Involvement of the Eye in Protein Malnutrition * -303
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Topical Serum for Treatment of Keratomalacia
PROCEDURES PRO > OPHTHALMOLOGY > PEER REVIEWED Topical Serum for Treatment of Keratomalacia Amy Knollinger, DVM, DACVO Eye Care for Animals Salt Lake City, Utah Corneal Anatomy An understanding of corneal anatomy is vital to determine if serum therapy for the treatment of keratomalacia should be initiated. The cornea makes up the anterior por- tion of the globe and provides multiple functions for vision: it is transparent (despite originating from surface ectoderm), thereby allowing for clear vision; it acts as the major refractive (bending of light) surface of the globe; and it provides a protective barrier between the globe and the environment The cornea consists of 4 layers in domestic species, being approximately 0.45–0.55 mm thick in the normal dog. The corneal epithelium is the most external layer overly- What You Will Need ing the stromal layer, which accounts for 90% of the total corneal thickness. The cor- n Sterile gloves neal epithelium in the dog and cat is 5–11 cells thick and has a turnover rate of n approximately 7 days.1 The stroma is made up of collagen fibers, which are precisely Clean #40 clipper blade arranged in parallel sheets running the entire diameter of the cornea, allowing for its n Chlorhexidine scrub and solution transparency. The third layer is an acellular membrane (ie, Descemet’s membrane), n Sterile needle and syringe which forms the basement membrane for the innermost layer, the endothelium. The n corneal endothelium is a single layer of hexagonally shaped cells forming the internal Red top sterile blood collection or barrier between the anterior chamber and the cornea.2 serum separator tube n Centrifuge Corneal Disease n Sterile pipette Corneal ulcers are classified by underlying cause. -

Kwashiokorl. Description of Kwashiorkor Kwashiorkor Is a Life-Threatening and Debilitating Form of Malnutrition. It's Caused B
Name ;OLAWUYI MUQTADIR OREDOLAPO COUSE AFE 101 DEPARTMENT ;ACCOUNTING KWASHIOKORl. Description of kwashiorkor kwashiorkor is a life-threatening and debilitating form of malnutrition. It’s caused by a lack of protein in your diet. Kwashiorkor is also commonly seen in low- and lower-middle-income regions facing famine. Signs and symptoms of kwashiorkor The symptoms of kwashiorkor include; • damaged immune system, which can lead to more frequent and severe infections • irritability. • flaky rash • shock. • change in skin and hair colour (to a rust colour) and texture • fatigue • diarrhea • loss of muscle mass • failure to grow or gain weight • edema (swelling) of the ankles, feet, and belly SUSCEPTIBLES If kwashiorkor is suspected, your doctor will first examine you to check for an enlarged liver (hepatomegaly) and swelling. Next, blood and urine tests may be ordered to measure the level of protein and sugar in your blood. Other tests may be performed on your blood and urine to measure signs of malnutrition and lack of protein. These tests may look for muscle breakdown and assess kidney function, overall health, and growth. These tests include: arterial blood gas, blood urea nitrogen , urinalysis e.t.c. TREATMENT Kwashiorkor can be corrected by eating more protein and more calories overall, especially if treatment is started early. You may first be given more calories in the form of carbohydrates, sugars, and fats. Once these calories provide energy, you will be given foods with proteins. Foods must be introduced and calories should be increased slowly because you have been without proper nutrition for a long period. Your body may need to adjust to the increased intake. -

