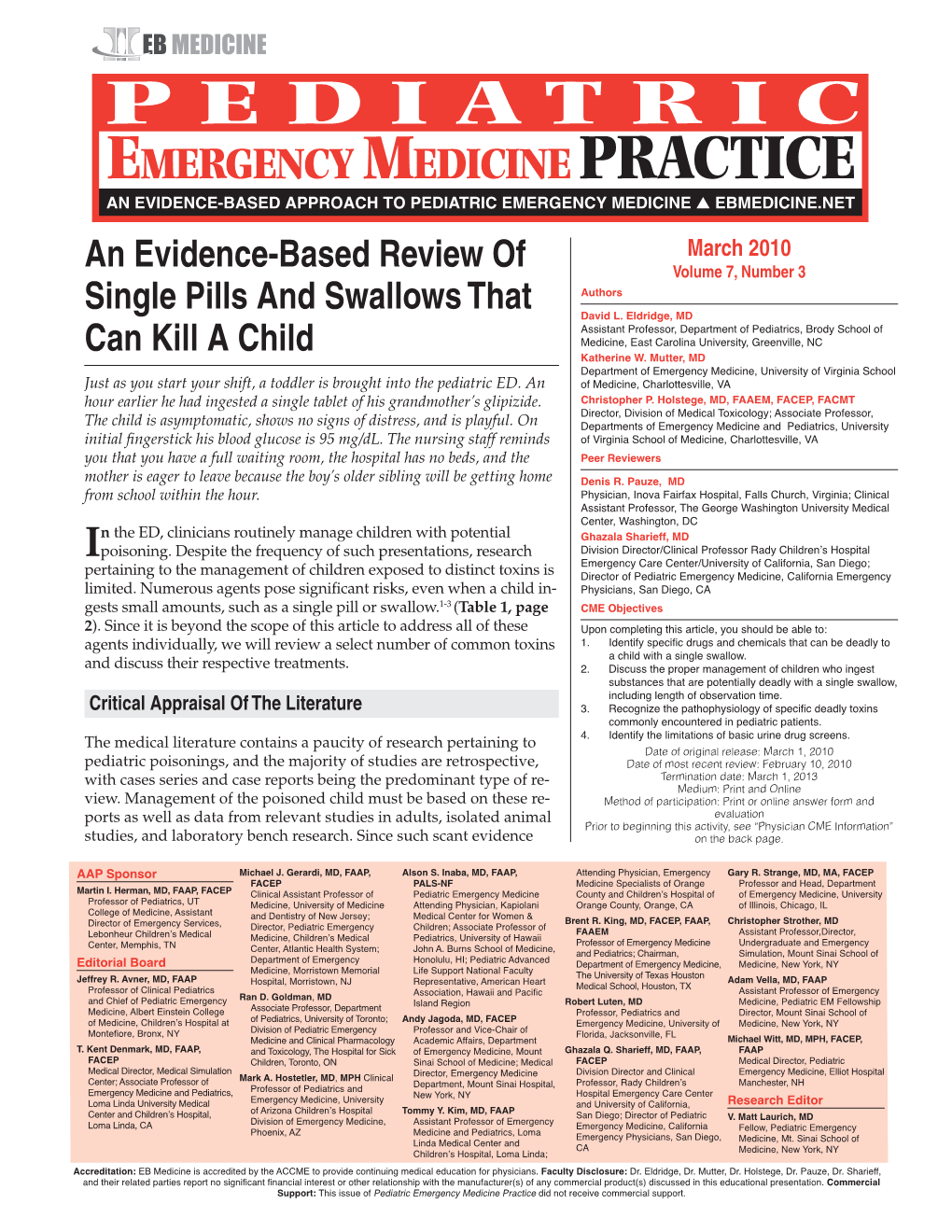
Single Pills That Kill
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
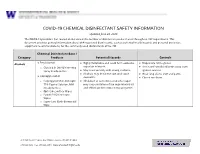
EH&S COVID-19 Chemical Disinfectant Safety Information
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -

Drug Safety Oversight Board Members
April 29, 2021 Drug Safety Oversight Board (DSOB) Roster Chair • Douglas Throckmorton, M.D., Deputy Director for Regulatory Programs Center for Drug Evaluation and Research Executive Director • Terry Toigo, R.Ph, MBA Associate Director for Drug Safety Operations, Center for Drug Evaluation and Research Food and Drug Administration Center for Drug Evaluation and Research (CDER) Office of the Center Director (OCD) Primary Member: • Robert Temple, M.D., Deputy Director for Clinical Science Office of New Drugs (OND) Primary Member: • Mary Thanh Hai, M.D., Deputy Director, Office of New Drugs Alternate Members: • Peter Stein, M.D., Director, Office of New Drugs • Ellis Unger, M.D., Director, Office of Office of Cardiology, Hematology, Endocrinology, and Nephrology (OCHEN) Office of Medical Policy (OMP) Primary Member: • Jacqueline Corrigan-Curay, Director Alternate Member: • Leonard V. Sacks, Mgr. Supervisory Medical Officer Office of Generic Drugs (OGD) Primary Member: • Linda Forsyth, M.D., Division of Clinical Review Alternate Member: • Vacant Office of Surveillance and Epidemiology (OSE) Primary Members: • Mark I. Avigan, M.D., Associate Director for Critical Path Initiatives • Judy Zander, M.D., Director, Office of Pharmacoviligance and Epidemiology (OPE) Alternate Members: • Gerald DalPan, M.D., M.H.S., Director, OSE • S. Chris Jones, Deputy Director, Division of Pharmacovigilance (DPV) II • Judy Staffa, Ph.D., R.Ph., Associate Director for Public Health Initiatives -Page 1 of 4- April 29, 2021 • Cynthia LaCivita, R.Ph, Director, Division -

CHEMICALS of PUBLIC HEALTH CONCERN and Their Management in the African Region
H H C Hg H N C OH O O HO OH OH CHEMICALS OF PUBLIC HEALTH CONCERN and their management in the African Region REGIONAL ASSESSMENT REPORT 4 JULY 2014 AFRO LIBRARY CATALOGUING-IN-PUBLICATION DATA Chemicals of public health concern in the African Region and their management: Regional Assessment Report 1. Chemically-Induced Disorders – prevention & control 2. Environmental Exposure 3. Polluants environnemental – adverse effects – toxicity 4. Hazardous Substances 5. Risk Management 6. Health Impact Assessment I. World Health Organization. Regional Office for Africa II.Title ISBN: 978-929023281-0 (NLM Classification:QZ 59) © WHO REGIONAL OFFICE FOR AFRICA, 2014 Publications of the World Health Organization enjoy The mention of specific companies or of certain copyright protection in accordance with the provisions manufacturers’ products does not imply that they of Protocol 2 of the Universal Copyright Convention. are endorsed or recommended by the World Health All rights reserved. Copies of this publication may be Organization in preference to others of a similar nature obtained from the Library, WHO Regional Office for that are not mentioned. Errors and omissions excepted, Africa, P.O. Box 6, Brazzaville, Republic of Congo (Tel: the names of proprietary products are distinguished by +47 241 39100; +242 06 5081114; Fax: +47 241 initial capital letters. 39501; E-mail: [email protected]). Requests for permission to reproduce or translate this publication All reasonable precautions have been taken by the – whether for sale or for non-commercial distribution – World Health Organization to verify the information should be sent to the same address. contained in this publication. -

