,ARF,CDK4 AND RB1). Interfere with cellular -

Alemtuzumab Comparison with Rituximab and Leukemia Whole
Mechanism of Action of Type II, Glycoengineered, Anti-CD20 Monoclonal Antibody GA101 in B-Chronic Lymphocytic Leukemia Whole Blood Assays in This information is current as Comparison with Rituximab and of September 29, 2021. Alemtuzumab Luca Bologna, Elisa Gotti, Massimiliano Manganini, Alessandro Rambaldi, Tamara Intermesoli, Martino Introna and Josée Golay Downloaded from J Immunol 2011; 186:3762-3769; Prepublished online 4 February 2011; doi: 10.4049/jimmunol.1000303 http://www.jimmunol.org/content/186/6/3762 http://www.jimmunol.org/ Supplementary http://www.jimmunol.org/content/suppl/2011/02/04/jimmunol.100030 Material 3.DC1 References This article cites 44 articles, 24 of which you can access for free at: http://www.jimmunol.org/content/186/6/3762.full#ref-list-1 by guest on September 29, 2021 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2011 by The American -

Neuro-Ophthalmic Side Effects of Molecularly Targeted Cancer Drugs
Eye (2018) 32, 287–301 © 2018 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0950-222X/18 www.nature.com/eye 1,2,3 4 Neuro-ophthalmic side MT Bhatti and AKS Salama REVIEW effects of molecularly targeted cancer drugs Abstract The past two decades has been an amazing time culminated in indescribable violence and in the advancement of cancer treatment. Mole- unspeakable death. However, amazingly within cularly targeted therapy is a concept in which the confines of war have risen some of the specific cellular molecules (overexpressed, greatest advancements in medicine. It is within mutationally activated, or selectively expressed this setting—in particular World War II with the proteins) are manipulated in an advantageous study of mustard gas—that the annals of cancer manner to decrease the transformation, prolif- chemotherapy began touching the lives of eration, and/or survival of cancer cells. In millions of people. It is estimated that in 2016, addition, increased knowledge of the role of the over 1.6 million people in the United States will immune system in carcinogenesis has led to the be diagnosed with cancer and over a half a development of immune checkpoint inhibitors million will die.1 The amount of money being to restore and enhance cellular-mediated anti- spent on research and development of new tumor immunity. The United States Food and cancer therapies is staggering with a record $43 Drug Administration approval of the chimeric billion dollars spent in 2014. Nearly 30% of all monoclonal antibody (mAb) rituximab in 1997 registered clinical trials on the clinicaltrials.gov 1Department of for the treatment of B cell non-Hodgkin lym- website pertain to cancer drugs. -

Whither Radioimmunotherapy: to Be Or Not to Be? Damian J
Published OnlineFirst April 20, 2017; DOI: 10.1158/0008-5472.CAN-16-2523 Cancer Perspective Research Whither Radioimmunotherapy: To Be or Not To Be? Damian J. Green1,2 and Oliver W. Press1,2,3 Abstract Therapy of cancer with radiolabeled monoclonal antibodies employing multistep "pretargeting" methods, particularly those has produced impressive results in preclinical experiments and in utilizing bispecific antibodies, have greatly enhanced the thera- clinical trials conducted in radiosensitive malignancies, particu- peutic efficacy of radioimmunotherapy and diminished its toxi- larly B-cell lymphomas. Two "first-generation," directly radiola- cities. The dramatically improved therapeutic index of bispecific beled anti-CD20 antibodies, 131iodine-tositumomab and 90yttri- antibody pretargeting appears to be sufficiently compelling to um-ibritumomab tiuxetan, were FDA-approved more than a justify human clinical trials and reinvigorate enthusiasm for decade ago but have been little utilized because of a variety of radioimmunotherapy in the treatment of malignancies, particu- medical, financial, and logistic obstacles. Newer technologies larly lymphomas. Cancer Res; 77(9); 1–6. Ó2017 AACR. "To be, or not to be, that is the question: Whether 'tis nobler in the pembrolizumab (anti-PD-1), which are not directly cytotoxic mind to suffer the slings and arrows of outrageous fortune, or to take for cancer cells but "release the brakes" on the immune system, arms against a sea of troubles, And by opposing end them." Hamlet. allowing cytotoxic T cells to be more effective at recognizing –William Shakespeare. and killing cancer cells. Outstanding results have already been demonstrated with checkpoint inhibiting antibodies even in far Introduction advanced refractory solid tumors including melanoma, lung cancer, Hodgkin lymphoma and are under study for a multi- Impact of monoclonal antibodies on the field of clinical tude of other malignancies (4–6). -