JMSCR Vol||08||Issue||02||Page 208-210||February 2020
JMSCR Vol||08||Issue||02||Page 208-210||February 2020 http://jmscr.igmpublication.org/home/ ISSN (e)-2347-176x ISSN (p) 2455-0450 DOI: https://dx.doi.org/10.18535/jmscr/v8i2.40 Keratomalacia - A Case Report Authors Deepthi Pullepu1*, Deepthi Janga2, V Murali Krishna3 *Corresponding Author Deepthi Pullepu Department of Ophthalmology, Rangaraya Medical College, Kakinada, Andhra Pradesh, India Abstract Xerophthalmia refers to an ocular condition of destructive dryness of conjunctiva and cornea caused due to severe vitamin A deficiency. Usually affects infants, children and women of reproductive age group. It is estimated to affect about one-third of children under the age of five around the world. Keratomalacia means dry and cloudy cornea which melts and perforates, caused due to severe vitamin A deficiency. Here we describe a case of 21 year old female with neurofibromatosis type 1 presenting with keratomalacia. Keywords: Vitamin A deficiency, Xerophthalmia, Keratomalacia. Introduction blindness is a significant contributor Vitamin A is essential for the functioning of the In India, it is estimated that there are immune system, healthy growth and development approximately 6.8 million people who have vision of body and is usually acquired through diet. less than 6/60 in at least one eye due to corneal Globally, 190 million children under five years of diseases; of these, about a million have bilateral age are affected by vitamin A deficiency involvement. They suffer from an increased risk of visual Corneal blindness resulting due to this disease can impairment, illness and death from childhood be completely prevented by institution of effective infections such as measles and those causing preventive or prophylactic measures at the diarrhoea community level. -
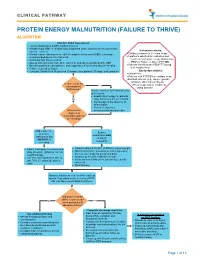
Protein Energy Malnutrition (Failure to Thrive) Algorithm
CLINICAL PATHWAY PROTEIN ENERGY MALNUTRITION (FAILURE TO THRIVE) ALGORITHM Conduct Initial Assessment • History and physical (H&P), nutrition focused • Weight height, BMI, % of ideal body weight and exam: assess severity (symmetric edema = severe) Inclusion criteria: • • Consider basic labs based on H&P; A complete blood count (CBC) is strongly Children newborn to 21 years of age • recommended due to risk of anemia Inpatients admitted for evaluation and • Additional labs based on H&P treatment of Protein Energy Malnutrition • Assess micronutrients: iron, zinc, vitamin D, and others as indicated by H&P (PEM) or Failure to thrive (FTT) OR • • Baseline potassium, phosphorus, and magnesium if concerned about re-feeding Patients identified with PEM/FTT during • Calorie count up to 3 days their hospital stay. • Consults: Social Work, Registered Dietician, Occupational Therapy, and Lactation Exclusion criteria: • Outpatients • Patients with FTT/PEM secondary to an identified concern (e.g., cancer, genetic condition, other chronic illness). Is there a risk for •Pts w/ suspected or confirmed micronutrient Yes eating disorder deficiencies? Initiate treatment for micronutrients deficiencies: • Empiric zinc therapy for patients No older than 6 months for 1 month • Iron therapy in the absence of inflammation • Vitamin D and other What are the micronutrients based on labs degrees of malnutrition and risk of refeeding? Mild, moderate, Severe or severe malnutrition AND malnutrition but at risk of NO RISK of refeeding refeeding • • Initiate feeding per recommended Initiate feeding at 30-50% of RDA for current weight • daily allowance (RDA) for current Monitor potassium, phosphorus, and magnesium weight and age once to twice a day for a total of 4 days • • Use PO route if patient is able to Advance by 10-20% if labs are normal • take 70% of estimated calories If labs abnormal hold off on advancing feed until orally corrected • Start thiamine Advance calories to meet level for catch up growth. -

Nutritional Dermatoses in the Hospitalized Patient
HOSPITAL CONSULT IN PARTNERSHIP WITH THE SOCIETY FOR DERMATOLOGY HOSPITALISTS Nutritional Dermatoses in the Hospitalized Patient Melissa Hoffman, MS; Robert G. Micheletti, MD; Bridget E. Shields, MD Nutritional deficiencies may arise from inadequate nutrient intake, abnormal nutrient absorption, or improper nutrient PRACTICE POINTS utilization.4 Unfortunately, no standardized algorithm for • Nutritional deficiencies are common in hospitalized screening and diagnosing patients with malnutrition exists, patients and often go unrecognized. making early physical examination findings of utmost • Awareness of the risk factors predisposing patients importance. Herein, we present a review of acquired nutri- to nutritional deficiencies and the cutaneous manifes- tional deficiency dermatoses in the inpatient setting. tations associated with undernutrition can promote copy early diagnosis. Protein-Energy Malnutrition • When investigating cutaneous findings, undernutri- tion should be considered in patients with chronic Protein-energy malnutrition (PEM) refers to a set of infections, malabsorptive states, psychiatric illness, related disorders that include marasmus, kwashiorkor and strict dietary practices, as well as in those using (KW), and marasmic KW. These conditions frequently are certain medications. seen in developing countries but also have been reported 5 • Prompt nutritional supplementation can prevent patient in developed nations. Marasmus occurs from a chronic morbidity and mortality and reverse skin disease. deficiencynot of protein and calories. Decreased insulin pro- duction and unopposed catabolism result in sarcopenia and loss of bone and subcutaneous fat.6 Affected patients include children who are less than 60% ideal body weight Cutaneous disease may be the first manifestation of an underlying nutri- 7 tional deficiency, highlighting the importance of early recognition by der- (IBW) without edema or hypoproteinemia. -

