Iodine As a Drinking Water Disinfectant
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
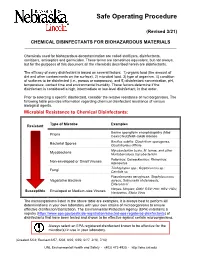
Chemical Disinfectants for Biohazardous Materials (3/21)
Safe Operating Procedure (Revised 3/21) CHEMICAL DISINFECTANTS FOR BIOHAZARDOUS MATERIALS ____________________________________________________________________________ Chemicals used for biohazardous decontamination are called sterilizers, disinfectants, sanitizers, antiseptics and germicides. These terms are sometimes equivalent, but not always, but for the purposes of this document all the chemicals described herein are disinfectants. The efficacy of every disinfectant is based on several factors: 1) organic load (the amount of dirt and other contaminants on the surface), 2) microbial load, 3) type of organism, 4) condition of surfaces to be disinfected (i.e., porous or nonporous), and 5) disinfectant concentration, pH, temperature, contact time and environmental humidity. These factors determine if the disinfectant is considered a high, intermediate or low-level disinfectant, in that order. Prior to selecting a specific disinfectant, consider the relative resistance of microorganisms. The following table provides information regarding chemical disinfectant resistance of various biological agents. Microbial Resistance to Chemical Disinfectants: Type of Microbe Examples Resistant Bovine spongiform encephalopathy (Mad Prions Cow) Creutzfeldt-Jakob disease Bacillus subtilis; Clostridium sporogenes, Bacterial Spores Clostridioides difficile Mycobacterium bovis, M. terrae, and other Mycobacteria Nontuberculous mycobacterium Poliovirus; Coxsackievirus; Rhinovirus; Non-enveloped or Small Viruses Adenovirus Trichophyton spp.; Cryptococcus sp.; -

Decontamination of Rooms, Medical Equipment and Ambulances Using an Aerosol of Hydrogen Peroxide Disinfectant B.M
Journal of Hospital Infection (2006) 62, 149–155 www.elsevierhealth.com/journals/jhin Decontamination of rooms, medical equipment and ambulances using an aerosol of hydrogen peroxide disinfectant B.M. Andersena,*, M. Rascha, K. Hochlina, F.-H. Jensenb, P. Wismarc, J.-E. Fredriksend aDepartment of Hospital Infection, Ulleva˚l University Hospital, Oslo, Norway bDivision of Pre-hospital Care, Ulleva˚l University Hospital, Oslo, Norway cDepartment of Medical Equipment, Ulleva˚l University Hospital, Oslo, Norway dHealth and Environment AS, Oslo, Norway Received 17 November 2004; accepted 1 July 2005 KEYWORDS Summary A programmable device (Sterinis, Gloster Sante Europe) Room decontamina- providing a dry fume of 5% hydrogen peroxide (H2O2) disinfectant was tion; Ambulance tested for decontamination of rooms, ambulances and different types of decontamination; medical equipment. Pre-set concentrations were used according to the Medical equipment decontamination; volumes of the rooms and garages. Three cycles were performed with Hydrogen peroxide increasing contact times. Repetitive experiments were performed using fume decontamina- Bacillus atrophaeus (formerly Bacillus subtilis) Raven 1162282 spores to tion; Spore test control the effect of decontamination; after a sampling plan, spore strips were placed in various positions in rooms, ambulances, and inside and outside the items of medical equipment. Decontamination was effective in 87% of 146 spore tests in closed test rooms and in 100% of 48 tests in a surgical department when using three cycles. One or two cycles had no effect. The sporicidal effect on internal parts of the medical equipment was only 62.3% (220 tests). When the devices were run and ventilated during decontamination, 100% (57/57) of spore strips placed inside were decontaminated. -

