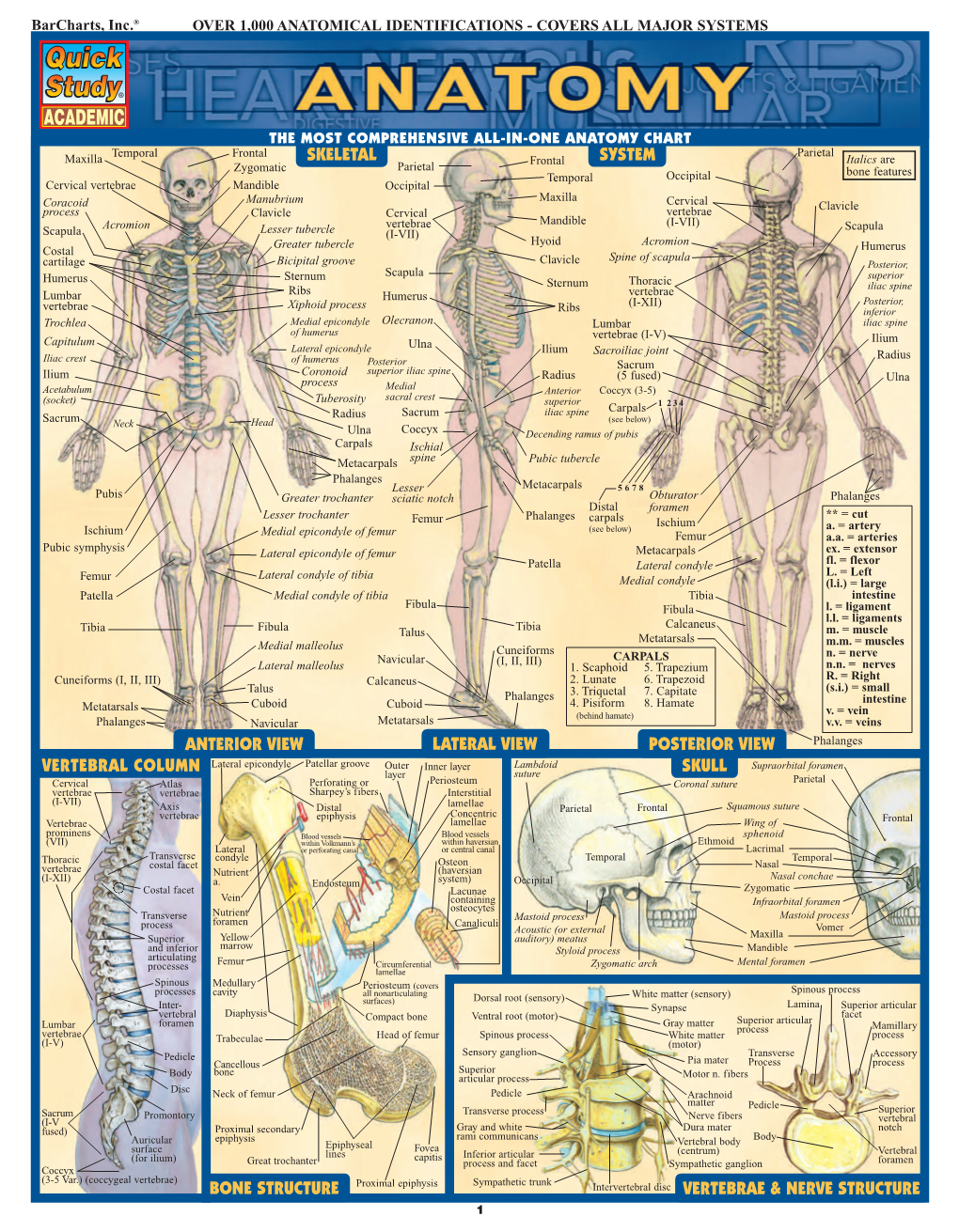
Barcharts Quickstudy Anatomy Vol 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

List: Bones & Bone Markings of Appendicular Skeleton and Knee
List: Bones & Bone markings of Appendicular skeleton and Knee joint Lab: Handout 4 Superior Appendicular Skeleton I. Clavicle (Left or Right?) A. Acromial End B. Conoid Tubercle C. Shaft D. Sternal End II. Scapula (Left or Right?) A. Superior border (superior margin) B. Medial border (vertebral margin) C. Lateral border (axillary margin) D. Scapular notch (suprascapular notch) E. Acromion Process F. Coracoid Process G. Glenoid Fossa (cavity) H. Infraglenoid tubercle I. Subscapular fossa J. Superior & Inferior Angle K. Scapular Spine L. Supraspinous Fossa M. Infraspinous Fossa III. Humerus (Left or Right?) A. Head of Humerus B. Anatomical Neck C. Surgical Neck D. Greater Tubercle E. Lesser Tubercle F. Intertubercular fossa (bicipital groove) G. Deltoid Tuberosity H. Radial Groove (groove for radial nerve) I. Lateral Epicondyle J. Medial Epicondyle K. Radial Fossa L. Coronoid Fossa M. Capitulum N. Trochlea O. Olecranon Fossa IV. Radius (Left or Right?) A. Head of Radius B. Neck C. Radial Tuberosity D. Styloid Process of radius E. Ulnar Notch of radius V. Ulna (Left or Right?) A. Olecranon Process B. Coronoid Process of ulna C. Trochlear Notch of ulna Human Anatomy List: Bones & Bone markings of Appendicular skeleton and Knee joint Lab: Handout 4 D. Radial Notch of ulna E. Head of Ulna F. Styloid Process VI. Carpals (8) A. Proximal row (4): Scaphoid, Lunate, Triquetrum, Pisiform B. Distal row (4): Trapezium, Trapezoid, Capitate, Hamate VII. Metacarpals: Numbered 1-5 A. Base B. Shaft C. Head VIII. Phalanges A. Proximal Phalanx B. Middle Phalanx C. Distal Phalanx ============================================================================= Inferior Appendicular Skeleton IX. Os Coxae (Innominate bone) (Left or Right?) A. -

PTA019: Anatomy & Physiology Manual
Anatomy & Physiology Full content for both the Level 2 Certificate in Fitness Instructing & Level 3 Certificate in Personal Training LEARN - INSPIRE - SUCCEED Contents Anatomy & Physiology for Exercise ………………………………………. Page 3 • The Musculoskeletal System ………………………………………. Page 3 • Energy Systems ………………………………………. Page 76 • The Cardiorespiratory System ………………………………………. Page 86 • The Neuroendocrine System ………………………………………. Page 105 Performance Training Academy 2 Chapter Two: Anatomy and Physiology Introduction This chapter is to be broken down into many sub-chapters, giving you a great reference point for your study as well as when needed once you are actively working as a Fitness Professional. It is of upmost importance that you continue to recap and learn further about the bio-mechanics and workings of the human body. A great fitness