A Case of Kwashiorkor Presenting with Pericardial Effusion
orts & Ca Taheri et al., Med Rep Case Stud 2017, 2:2 ep se R S l t a u DOI: 10.4172/2572-5130.1000134 c d i i d e s e M + Medical Reports & Case Studies ISSN: 2572-5130 CaseResearch Report Article Open Access A Case of Kwashiorkor Presenting with Pericardial Effusion Taheri S*, Surak A, Bravo G, McMurray A and Altamirano-Diaz L Department of Paediatrics, Children’s Hospital, London Health Sciences Centre, Western University, London, UK Abstract Introduction: Kwashiorkor is a type of protein-calorie malnutrition often seen in children of impoverished countries and famine. It is a result of insufficient protein intake in the context of adequate caloric intake. Case report: We report a case of a 13-year-old male with trisomy 21 in Southwestern Ontario, Canada who presented with bilateral pneumonia, pericardial effusion and peripheral edema. Evaluation revealed severe dietary restriction, consistent with kwashiorkor. Child was placed on severely restrictive diet, particularly limiting dairy intake to one daily cup of plain, unfortified yogurt. His hospital course was complicated with severe hypocalcemia, hypomagnesemia and hypophosphatemia. These findings resolved gradually upon slow introduction of well-balanced diet and adequate caloric and protein intake. Conclusion: Malnutrition is often underdiagnosed or misdiagnosed in developed countries with devastating outcomes if unrecognized. This makes it imperative to consider this diagnosis, recognize potential risk factors and be prepared to accurately assess overall nutritional status. Keywords: Malnutrition; Kwashiorkor; Case report; pneumonia; in Canada. He is the first child born to parents of East Indian descent Respiratory; Pericardial effusion (unknown exact geographic region). -

Clinical Case Revista Colombiana De Ciencias Pecuarias
Estrada RD et al Melting ulcer in a colt 31 Clinical case Revista Colombiana de Ciencias Pecuarias Melting ulcer in a colt: clinical management and evolution ¤ Úlcera fundente en un potro: manejo clínico y evolución Úlcera colagenolítica em um potro: manejo clínico e evolução Rubén D Estrada 1, MV; Susana Penagos 2, est MV; Elizabeth Viera 2, est MV; Paula A Angulo 2, est MV; Maria P Arias 2*, MV, MS, PhD. 1MV Actividad independiente 2Facultad de Medicina Veterinaria y Zootecnia, Universidad CES, AA 054591, Medellín, Colombia (Received: June 1, 2012; accepted: November 19, 2012) Summary Anamnesis : a colt showing a whitish coloration accompanied by abundant secretion on the left eye was examined. Clinical and laboratory findings: at ophthalmological examination, signs of melting ulcer were observed. Culture isolation revealed positive growing of Flavobacterium sp. and Gram-negative rods. Treatment approach : several keratectomies and tarsorrhaphies, as well as exhaustive antiproteinases, anti- inflammatory, and antibiotic treatments, were conducted. Treatment focused on reducing inflammatory response, eliminating infective organisms, and promoting epithelial healing. Colt showed complete recovery of vision after 3 months. Conclusions: clinical management of melting ulcer implies exhaustive, though unexpensive, treatment. Key words: cornea, keratectomy, keratomalacia, ophthalmology, tarsorrhaphy Resumen Anamnesis : se examinó un potro que presentó una coloración blanquecina acompañada de abundante secreción en el ojo izquierdo. Hallazgos clínicos y de laboratorio : al examen oftalmológico se observaron signos de ulcera fundente. El aislamiento por cultivo mostró crecimiento de Flavobacterium sp. y cocos Gram negativos. Abordaje terapéutico : se realizaron varias queratectomías y tarsorrafias, además de un tratamiento exhaustivo con antiproteinasas, antiinflamatorios y antibióticos enfocado a reducir la respuesta inflamatoria, eliminar los microorganismos infecciosos y promover la cicatrización epitelial. -