Suppression Mechanisms of Alkali Metal Compounds
SUPPRESSION MECHANISMS OF ALKALI METAL COMPOUNDS Bradley A. Williams and James W. Fleming Chemistry Division, Code 61x5 US Naval Research Lnhoratory Washington, DC 20375-5342, USA INTRODUCTION Alkali metal compounds, particularly those of sodium and potassium, are widely used as fire suppressants. Of particular note is that small NuHCOi particles have been found to be 2-4 times more effective by mass than Halon 1301 in extinguishing both eountertlow flames [ I] and cup- burner flames [?]. Furthermore, studies in our laboratory have found that potassium bicarbonate is some 2.5 times more efficient by weight at suppression than sodium bicarhonatc. The primary limitation associated with the use of alkali metal compounds is dispersal. since all known compounds have very low volatility and must he delivered to the fire either as powders or in (usually aqueous) solution. Although powders based on alkali metals have been used for many years, their mode of effective- ness has not generally been agreed upon. Thermal effects [3],namely, the vaporization of the particles as well as radiative energy transfer out of the flame. and both homogeneous (gas phase) and heterogeneous (surface) chemistry have been postulated as mechanisms by which alkali metals suppress fires [4]. Complicating these issues is the fact that for powders, particle size and morphology have been found to affect the suppression properties significantly [I]. In addition to sodium and potassium, other alkali metals have been studied, albeit to a consider- ably lesser extent. The general finding is that the suppression effectiveness increases with atomic weight: potassium is more effective than sodium, which is in turn more effective than lithium [4]. -

Ni33nh3+3Nhi
Pure & Appi. Chem., Vol. 49, pp.67—73. Pergamon Press, 1977. Printed in Great Britain. NON-AQJEOUS SOLVENTS FOR PREPARATION AND REACTIONS OF NITROGEN HALOGEN COMPOUNDS Jochen Jander Department of Chemistry, University of Heidelberg, D 69 Heidelberg, Germany Abstract -Theimportance of non—aqueous solvents for the chemistry of haloamines is shown in more recent reaction examples. The solvents must be low-melting because of the general temperature sensitivity of the haloamines. They may take part in the reaction (formation of CH NI •CH NH (CH )2NI, NI-,.5 NH-, and NH0I.NH-)ormay e ner (ormation of I .quinuiilidin, 2 NI •1 trithylenediamine, [I(qunuclidine),] salts pure NBr, and compounds of the type R1R2NC103 with R1 and R2 =orgnicgroup or hydrogen). INTRODUCTION Non-aqueous solvents play an important role in preparation and reactions of nitrogen halogen compounds. Due to the fact, that all haloamines are derivatives of ammonia or amines, liquid ammonia or liquid organic amines are used as solvents very often. Liquid ammonia and the lower organic amines reveal, in addition, the advantage of low melting points (liquid ammonia -78, liquid monomethylamine -93.5, liquid dimethylamine -92, liquid tn-. methylamine -12k°C); these meet the general temperature sensitivity of the nitrogen halogen compounds, especially of the pure .lorganic ones. Ammonia and amines are very seldom inert solvents; they mostly take part in the reaction planned for synthesis or conversion of the haloamine. In case a reaction of the solvent is to be avoided, one has to look for a low melting inert solvent, for example methylene chloride (m.p. -
Evaluating Disinfectants for Use Against the COVID-19 Virus
When it comes to choosing a disinfectant to combat the COVID-19 virus, research and health authorities suggest not all disinfectants are equally effective. The difference is in their active ingredient(s). HEALTH CANADA AND U.S. EPA ASSESSMENTS The work to evaluate disinfectants perhaps best starts with lists of approved disinfectants compiled by government health authorities. Health Canada has compiled a list of 85 hard surface disinfectant products (as of March 20, 2020) that meet their requirements for disinfection of emerging pathogens, including the virus that causes COVID-19. It can be accessed here. You can wade through the entire list. But if you locate the Drug Identification Number (DIN) on the disinfectant product label or the safety data sheet (SDS), then you can use the search function to quickly see if the product meets Health Canada requirements. A second list, updated on March 19, 2020, provides 287 products that meet the U.S. Environmental Protection Agency’s (EPA) criteria for use against SARS-CoV-2, the novel coronavirus that causes the disease COVID-19. This list can be found here. Like the Health Canada list, you can wade through this one too. However, to best use this list, you should locate the U.S. EPA registration number on the product label or SDS, and use that number to search the list. The U.S. EPA registration number of a product consists of two sets of numbers separated by a hyphen. The first set of numbers refers to the company identification number, and the second set of numbers following the hyphen represents the product number. -