professional won’t just know how to programme for an individual, but will know how to help improve weaknesses and imbalances within the body, knowledge of Anatomy and Physiology is key to be able to do this. The Musculoskeletal System Unit Objectives Our first objective is to understand the biomechanics of the human body. We can do this by learning about the skeletal system, and then how the muscles are layered upon the skeleton. By the end of this unit we want you to have a good subject knowledge of the following: • The main bones of the skeleton • Joint types and joint actions • How exercise can create a strong and healthy skeletal system • The main muscles of the body • Muscle contractions and fibre types We will start by going through the skeletal system before bringing the muscles into the equation. This will allow you to build up your knowledge of bones and terminology before recapping them again by layering the muscles across specific joints. -

General Introduction of Anatomy
ﺍﳌﻌﻬﺪ ﺍﻟﻄﺒﻲ ﺍﻟﺘﻘﻨﻲ / ﺑﻐﺪﺍﺩ ﻗﺴﻢ ﺍﻟﺘﺄﻫﻴﻞ ﺍﻟﻄﺒﻲ ﻭﺍﻟﻌﻼﺝ ﺍﻟﻄﺒﻴﻌﻲ ﻓﺮﻉ ﺻﻨﺎﻋﺔ ﺍﻻﻃﺮﺍﻑ ﻭﺍﳌﺴﺎﻧﺪ General introduction of Anatomy 2013 – 2014 Dr. ASHRAF Ali AL-ZUBAIDI Dr. ASHRAF Ali AL-ZUBAIDI 2013-2014 1 GENERAL INTRODUCTION Anatomy: is the science of body structures and the relationships among Structures. At first the anatomy was studied by dissection, the carful cutting apart of body structures to study their relationships, Nowadays, many imaging of anatomical (ﺗﻘﺪم) to the advancement (ﺗﺴﺎھﻢ) techniques also contribute knowledge. The Anatomy is including many of fields, which is: It is the study of different : (اﻟﻔﺤﺺ اﻟﻌﯿﻨﻲ ) Macroscopic examination 1- structures , which make up the human body . It is the study of : (اﻟﻔﺤﺺ اﻟﻤﺠﮭﺮي ) Microscopic examination 2- seen (اﻟﻜﺎﺋﻦ اﻟﺤﻲ ) microscopic different structures of an organism only by use of a microscope . It is the study of different structures as : (اﻻﺟﮭﺰة اﻟﺠﺴﻤﯿﺔ) Systemic 3- : It comprises of the followings . (ﻛﻜﯿﺎﻧﺎت ﻓﺮدﯾﺔ) individual entities .The bony system \ ( ﻋﻠﻢ اﻟﻌﻈﺎم ) Osteology • . The articular system or joint \(ﻋﻠﻢ اﻟﻤﻔﺎﺻﻞ ) Syndesmology • . The muscular system \ (ﻋﻠﻢ الﻋﻀﻼت )Myology • , Comprising the heart , blood vessels \ (ﻋﻠﻢ اﻻوﻋﯿﺔ ) Angiology • ( اﻟﻌﻘﺪ اﻟﻠﻤﻔﺎوﯾﺔ)lymph nodes & (اﻻوﻋﯿﺔ اﻟﻠﻤﻔﺎوﯾﺔ) lymph vessels .The nervous system \(ﻋﻠﻢ اﻟﺠﮭﺎز اﻟﻌﺼﺒﻲ) Neurology • , ( اﻟﻨﻈﺎم اﻟﺤﺸﻮي ) The visceral system \ (ﻋﻠﻢ اﻻﺣﺸﺎء) Splanchnology • , (ﻧﻈﺎم اﻧﺒﻮﺑﻲ – ھﻀﻤﻲ ) comprising two tubular system – digestive . (اﻟﺠﮭﺎز اﻟﺘﻨﺎﺳﻠﻲ) and genital (اﻟﺠﮭﺎز اﻟﺒﻮﻟﻲ) urinary tract The study of form and marking of those :(اﻟﺘﺸﺮﯾﺢ اﻟﺴﻄﺤﻲ) Surface 4- structures by examination through skin. .It is the study of development before birth :(ﻋﻠﻢ اﻻﺟﻨﺔ) Embryology 5- GLOSSARY OF ANATOMIC TERMINOLOGY description of location (ﯾﺴﻤﺢ) Reference position of body permitting and movements: 1- Term of Anatomical position: • Head ………. -