Bilateral Keratomalacia Secondary to Diet Induced Vitamin a Deficiency in an Ethiopian Young Woman: a Case Report
Bilateral Keratomalacia… Kumale T. et al. 295 CASE REPORT Bilateral Keratomalacia Secondary to Diet Induced Vitamin A Deficiency in an Ethiopian Young woman: A Case Report Kumale Tolesa Daba1*, Dagmawit Kifle1, Jafer Kedir Ababora1 ABSTRACT OPEN ACCESS BACKGROUND: Diet induced vitamin A deficiency is less Citation: Kumale Tolesa Daba, Dagmawit commonly seen in otherwise healthy adults, due to large store of Kifle, Jafer Kedir Ababora. Bilateral vitamin A in the body. Night blindness is the commonest Keratomalacia Secondary to Diet Induced Vitamin A Deficiency in an Ethiopian manifestation of vitamin A deficiency in adults, whereas Young woman: A Case Report. Ethiop J Keratomalacia is a rare manifestation. Health Sci. 2018;29(2):295 doi:http://dx.doi.org/10.4314/ ejhs. v29i2.18 CASE REPORT: A 27 years old Ethiopian woman came to Jimma Received: June 22, 2018 University Department of Ohthalmology with a compliant of Accepted: October 27, 2018 protrusion of the globe content of both eyes within a week, after Published: March 1, 2019 Copyright: © 2019 Kumale Tolosa Daba, having redness and fear of light of both eyes for 2 months. She was et al. This is an open access article a mother of twins and had low socioeconomic status. On general distributed under the terms of the Creative examination, she was cachectic with enlarged parotid glands. On Commons Attribution License, which permits unrestricted use, distribution, and ocular examination, she was bilaterally blind and had dry ocular reproduction in any medium, provided the surface. There was bilaterally melted cornea with prolapsed uveal original author and source are credited. -

Serum and Red Cell Folates, and Serum Vitamin B12 in Protein Calorie Malnutrition
Arch Dis Child: first published as 10.1136/adc.48.5.366 on 1 May 1973. Downloaded from Archives of Disease in Childhood, 1973, 48, 366. Serum and red cell folates, and serum vitamin B12 in protein calorie malnutrition M. KHALIL, A. TANIOS, M. MOGHAZY, M. K. AREF, S. MAHMOUD, and M. EL LOZY From the Departments of Paediatrics, Clinical Pathology, and Physiology, Faculty of Medicine, University of Alexandria, Alexandria, Egypt Khalil, M., Tanios, A., Moghazy, M., Aref, M. K., Mahmoud, S., and el Lozy, M. (1973). Archives of Disease in Childhood, 48, 366. Serum and red cell folates, and serum vitamin B12 in protein calorie malnutrition. In 22 cases of kwashiorkor, 19 cases of marasmus, and 16 normal controls, red cell folate, serum folate, and serum vitamin B1, were estimated, and the bone marrow and peripheral blood examined. Erythrocyte folate deficiency was shown in 9 cases of kwashiorkor and 7 cases of marasmus. Serum folate deficiency was present in 14 cases of kwashi- orkor and 7 cases of marasmus. Megaloblastosis was found in 45% of cases of kwashiorkor and 37% of cases of marasmus. Megaloblastosis and macrocytosis correlated more with erythrocyte than with serum folate deficiency. Serum vitamin B1, levels in children with kwashiorkor or marasmus did not differ from those of normal controls. The role of folate deficiency in the pathogenesis of megaloblastosis in protein calorie malnutrition was confirmed. copyright. A hypochromic anaemia of iron deficiency is a Material and methods salient finding in patients with protein calorie The study was carried out on 22 infants (12 males and malnutrition (Khalil, Awwad, and Hafez, 1968). -