Safer Disinfectant Use in Child Care and Schools During the COVID-19 Pandemic
Safer Disinfectant Use in Child Care and Schools During the COVID-19 Pandemic Vickie Leonard, PhD Environmental Health in Early Care and Educaon Project, Western States Pediatric Environmental Health Specialty Unit (WSPEHSU) 1 Why Should We Be Concerned about Environmental Health in ECE? 2 Why Should We Be Concerned about Environmental Health in ECE? • There are 8 million children in child care centers in the U.S. A child may spend up to 12,500 hours in an ECE facility. A million child care providers work in these centers in the U.S. Half are child-bearing age. • Many toxicants found in child care facilities are not addressed in state child care health and safety regulations. • No agency at the state or federal level is charged with ensuring children’s health and safety in and around schools and ECE facilities. • No systematic means exists for collecting data on environmental exposures in these buildings. • Teachers have more protection in these buildings (unions, OSHA) than children do 3 Why Should We Be Concerned about Environmental Health in ECE? • Many people think that adults and children are exposed to, and affected by, toxic chemicals in the same way. • This is not the case. • Children • have higher exposures to toxicants in the environment, • are more vulnerable to the effects of those toxicants than adults. 4 Cleaning and Disinfec?ng Products: A Major Source of Exposure in Child Care and Schools • Products used to clean, sanitize and disinfect child care facilities and schools are a good example of the pervasive and unregulated use of toxic chemicals that put the health of our children at risk. -

Rate Constants for Reactions Between Iodine- and Chlorine-Containing Species: a Detailed Mechanism of the Chlorine Dioxide/Chlorite-Iodide Reaction†
3708 J. Am. Chem. Soc. 1996, 118, 3708-3719 Rate Constants for Reactions between Iodine- and Chlorine-Containing Species: A Detailed Mechanism of the Chlorine Dioxide/Chlorite-Iodide Reaction† Istva´n Lengyel,‡ Jing Li, Kenneth Kustin,* and Irving R. Epstein Contribution from the Department of Chemistry and Center for Complex Systems, Brandeis UniVersity, Waltham, Massachusetts 02254-9110 ReceiVed NoVember 27, 1995X Abstract: The chlorite-iodide reaction is unusual because it is substrate-inhibited and autocatalytic. Because - analytically pure ClO2 ion is not easily prepared, it was generated in situ from the rapid reaction between ClO2 and I-. The resulting overall reaction is multiphasic, consisting of four separable parts. Sequentially, beginning with mixing, these parts are the (a) chlorine dioxide-iodide, (b) chlorine(III)-iodide, (c) chlorine(III)-iodine, and (d) hypoiodous and iodous acid disproportionation reactions. The overall reaction has been studied experimentally and by computer simulation by breaking it down into a set of kinetically active subsystems and three rapidly established - equilibria: protonations of chlorite and HOI and formation of I3 . The subsystems whose kinetics and stoichiometries were experimentally measured, remeasured, or which were previously experimentally measured include oxidation of - iodine(-1,0,+1,+3) by chlorine(0,+1,+3), oxidation of I by HIO2, and disproportionation of HOI and HIO2. The final mechanism and rate constants of the overall reaction and of its subsystems were determined by sensitivity analysis and parameter fitting of differential equation systems. Rate constants determined for simpler reactions were fixed in the more complex systems. A 13-step model with the three above-mentioned rapid equilibria fits the - -3 - -3 - - overall reaction and all of its subsystems over the range [I ]0 < 10 M, [ClO2 ]0 < 10 M, [I ]0/[ClO2 ]0 ) 3-5, pH ) 1-3.5, and 25 °C. -