Monoclonal Antibodies
MONOCLONAL ANTIBODIES ALEMTUZUMAB ® (CAMPATH 1H ) I. MECHANISM OF ACTION Antibody-dependent lysis of leukemic cells following cell surface binding. Alemtuzumab is a recombinant DNA-derived humanized monoclonal antibody that is directed against surface glycoprotein CD52. CD52 is expressed on the surface of normal and malignant B and T lymphocytes, NK cells, monocytes, macrophages, a subpopulation of granulocytes, and tissues of the male reproductive system (CD 52 is not expressed on erythrocytes or hematopoietic stem cells). The alemtuzumab antibody is an IgG1 kappa with human variable framework and constant regions, and complementarity-determining regions from a murine monoclonal antibody (campath 1G). II. PHARMACOKINETICS Cmax and AUC show dose proportionality over increasing dose ranges. The overall average half-life is 12 days. Peak and trough levels of Campath rise during the first weeks of Campath therapy, and approach steady state by week 6. The rise in serum Campath concentration corresponds with the reduction in malignant lymphocytes. III. DOSAGE AND ADMINISTRATION Campath can be administered intravenously or subcutaneously. Intravenous: Alemtuzumab therapy should be initiated at a dose of 3 mg administered as a 2-hour IV infusion daily. When the 3 mg dose is tolerated (i.e., ≤ Grade 2 infusion related side effects), the daily dose should be escalated to 10mg and continued until tolerated (i.e., ≤ Grade 2 infusion related side effects). When the 10 mg dose is tolerated, the maintenance dose of 30 mg may be initiated. The maintenance dose of alemtuzumab is 30 mg/day administered three times a week on alternate days (i.e. Monday, Wednesday, and Friday), for up to 12 weeks. -

Role of Intrathecal Rituximab and Trastuzumab in the Management of Leptomeningeal Carcinomatosis
Butler University Digital Commons @ Butler University Scholarship and Professional Work – COPHS College of Pharmacy & Health Sciences 2010 Role of Intrathecal Rituximab and Trastuzumab in the Management of Leptomeningeal Carcinomatosis Anthony J. Perissinotti David J. Reeves Butler University, [email protected] Follow this and additional works at: https://digitalcommons.butler.edu/cophs_papers Part of the Oncology Commons, and the Pharmacy and Pharmaceutical Sciences Commons Recommended Citation Perissinotti, Anthony J. and Reeves, David J., "Role of Intrathecal Rituximab and Trastuzumab in the Management of Leptomeningeal Carcinomatosis" (2010). Scholarship and Professional Work – COPHS. 208. https://digitalcommons.butler.edu/cophs_papers/208 This Article is brought to you for free and open access by the College of Pharmacy & Health Sciences at Digital Commons @ Butler University. It has been accepted for inclusion in Scholarship and Professional Work – COPHS by an authorized administrator of Digital Commons @ Butler University. For more information, please contact [email protected]. Role of Intrathecal Rituximab and Trastuzumab in the Management of Leptomeningeal Carcinomatosis Anthony J Perissinotti David J Reeves Abstract OBJECTIVE: To review evidence for the use of intrathecal rituximab and trastuzumab in the management of leptomeningeal carcinomatosis. DATA SOURCES: A search of MEDLINE (1966-July 2010) and International Pharmaceutical Abstracts (1970-July 2010) was performed using search terms intrathecal, trastuzumab, rituximab, and monoclonal antibody. Additionally, American Society of Clinical Oncology, San Antonio Breast Conference, American Association for Cancer Research, and American Society of Hematology meeting abstracts were searched. STUDY SELECTION AND DATA EXTRACTION: Publications were reviewed for inclusion. Those reporting use of rituximab and trastuzumab intrathecally are reviewed and include 1 Phase 1 trial, 2 small prospective studies, 1 case series, and 15 case reports. -

Antibody-Drug Conjugates (Adcs) – Biotherapeutic Bullets
Sean L Kitson Antibody-Drug Conjugates (ADCs) – Biotherapeutic bullets SEAN L KITSON*, DEREK J QUINN, THOMAS S MOODY, DAVID SPEED, WILLIAM WATTERS, DAVID ROZZELL *Corresponding author Almac, Department of Biocatalysis and Isotope Chemistry, 20 Seagoe Industrial Estate, Craigavon, BT63 5QD, United Kingdom (chimeric human-murine IgG1 targeting EGF receptor) and KEYWORDS panitumumab (human IgG2 targeting EGF receptor) for the Antibody-drug conjugate; ADC; monoclonal antibody; treatment of metastatic colorectal cancer (5). cancer; carbon-14; linker; immunotherapy. This technology of tailoring MAbs has been exploited to develop delivery systems for radionuclides to image and treat a variety of cancers (6). This led to the hypothesis that a ABSTRACT cancer patient would first receive a radionuclide antibody capable of imaging the tumour volume. The images of the Immunotherapies especially targeted towards oncology, tumour are obtained by using one or more combinations of based on antibody-drug conjugates (ADCs) have the following methods: planar imaging; single photon recently been boosted by the US Food and Drug emission computed tomography (SPECT) and positron Administration approval of Adcetris to treat Hodgkin’s emission tomography (PET) (7). These techniques can be lymphoma and Kadcyla for metastatic breast cancer. extended to hybrid imaging systems incorporating PET (or The emphasis of this article is to provide an overview of SPECT) with computed tomography (CT) or magnetic the design of ADCs in order to examine their ability to 30 resonance imaging (MRI) (8). find and kill tumour cells. A particular focus will be on the relationship between the cytotoxic drug, chemical The imaging process is first used to locate the precise position linker and the type of monoclonal antibody (MAb) used of the tumour and ascertain the appropriate level of the to make up the components of the ADC. -