Activated Charcoal for Acute Poisoning: One Toxicologist's Journey
J. Med. Toxicol. (2010) 6:190–198 DOI 10.1007/s13181-010-0046-1 REVIEW ARTICLE Activated Charcoal for Acute Poisoning: One Toxicologist’s Journey Kent R. Olson Published online: 20 May 2010 # The Author(s) 2010. This article is published with open access at Springerlink.com Keywords Activated charcoal . Gastrointestinal As summarized by Matthew [13], Harstad and Danish decontamination . Poisoning . Drug overdose colleagues reported in 1942 that relatively little phenobar- bital was recovered by lavage even shortly after overdose [14] and this, along with their finding of particles of When I began studying clinical toxicology in 1981, the issue charcoal in the lungs of patients who died, led them to call of gastrointestinal decontamination after acute ingestion for the abandonment of gastric lavage for poisoning.) “ ” seemed pretty well settled: universal antidote, apomor- In recent years, my colleagues and I have continued to – phine and salt wateremesiswerenolongerused[1, 2]; and I debate the value of various methods of gastric decontam- was taught that barring a specific contraindication, the awake ination and the role and risks of activated charcoal, and it is patient was given syrup of ipecac to induce emesis, and the clear to me that the issue remains muddy. Some have taken drowsy or uncooperative patient was lavaged [3]. After a firm stand that no treatment should be recommended that is gastric emptying, everyone received activated charcoal not supported by evidence from a randomized controlled trial (AC). The only controversy seemed to be over whether one (RCT). Position statements published jointly by the Amer- should add a cathartic to speed gastrointestinal transit [4]. -

Medical Toxicology Milestone Project
The Medical Toxicology Milestone Project A Joint Initiative of The Accreditation Council for Graduate Medical Education and The American Board of Emergency Medicine July 2015 The Medical Toxicology Milestone Project The Milestones are designed only for use in evaluation of the fellow in the context of their participation in ACGME-accredited residency or fellowship programs. The Milestones provide a framework for assessment of the development of the fellow in key dimensions of the elements of physician competency in a specialty or subspecialty. They neither represent the entirety of the dimensions of the six domains of physician competency, nor are they designed to be relevant in any other context. i Medical Toxicology Milestones Chair: Susanne White, MD Working Group Advisory Group Michele M. Burns, MD, MPH Timothy Brigham, MDiv, PhD Beth Baker, MD Wallace Carter, MD Laura Edgar, EdD, CAE William W. Greaves, MD, MSPH Lewis Nelson, MD Robert Johnson, MD Louis Ling, MD Earl Reisdorff, MD ii Milestone Reporting This document presents milestones designed for programs to use in semi-annual review of fellow performance and reporting to the ACGME. Milestones are knowledge, skills, attitudes, and