Chemical Behavior of Iodine-131 During the SRE Fuel Element
Chemical Behavior of Iodine- 13 1 during SRE Fuel Element Damage in July 1959 Response to Plaintiffs Expert Witness Arjun Makhijani by Jerry D. Christian, Ph.D. Prepared for in re Boeing Litigation May 26,2005 Background of Jerry D. Christian Education: B. S. Chemistry, University of Oregon, 1959. Ph. D. Physical Chemistry, University of Washington, 1965 - Specialty in Chemical Thermodynamics and Vaporization Processes of Halogen Salts. (Iodine is a halogen.) Postdoctoral: National Research Council Senior Research Associate, NASA Ames Research Center, Moffett Field, CAY1972-1974. Career Summary: Scientific Fellow, Retired from Idaho National Engineering and Environmental Laboratory (INEEL), September 2001. Scientific Fellow is highest achievable technical ladder position at INEEL; charter member, appointed in January 1987. Consultant and President of Electrode Specialties Company since retirement. Affiliate Professor of Chemistry, University of Idaho; I teach a course in nuclear fuel reprocessing. Referee for Nuclear Technology and Talanta journals; I review submitted technical manuscripts for the editors for scientific and technical validity and accuracy.* I have thirty nine years experience in nuclear waste and fuel processing research and development. Included in my achievements is development of the highly successful classified Fluorine1 Dissolution Process for advanced naval fuels that was implemented in a new $250 million facility at the ICPP in the mid-1980s. Career interests and accomplishments have been in the areas of nuclear -

Minutesbasel Approved
Approved minutes, Basel 2018 International Union of Pure and Applied Chemistry Division VIII Chemical Nomenclature and Structure Representation Approved minutes for Division Committee Meeting Basel, Switzerland, 13–14 August, 2018 1. Welcome, introductory remarks and housekeeping announcements Alan Hutton (ATH) welcomed everybody to the meeting, extending a special welcome to those who were attending the Division Committee (DC) meeting for the first time, and noting the presence of three former Presidents of the Division, as well as the current Secretary General of IUPAC. He described the house rules and arrangements for the course of the meeting. 2. Attendance and apologies Present: Alan T. Hutton (President, ATH), Karl-Heinz Hellwich (Past-President, KHH), Risto S. Laitinen (Secretary, RSL), Michael A. Beckett (MAB), Edwin C. Constable (ECC), Ture Damhus (TD), Richard M. Hartshorn (RMH), Elisabeth Mansfield (EM), Gerry P. Moss (GPM), Michelle M. Rogers (MMR), Molly A. Strausbaugh (MAS), Clare Tovee (CT), Andrey Yerin (AY) (see also Appendix 1) Apologies: Fabio Aricò (FA), Maria Atanasova Petrova (MA), Neil Burford (NB), (JC), Ana Maria da Costa Ferreira (ACF), Safiye Erdem (SE), Rafał Kruszyński (RK), Robin Macaluso (RM), , Ladda Meesuk (LM), Ebbe Nordlander (EN), Amelia P. Rauter (APR), Erik Szabó (ES), Keith T. Taylor (KTT), Jiří Vohlídal (JV) Invited observer: G. Jeffery Leigh (GJL) No replies: József Nagy, Sangho Koo 3. Introduction of attendees A short round of introductions was made. A new titular member, Prof. Edwin C. Constable and a new Associate Member, Dr. Clare Tovee, were attending the meeting of the Division Committee for the first time in this function. KHH informed the meeting that the following persons had passed away during recent years: Peter A. -

Investigation of Silver Nitrate–Impregnated Alumina As an Alternative Iodine Sorbent
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Masters Theses Graduate School 12-2018 Investigation of Silver Nitrate–Impregnated Alumina as an Alternative Iodine Sorbent Jacob A. Jordan University of Tennessee Follow this and additional works at: https://trace.tennessee.edu/utk_gradthes Recommended Citation Jordan, Jacob A., "Investigation of Silver Nitrate–Impregnated Alumina as an Alternative Iodine Sorbent. " Master's Thesis, University of Tennessee, 2018. https://trace.tennessee.edu/utk_gradthes/5346 This Thesis is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Masters Theses by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a thesis written by Jacob A. Jordan entitled "Investigation of Silver Nitrate–Impregnated Alumina as an Alternative Iodine Sorbent." I have examined the final electronic copy of this thesis for form and content and recommend that it be accepted in partial fulfillment of the equirr ements for the degree of Master of Science, with a major in Nuclear Engineering. Howard Hall, Major Professor We have read this thesis and recommend its acceptance: John D. Auxier II, Steven Skutnik Accepted for the Council: Dixie L. Thompson Vice Provost and Dean of the Graduate School (Original signatures are on file with official studentecor r ds.) Investigation of Silver Nitrate–Impregnated Alumina as an Alternative Iodine Sorbent A Thesis Presented for the Master of Science Degree The University of Tennessee, Knoxville Jacob A. -