Imatinib (Gleevec™)
Biologicals What Are They? When Did All of this Happen? There are Clear Benefits. Are there also Risks? Brian J Ward Research Institute of the McGill University Health Centre Global Health, Immunity & Infectious Diseases Grand Rounds – March 2016 Biologicals Biological therapy involves the use of living organisms, substances derived from living organisms, or laboratory-produced versions of such substances to treat disease. National Cancer Institute (USA) What Effects Do Steroids Have on Immune Responses? This is your immune system on high dose steroids projects.accessatlanta.com • Suppress innate and adaptive responses • Shut down inflammatory responses in progress • Effects on neutrophils, macrophages & lymphocytes • Few problems because use typically short-term Virtually Every Cell and Pathway in Immune System ‘Target-able’ (Influenza Vaccination) Reed SG et al. Nature Medicine 2013 Nakaya HI et al. Nature Immunology 2011 Landscape - 2013 Antisense (30) Cell therapy (69) Gene Therapy (46) Monoclonal Antibodies (308) Recombinant Proteins (93) Vaccines (250) Other (81) http://www.phrma.org/sites/default/files/pdf/biologicsoverview2013.pdf Therapeutic Category Drugs versus Biologics Patented Ibuprofen (Advil™) Generic Ibuprofen BioSimilars/BioSuperiors ? www.drugbank.ca Patented Etanercept (Enbrel™) BioSimilar Etanercept Etacept™ (India) Biologics in Cancer Therapy Therapeutic Categories • Hormonal Therapy • Monoclonal antibodies • Cytokine therapy • Classical vaccine strategies • Adoptive T-cell or dendritic cells transfer • Oncolytic -

Hodgkin's Lymphoma Unresponsive to Rituximab Or a Rituximab
Clinical Development GSK1841157 Protocol OMB110918 / NCT01077518 A Randomized, Open Label Study of Ofatumumab and Bendamustine Combination Therapy Compared with Bendamustine Monotherapy in Indolent B-cell Non- Hodgkin’s Lymphoma Unresponsive to Rituximab or a Rituximab-Containing Regimen During or Within Six Months of Treatment Authors Document type Amended Protocol Version EUDRACT number 2008-004177-17 Version number 11 Development phase III Document status Final Release date 13-Apr-2017 Novartis internal reference number COMB157E2301 Property of Novartis Confidential May not be used, divulged, published, or otherwise disclosed without the consent of Novartis Novartis Confidential Page 2 Amended Protocol Version 11 Clean Protocol No. COMB157E2301/OMB110918 Amendment 9 (13-Apr-2017) Amendment rationale The purpose of amendment 9 is to revise the total number of events required for the primary analysis of the primary end point PFS. The primary analysis was planned after reaching 259 PFS events as determined by an Independent Review Committee (IRC). Based on the current status of the study and PFS event count by IRC, it is highly unlikely that the 259 PFS events will be achieved. The study has been ongoing since September 2010 when the first patient was enrolled and the study sponsorship changed in February 2016 from GSK to Novartis (Amendment 8 , dated 18Mar2016). Per protocol, Interim Analysis for efficacy and futility and IDMC review occurred (22Feb2016) after 180 PFS events by IRC were reached (31Oct2015). IDMC recommended to continue the study without changes. The interim analysis of PFS was performed by an independent Statistical Data Analysis Centre. As per IDMC charter, unblinded results were not communicated to the sponsor in order to maintain the integrity of the trial. -