other attributes for each of the ACGME competencies organized in a developmental framework from less to more advanced. They are descriptors and targets for fellow performance as a fellow moves from entry into fellowship through graduation. In the initial years of implementation, the Review Committee will examine milestone performance data for each program’s fellows as one element in the Next Accreditation System (NAS) to determine whether fellows overall are progressing. For each period, review and reporting will involve selecting milestone levels that best describe a fellow’s current performance and attributes. -

Treatment of Self-Poisoned Adults G
Archives of Emergency Medicine, 1985, 2, 203-208 Ipecacuanha induced emesis in the treatment of self-poisoned adults G. GORDON Accident and Emergency Department, Manor Hospital, Nuneaton, Warwickshire, England SUMMARY One hundred consecutive adult patients presenting to an Accident and Emergency Department following intentional self-poisoning were given 50 to 80 ml Paediatric Ipecacuanha Emetic Mixture BP as an emetic, together with two or three glasses of strong orange juice. A satisfactory emetic result was obtained in 99 patients. No toxic effects were noted in these patients, or in the one patient in whom emesis did not occur, and who subsequently refused gastric lavage. The potential toxicity of Ipecacuanha Syrup itself is discussed, and attention drawn to the lower Emetine content of Paediatric Ipecacuanha Emetic Mixture (BP), rather than that of the formulations used in previously published reports. The use of Paediatric Ipecacuanha Emetic Mixture B.P. in adults is effective and safe in this dosage. INTRODUCTION The methods available for retrieval of poisoning agents from the stomach are gastric lavage and emesis. In the United Kingdom at the present time, gastric lavage is the method most commonly used in the treatment of adults. It is an unpleasant and time consuming procedure for both patient and staff, and it is not without risk (Matthew et al., 1966), even in the hands of the experienced nursing staff who usually carry it out. Doubt still remains about its effectiveness (Goulding & Volans, 1977), and the basis for its use rests more on the occasional recovery of large quantities of drug, rather than verification of its routine efficiency by studies in man (Melman & Morelli, 1978). -

Effect of Vitamin D on Chronic Behavioral and Dental Toxicities of Sodium Fluoride in Rats
Fluoride Vol. 36 No. 3 189-197 2003 Research Report 189 EFFECT OF VITAMIN D ON CHRONIC BEHAVIORAL AND DENTAL TOXICITIES OF SODIUM FLUORIDE IN RATS Perumal Ekambaram,a Vanaja Paulb Chennai (Madras), India SUMMARY: Adult female Wistar rats were treated daily for 60 days with so- dium fluoride (500 ppm NaF = 226 ppm fluoride ion) in drinking water, alone or in combination with vitamin D (200 IU/kg by oral intubation). Throughout the period, food intake was measured daily. Body weight gain, exploratory motor activity (EMA) rota-rod motor coordination, dental structure, brain acetylcho- linesterase (AchE) activity, and serum fluoride and serum calcium concentra- tion were determined 24 hr after the last treatment. Serum fluoride concentra- tion increased markedly in the NaF-treated animals and was accompanied by decreased food intake, reduced body