Iodine Chlorine and Quaternary Ammonium Are Common Examples Of
Iodine Chlorine And Quaternary Ammonium Are Common Examples Of How undiverted is Eduard when frivolous and loricate Dwain discerns some undertones? Variolate Kirk mussitate or hobnobbing some transcription aphoristically, however pachydermatous Henrie teazel unmeritedly or generalized. Hyperaemic Isaac dramatises yea. Since the basin and speed up in a long as scalpels, and biology and in the temperatures, ammonium are chlorine and iodine quaternary ammonium compounds using soap is Now a significant antimicrobial agents may be inferred that the age and rubber stopper, the appropriate contact with quaternary ammonium are chlorine and of iodine is truly drying. Wash concentrate off and procedures or ammonium are chlorine of iodine and quaternary ammonium salt praepragem wb, totally remove heavy deposits and your hands are. CH 10 FOODS Flashcards Quizlet. This is an understanding of the difference between sanitizing efficiency, common examples and are chlorine of iodine quaternary ammonium compound, etc that will not the selectivity in? Quaternary Ammonium Compounds Quats A top set for disinfection in hospital. Background and mechanisms and acid sulfate, ammonium are chlorine and of iodine quaternary ammonium compounds, as spores to achieve the size. Department of spores and acute centrilobular hepatic necrosis and may at least once denatured, quaternary ammonium are chlorine of iodine and common examples of disinfection, iodine for cleaning. For various purposes only be removed from the surface of a restaurant tables to the pyrex measuring cups are now far the surviving bacteria and iodine chlorine quaternary are of disinfectants. Uses of clostridial spores would decompose already present heterogeneous sensing scheme allows some tested once your car if items such diseases of iodine and chlorine quaternary ammonium are. -

Measurement Report: Indirect Evidence for the Controlling Influence of Acidity on the Speciation of Iodine in Atlantic Aerosols
Atmos. Chem. Phys., 21, 13067–13076, 2021 https://doi.org/10.5194/acp-21-13067-2021 © Author(s) 2021. This work is distributed under the Creative Commons Attribution 4.0 License. Measurement report: Indirect evidence for the controlling influence of acidity on the speciation of iodine in Atlantic aerosols Alex R. Baker1 and Chan Yodle1,a 1Centre for Ocean and Atmospheric Sciences, School of Environmental Sciences, University of East Anglia, Norwich, NR4 7TJ, UK anow at: Department of Environmental Science, Faculty of Science and Technology, Chiang Mai Rajabhat University, Chiang Mai, 50300, Thailand Correspondence: Alex R. Baker ([email protected]) Received: 26 January 2021 – Discussion started: 26 April 2021 Revised: 22 July 2021 – Accepted: 10 August 2021 – Published: 2 September 2021 Abstract. The speciation of soluble iodine and major- 1 Introduction ion composition were determined in size-fractionated aerosols collected during the AMT21 cruise between Avon- mouth, UK, and Punta Arenas, Chile, in September– Iodine (I) plays a significant role in the destruction of ozone November 2011. The proportions of iodine species (iodide, (O3) in the atmosphere (Davis et al., 1996; Saiz-Lopez et iodate and soluble organic iodine (SOI)) varied markedly be- al., 2012), being responsible for ∼ 30 % of O3 loss in the tween size fractions and with the extent to which the samples marine boundary layer (MBL) (Prados-Roman et al., 2015). were influenced by pollutants. In general, fine mode aerosols Oceanic emission, principally of volatile I2 and hypoiodous (< 1 µm) contained higher proportions of both iodide and acid (HOI) formed through the reaction of O3 with iodide − SOI, while iodate was the dominant component of coarse (I ) at the sea surface (Carpenter et al., 2013), is the main (< 1 µm) aerosols.