Mabthera, INN-Rituximab
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT MabThera 100 mg concentrate for solution for infusion MabThera 500 mg concentrate for solution for infusion 2. QUALITATIVE AND QUANTITATIVE COMPOSITION MabThera 100 mg concentrate for solution for infusion Each mL contains 10 mg of rituximab. Each 10 mL vial contains 100 mg of rituximab. MabThera 500 mg concentrate for solution for infusion Each mL contains 10 mg of rituximab. Each 50 mL vial contains 500 mg of rituximab. Rituximab is a genetically engineered chimeric mouse/human monoclonal antibody representing a glycosylated immunoglobulin with human IgG1 constant regions and murine light-chain and heavy-chain variable region sequences. The antibody is produced by mammalian (Chinese hamster ovary) cell suspension culture and purified by affinity chromatography and ion exchange, including specific viral inactivation and removal procedures. Excipients with known effects Each 10 mL vial contains 2.3 mmol (52.6 mg) sodium. Each 50 mL vial contains 11.5 mmol (263.2 mg) sodium. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Concentrate for solution for infusion. Clear, colourless liquid with pH of 6.2 – 6.8 and osmolality of 324 - 396 mOsmol/kg . 4. CLINICAL PARTICULARS 4.1 Therapeutic indications MabThera is indicated in adults for the following indications: Non-Hodgkin’s lymphoma (NHL) MabThera is indicated for the treatment of previously untreated adult patients with stage III-IV follicular lymphoma in combination with chemotherapy. MabThera maintenance therapy is indicated for the treatment of adult follicular lymphoma patients responding to induction therapy. -

Ibritumomab Tiuxetan (Zevalin)
Ibritumomab tiuxetan (Zevalin) Policy Number: Original Effective Date: MM.04.013 03/11/2003 Line(s) of Business: Current Effective Date: HMO; PPO 06/22/2012 Section: Prescription Drugs Place(s) of Service: Outpatient I. Description Ibritumomab tiuxetan (Zevalin) is a CD20-directed radiotherapeutic antibody administered as part of the ibritumomab tiuxetan therapeutic regimen indicated for the treatment of patients with relapsed or refractory, low-grade or follicular B-cell non-Hodgkin’s lymphoma (NHL) and for the treatment of patients with previously untreated follicular NHL who have achieved a partial or complete response to first-line chemotherapy. Ibritumomab tiuxetan is comprised of two separate components, indium-111(IN-111) the diagnostic component and yttrium-90 (Y-90) the therapeutic component. The ibritumomab tiuxetan regimen includes the administration of rituximab followed by IN-111, which targets and binds to the tumor cell. If the IN-111 binds successfully to the tumor cells, seven to nine days later, a second dose of rituximab is administered followed by Y-90 which damages the targeted tumor cells. II. Criteria/Guidelines A. The ibritumomab tiuxetan therapeutic regimen is covered (subject to Limitations/Exclusions and Administrative Guidelines) when recommended by an oncologist for the following conditions: 1. Non-Hodgkin’s lymphoma (NHL) a. For the treatment of patients with relapsed or refractory, low-grade or follicular B-cell NHL b. For the treatment of patients with follicular NHL who achieve a partial or complete response to first-line chemotherapy 2. For the indications listed above, the following criteria must be met: a. Lymphoma involvement of the bone is less than 25 percent Ibritumomab tiuxetan (Zevalin) 2 b. -

Cetuximab Promotes Anticancer Drug Toxicity in Rhabdomyosarcomas with EGFR Amplificationin Vitro
ONCOLOGY REPORTS 30: 1081-1086, 2013 Cetuximab promotes anticancer drug toxicity in rhabdomyosarcomas with EGFR amplificationin vitro YUKI YAMAMOTO1*, KAZUMASA FUKUDA2*, YASUSHI FUCHIMOTO4*, YUMI MATSUZAKI3, YOSHIRO SAIKAWA2, YUKO KITAGAWA2, YASUHIDE MORIKAWA1 and TATSUO KURODA1 Departments of 1Pediatric Surgery, 2Surgery and 3Physiology, Keio University School of Medicine, Tokyo 160-858; 4Division of Surgery, Department of Surgical Subspecialities, National Center for Child Health and Development, Tokyo 157-8535, Japan Received January 15, 2013; Accepted April 2, 2013 DOI: 10.3892/or.2013.2588 Abstract. Overexpression of human epidermal growth factor i.e., t(2;13) (q35;q14) in 55% of cases and t(1;13) (p36;q14) in receptor (EGFR) has been detected in various tumors and is 22% of cases (1). Current treatment options include chemo- associated with poor outcomes. Combination treatment regi- therapy, complete surgical resection and radiotherapy (3). mens with EGFR-targeting and cytotoxic agents are a potential However, the prognosis for patients with advanced-stage RMS therapeutic option for rhabdomyosarcoma (RMS) with EGFR is quite poor (4). The main problems with clinical treatments amplification. We investigated the effects of combination include metastatic invasion, local tumor recurrence and multi- treatment with actinomycin D and the EGFR-targeting agent drug resistance. Therefore, more specific, effective and less cetuximab in 4 RMS cell lines. All 4 RMS cell lines expressed toxic therapies are required. wild-type K-ras, and 2 of the 4 overexpressed EGFR, as Numerous novel anticancer agents are currently in early determined by flow cytometry, real-time PCR and direct phase clinical trials. Of these, immunotherapy with specific sequencing.