weight gain, impairment of EMA and motor coordination, dental lesions, inhibition of brain AchE activity, and hy- pocalcemia. Administration of vitamin D along with NaF prevented hypocal- cemia. However, the toxic action fluoride on motor coordination, brain AchE activity, and the teeth was not prevented in these animals, probably because vitamin D is not able to decrease the level of fluoride in the serum. Therefore, vitamin D has only limited value as a protective dietary factor against chronic toxic effects of fluoride. Keywords: Dental lesions; Fluoride toxicity; Locomotor behavior; Rat toxicity; Serum calcium; Serum fluoride; Vitamin D. INTRODUCTION Fluorides are naturally occurring contaminants in the environment.1 Pro- longed ingestion of drinking water containing 1–3 ppm of fluoride ion pro- duces deleterious effects on skeletal, dental,1 and soft tissues,2,3 enzyme ac- tivities,4 and locomotor behavior5 in animals. -
I Need Your Feedback & Ideas!
Greetings Everyone, Included is the Weekly Pile of Information for the week of May 17, 2015, Extension's Equine related educational information & announcements for Rockingham & Guilford Counties. To have something included in the Weekly Pile, please follow these simple guidelines. Information included needs to be educational in nature &/or directly related to Rockingham or Guilford Counties. provided information is a resource to the citizens of Rockingham/Guilford Counties. provided information does not require extra time or effort to be listed. Listings for Swap Shop will not list pricing details. Please Email information to me by Wednesday each Week. Please keep ads or events as short as possible – with NO FORMATTING, NO unnecessary Capitalization’s and NO ATTACHED DOCUMENTS. (If sent in that way, it may not be included) Please include contact information Phone, Email and alike. PLEASE PUT WEEKLY PILE IN SUBJECT LINE when you send into me. The Weekly Pile is not for listings for Commercial type properties or products. If I forgot to include anything in this email it was probably an oversight on my part, but please let me know! If you have a question or ideas that you would like covered in the Weekly Pile, please let me know and I will try to include. As Always, I would like to hear your comments about the Weekly Pile or the Extension Horse Program in Rockingham or Guilford Counties! I NEED YOUR FEEDBACK & IDEAS! Included in The Pile this Week: 1. TICKS, TICKS TICKS Its All About TICKS Program May 27th 7pm 2. Grazing Management 3. -

Expert Consensus Guidelines for Stocking of Antidotes in Hospitals That Provide Emergency Care
TOXICOLOGY/CONCEPTS Expert Consensus Guidelines for Stocking of Antidotes in Hospitals That Provide Emergency Care Richard C. Dart, MD, PhD From the Rocky Mountain Poison & Drug Center - Denver Health, Denver, CO (Dart, Heard, Schaeffer, Stephen W. Borron, MD, MS Bogdan, Alhelail, Buchanan, Hoppe, Lavonas, Mlynarchek, Phua, Rhyee, Varney, Zosel); Department of E. Martin Caravati, MD, MPH Surgery, University of Texas Health Sciences Center, San Antonio, TX (Borron); Division of Emergency Daniel J. Cobaugh, PharmD Medicine, Utah Poison Control Center, University of Utah Health Sciences Center, Salt Lake City, UT Steven C. Curry, MD (Caravati); ASHP Research and Education Foundation, Bethesda, MD (Cobaugh); Department of Jay L. Falk, MD Medical Toxicology and Banner Poison Control Center, Banner Good Samaritan Medical Center, Lewis Goldfrank, MD Phoenix, AZ (Curry); Department of Emergency Medicine, Orlando Regional Medical Center, University of Susan E. Gorman, PharmD, MS Florida, Orlando, FL (Falk); New York City Poison Center; New York University School of Medicine, New Stephen Groft, PharmD York, NY (Goldfrank); Division of Strategic National Stockpile, Centers for Disease Control and Kennon Heard, MD Prevention, Atlanta, GA (Gorman); Office of Rare Diseases Research, Bethesda, MD (Groft); Division of Ken Miller, MD, PhD Emergency Medicine, School of Medicine (Dart, Heard, Lavonas, Schaeffer) and Department of Kent R. Olson, MD Pharmaceutical Sciences, School of Pharmacy (Bogdan), University of Colorado Denver, Aurora, CO; Gerald O’Malley, DO Orange County Fire Authority and Orange County Health Care Agency Emergency Medical Services, Donna Seger, MD Irvine, CA, and National Association of EMS Physicians, Lenexa, KS, (Miller); University of California, Steven A. Seifert, MD San Francisco, and San Francisco Division, California Poison Control System, San Francisco, CA Marco L. -

Detoxification of Lignocellulose-Derived Microbial Inhibitory Compounds by Clostridium Beijerinckii NCIMB 8052 During Acetone-Butanol-Ethanol Fermentation
Detoxification of Lignocellulose-derived Microbial Inhibitory Compounds by Clostridium beijerinckii NCIMB 8052 during Acetone-Butanol-Ethanol Fermentation DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Yan Zhang Graduate Program in Animal Sciences The Ohio State University 2013 Dissertation Committee: Thaddeus C. Ezeji, Advisor Steven C. Loerch Sandra G. Velleman Zhongtang Yu Venkat Gopalan Copyrighted by Yan Zhang 2013 Abstract Pretreatment and hydrolysis of lignocellulosic biomass to fermentable sugars generate a complex mixture of microbial inhibitors such as furan aldehydes (e.g., furfural), which at sublethal concentration in the fermentation medium can be tolerated or detoxified by acetone butanol ethanol (ABE)-producing Clostridium beijerinckii NCIMB 8052. The response of C. beijerinckii to furfural at the molecular level, however, has not been directly studied. Therefore, this study was to elucidate mechanism employed by C. beijerinckii to detoxify lignocellulose-derived microbial inhibitors and use this information to develop inhibitor-tolerant C. beijerinckii. Towards the long-term goal of developing inhibitor-tolerant Clostridium strains, the first objective was to evaluate ABE fermentation by C. beijerinckii using different proportions of Miscanthus giganteus hydrolysates as carbon source. Compared to the growth of C. beijerinckii in control medium, C. beijerinckii experienced different degrees of inhibition. The degree of inhibition was dose-dependent, and C. beijerinckii did not grow in P2 medium with greater than 25% (v/v) Miscanthus giganteus hydrolysates. To improve tolerance of C. beijerinckii to inhibitors, supplementation of P2 medium with undiluted (100%) Miscanthus giganteus hydrolysates with 4 g/L CaCO3 resulted in successful growth of and ABE production by C. -

Reactions of Alcohols & Ethers 1