Scapular Dyskinesis
Scapular Dyskinesis Presented by: Scott Sevinsky MSPT Presented by: Scott Sevinsky SPT 1 What is Scapular Dyskinesis? Alteration in the normal static or dynamic position or motion of the scapula during coupled scapulohumeral movements. Other names given to this catch-all phrase include: “floating scapula” and “lateral scapular slide”.1, 2 1 Alterations in scapular position and motion occur in 68 – 100% of patients with shoulder injuries. Scapular Dyskinesis Classification System 1, 3 Pattern Definitions Inferior angle At rest, the inferior medial scapular border may be prominent dorsally. During arm motion, the inferior (type I) angle tilts dorsally and the acromion tilts ventrally over the top of the thorax. The axis of the rotation is in the horizontal plane. Medial border At rest, the entire medial border may be prominent dorsally. During arm motion, the medial scapular (type II) border tilts dorsally off the thorax. The axis of the rotation is vertical in the frontal plane. Superior border At rest, the superior border of the scapula may be elevated and the scapula can also be anteriorly (type III) displaced. During arm motion, a shoulder shrug initiates movement without significant winging of the scapula occurring. The axis of this motion occurs in the sagittal plane. Symmetric At rest, the position of both scapula are relatively symmetrical, taking into account that the dominant scapulohumeral arm may be slightly lower. During arm motion, the scapulae rotate symmetrically upward such that the (type IV) inferior angles translate laterally away from the midline and the scapular medial border remains flush against the thoracic wall. The reverse occurs during lowering of the arm. -

Bone Limb Upper
Shoulder Pectoral girdle (shoulder girdle) Scapula Acromioclavicular joint proximal end of Humerus Clavicle Sternoclavicular joint Bone: Upper limb - 1 Scapula Coracoid proc. 3 angles Superior Inferior Lateral 3 borders Lateral angle Medial Lateral Superior 2 surfaces 3 processes Posterior view: Acromion Right Scapula Spine Coracoid Bone: Upper limb - 2 Scapula 2 surfaces: Costal (Anterior), Posterior Posterior view: Costal (Anterior) view: Right Scapula Right Scapula Bone: Upper limb - 3 Scapula Glenoid cavity: Glenohumeral joint Lateral view: Infraglenoid tubercle Right Scapula Supraglenoid tubercle posterior anterior Bone: Upper limb - 4 Scapula Supraglenoid tubercle: long head of biceps Anterior view: brachii Right Scapula Bone: Upper limb - 5 Scapula Infraglenoid tubercle: long head of triceps brachii Anterior view: Right Scapula (with biceps brachii removed) Bone: Upper limb - 6 Posterior surface of Scapula, Right Acromion; Spine; Spinoglenoid notch Suprspinatous fossa, Infraspinatous