A Child with Kwashiorkor Misdiagnosed As Atopic Dermatitis
Volume 23 Number 5 | May 2017 Dermatology Online Journal || Letter DOJ 23 (5): 17 A child with kwashiorkor misdiagnosed as atopic dermatitis Marcus Henrique de S B Xavier MD, MsC, Eduardo de Magalhães MD, Gilmar Ferraz Oliveira MD, Mariana Keltke Magalhães MD, Cláudio Prates de Almeida e Oliveira MD, Natália Bragança Oliveira MD Affiliations: Hospital Infantil Padre Anchieta, Belo Horizonte, Minas Gerais, Brazil Corresponding Author: Marcus H. Xavier,MD, MSC, 465 Mangabeira street, Suite 601, Belo Horizonte, MG 30350-170, Brazil, Email: marcus_ [email protected] Abstract The condition is a type of protein-calorie malnutrition most often seen in children of impoverished countries Although uncommon, kwashiorkor continues to occur or areas of famine. Causes are controversial, but the in developed, but mainly in developing nations. It is a most commonly accepted theory is inadequate type of protein-calorie malnutrition that occurs in the dietary protein in the presence of sufficient caloric setting of insufficient protein intake in the presence of intake [1-4]. Children placed on restrictive diets by sufficient caloric intake. Skin and hair changes should ‘‘well-intending’’ parents, as a result of concern for prompt a thorough dietary history and appropriate food allergies, have been reported to be previously dietary intervention. We report a case of a 12-month- at risk of nutritional deficiency, such as kwashiorkor old girl in Belo Horizonte, Minas Gerais, Brazil, who [3, 4]. presented with diffuse edema, desquamation, and irritability misdiagnosed as atopic dermatitis. The Case Synopsis diagnosis was consistent with kwashiorkor as a result A 12-month-old girl presented with a 3-month of severe dietary restriction. -

Therapy-Resistant Dry Itchy Eyes Rima Wardeh* , Volker Besgen and Walter Sekundo
Wardeh et al. Journal of Ophthalmic Inflammation and Infection (2019) 9:13 Journal of Ophthalmic https://doi.org/10.1186/s12348-019-0178-7 Inflammation and Infection BRIEFREPORT Open Access Therapy-resistant dry itchy eyes Rima Wardeh* , Volker Besgen and Walter Sekundo Abstract An 8 years old male presented to our clinic with dry eye symptomes. Different therapiy attemps were made in the last few months and did not lead to any improvement. Examining this patient revealed multiple signs of vitamin A deficiency, which could confirmed by laboratory examination. The initial substitution of vitamin A led to a fast rehabilitation and a following nutrition consulting kept the patient symptom-free over 6 month follow up. Vitamin A deficiency -although rare in the developed countries- is an importent differential diagnosis of the dry eye especially in children. Vitamin A deficiency not only causes ocular manifistaion, but also general symptoms. Dietary change and initial subtitution is the key element for a fast and sustaining improvement. Medical history follow-up examination showed no improvement in the An 8-year-old male child was referred to our pediatric visual acuity nor in the corneal surface. In addition, the ophthalmology department because of burning sensation conjunctiva had developed triangular-shaped superficial and itching in both eyes during the last 4 months. His spots with keratinization in the bulbar conjunctiva nas- mother reported that the child was always pinching his ally, inferiorly, and temporally near the limbus of both eyes while reading or focusing. Topical therapy with eyes. With these findings, the diagnosis of conjunctival dexamethasone eye drops, antihistamine eye drops and corneal xerosis due to vitamin A deficiency was sus- (ketotifen), antibiotic eye drops (ofloxacine) and im- pected. -

The Definition and Classification of Dry Eye Disease
DEWS Definition and Classification The Definition and Classification of Dry Eye Disease: Report of the Definition and Classification Subcommittee of the International Dry E y e W ork Shop (2 0 0 7 ) ABSTRACT The aim of the DEWS Definition and Classifica- I. INTRODUCTION tion Subcommittee was to provide a contemporary definition he Definition and Classification Subcommittee of dry eye disease, supported within a comprehensive clas- reviewed previous definitions and classification sification framework. A new definition of dry eye was devel- T schemes for dry eye, as well as the current clinical oped to reflect current understanding of the disease, and the and basic science literature that has increased and clarified committee recommended a three-part classification system. knowledge of the factors that characteriz e and contribute to The first part is etiopathogenic and illustrates the multiple dry eye. Based on its findings, the Subcommittee presents causes of dry eye. The second is mechanistic and shows how herein an updated definition of dry eye and classifications each cause of dry eye may act through a common pathway. based on etiology, mechanisms, and severity of disease. It is stressed that any form of dry eye can interact with and exacerbate other forms of dry eye, as part of a vicious circle. II. GOALS OF THE DEFINITION AND Finally, a scheme is presented, based on the severity of the CLASSIFICATION SUBCOMMITTEE dry eye disease, which is expected to provide a rational basis The goals of the DEWS Definition and Classification for therapy. These guidelines are not intended to override the Subcommittee were to develop a contemporary definition of clinical assessment and judgment of an expert clinician in dry eye disease and to develop a three-part classification of individual cases, but they should prove helpful in the conduct dry eye, based on etiology, mechanisms, and disease stage.