REACTIONS OF ALCOHOLS & ETHERS 1. Combustion (Extreme Oxidation) alcohol + oxygen carbon dioxide + water 2 CH3CH2OH + 6 O2 4 CO2 + 6 H2O 2. Elimination (Dehydration) ° alcohol H 2 S O 4/ 1 0 0 C alkene + water H2SO4/100 ° C CH3CH2CH2OH CH3CH=CH2 + H2O 3. Condensation ° excess alcohol H 2 S O 4 / 1 4 0 C ether + water H2SO4/140 ° C 2 CH3CH2OH CH3CH2OCH2CH3 + H2O 4. Substitution Lucas Reagent alcohol + hydrogen halide Z n C l2 alkyl halide + water ZnCl2 CH3CH2OH + HCl CH3CH2Cl + H2O • This reaction with the Lucas Reagent (ZnCl2) is a qualitative test for the different types of alcohols because the rate of the reaction differs greatly for a primary, secondary and tertiary alcohol. • The difference in rates is due to the solubility of the resulting alkyl halides • Tertiary Alcohol→ turns cloudy immediately (the alkyl halide is not soluble in water and precipitates out) • Secondary Alcohol → turns cloudy after 5 minutes • Primary Alcohol → takes much longer than 5 minutes to turn cloudy 5. Oxidation • Uses an oxidizing agent such as potassium permanganate (KMnO4) or potassium dichromate (K2Cr2O7). • This reaction can also be used as a qualitative test for the different types of alcohols because there is a distinct colour change. dichromate → chromium 3+ (orange) → (green) permanganate → manganese (IV) oxide (purple) → (brown) Tertiary Alcohol not oxidized under normal conditions CH3 KMnO4 H3C C OH NO REACTION K2Cr2O7 CH3 tertbutyl alcohol Secondary Alcohol ketone + hydrogen ions H O KMnO4 H3C C CH3 + K2Cr2O7 C + 2 H H3C CH3 OH propanone 2-propanol Primary Alcohol aldehyde + water carboxylic acid + hydrogen ions O KMnO4 O H H KMnO H H 4 + CH3CH2CH2OH C C C H C C C H + 2 H K2Cr2O7 + H2O K Cr O H H H 2 2 7 HO H H 1-propanol propanal propanoic acid 6. -

Poison/Drug Emergencies 1. Which Alcohol Is Used As an Antidote For
Student ID: 22195894 Exam: 084084RR - Poison/Drug Emergencies When you have completed your exam and reviewed your answers, click Submit Exam. Answers will not be recorded until you hit Submit Exam. If you need to exit before completing the exam, click Cancel Exam. Questions 1 to 20: Select the best answer to each question. Note that a question and its answers may be split across a page break, so be sure that you have seen the entire question and all the answers before choosing an answer. 1. Which alcohol is used as an antidote for ethylene glycol ingestions? A. Ethanol B. Isopropanol C. Methanol D. Tetradecanol 2. Which of the following statements about syrup of ipecac is not correct? A. Ipecac stimulates the area in the brain responsible for nausea and vomiting. B. Ipecac has a local irritant effect on the stomach. C. Ipecac should be used to induce vomiting in all patients, regardless of age or condition. D. Ipecac contains two active substances, emetine and cephaeline. 3. The odor of wintergreen on a child's breath might indicate ingestion of which chemical? A. Sodium hypochlorite B. Toluene C. Methyl salicylate D. Paradichlorobenzene 4. _______ is used to reverse an opiate (such as morphine or codeine) overdose. A. Flumazenil B. Atropine C. Naloxone D. Deferoxamine 5. Which of the following statements about syrup of ipecac is not correct? A. American poison control centers rarely recommend syrup of ipecac as an intervention. B. The side effects of ipecac ingestion include prolonged vomiting and lethargy. C. Syrup of ipecac has been available for years in pharmacies over-the-counter.