fossa Bone: Upper limb - 7 Costal (Anterior) surface of Scapula, Right Subscapular fossa: Shallow concave surface for subscapularis Bone: Upper limb - 8 Superior border Coracoid process Suprascapular notch Suprascapular nerve Posterior view: Right Scapula Bone: Upper limb - 9 Acromial Clavicle end Sternal end S-shaped Acromial end: smaller, oval facet Sternal end: larger,quadrangular facet, with manubrium, 1st rib Conoid tubercle Trapezoid line Right Clavicle Bone: Upper limb - 10 Clavicle Conoid tubercle: inferior -

Geometric Variations in Load-Bearing Joints
University of Alberta Geometric Variations in Load-Bearing Joints by Kamrul Islam A thesis submitted to the Faculty of Graduate Studies and Research in partial fulfillment of the requirements for the degree of Master of Science in Structural Engineering Department of Civil and Environmental Engineering ©Kamrul Islam Fall 2012 Edmonton, Alberta Permission is hereby granted to the University of Alberta Libraries to reproduce single copies of this thesis and to lend or sell such copies for private, scholarly or scientific research purposes only. Where the thesis is converted to, or otherwise made available in digital form, the University of Alberta will advise potential users of the thesis of these terms. The author reserves all other publication and other rights in association with the copyright in the thesis and, except as herein before provided, neither the thesis nor any substantial portion thereof may be printed or otherwise reproduced in any material form whatsoever without the author's prior written permission. Dedication Dedicated to my dad, A.F.M. Shamsul Islam, my mom, Shahina Akhter Chowdhury, and my brother, Nazmul Islam Abstract The purpose of the current study was to investigate the geometric variations in the load-bearing joints among individuals. Two existing concepts in mathematics were introduced and their application in computational biomechanics was completely novel: 1) computing the depth of penetration between contact objects as an indirect measure of stress; and 2) computing the geometric similarity using the cubic root of volumetric ratio as a scaling law. Furthermore, an alternative geometric method to finite element analysis was proposed, which should be considered as a “proof of concept”. -

Masaryk University Faculty of Medicine REHABILITATION IN
Masaryk University Faculty of Medicine REHABILITATION IN PATIENTS AFTER TOTAL KNEE ARTHROPLASTY Bachelor´s Thesis Physiotherapy Bachelor’s Thesis Supervisor: Author: Mgr. Veronika Mrkvicová Josh Tilrem Brno, 2018 Name and Surname of the Author: Josh Tilrem Title of Bachelor’s thesis: Rehabilitation in patients after total knee arthroplasty Název bakalářské práce: Rehabilitace u pacientů po totální endoprotéze kolenního kloubu Department: Department of Rehabilitation and Physiotherapy MF MU Supervisor: Mgr. Veronika Mrkvicová Year of the Bachelor’s thesis defence: 2018 Summary: This Bachelor’s thesis is composed of two parts. The first part deals with the subject of total knee arthroplasty. The aim of this part is to describe the indication, surgical procedure and treatment, both in acute and long-term phase. The first part also contains the approach and management of the physical therapist and how to utilize proper rehabilitation. The second part is a case study and the aim is to describe the practical procedure of a specific rehabilitation after total knee arthroplasty. This include examination at admittance, discharge and rehabilitation provided by the author. Souhrn: Tato bakalářská práce je složená ze dvou částí. Prní část pojednává o tématu totální endoprotézy kolenního kloubu. Cílem této části je popsat indikace, chirurgický přístup a léčbu, jak v akutní, tak chronické fázi. První část také zahrnuje fyzioterapetické postupy a provádění léčebné rehabilitace. Druhá část obsahuje kazuistiku a jejím cílem je přiblížit praktické postupy speciální rehabilitace po totální endoprotéze kolenního kloubu. To zahrnuje vstupní a výstupní vyšetření a rehabilitaci prováděnou autorem. Keywords: Total knee arthroplasty, rehabilitation, physiotherapy Klíčová slova: Totální endoprotéza kolenního kloubu, rehabilitace, fyzioterapie I agree that this bachelor thesis will be archived in the Masaryk University of Brno library and will be quoted according to citations norms. -

The Painful Shoulder Part II: Common Acute & Chronic Disorders
The Painful Shoulder Part II: Common Acute & Chronic Disorders © Jackson Orthopaedic Foundation www.jacksonortho.org Presenters AJ Benham, DNP, FNP, ONC Kathleen Geier, DNP, FNP, ONC Jackson Orthopedic Foundation 3317 Elm Street - Suite 102 Oakland, CA 94609 [email protected] [email protected] http://www.orthoprimarycare.info/ Conflict Of Interest Disclosures We hereby certify that, to the best of our knowledge, no aspect of our current personal or professional situation might reasonably be expected to affect significantly our views on the subject on which we are presenting. Objectives • 1. Differentiate among common conditions associated with shoulder pain based on history and physical exam • 2. Formulate plans for imaging and treatment of specific shoulder conditions according to evidence based guidelines. • 3. Discuss indications & appropriate communication techniques for referral of patients with shoulder conditions to services including PT, surgery, etc. Common Sites of Shoulder Pain A A good place for a chart ACUTE CHRONIC • Fractures • Impingement Syndrome Humerus • Frozen Shoulder Clavicle Adhesive capsulitis Scapula • Biceps Tendonitis • *Dislocations • Labral Injury Humerus SLAP Tear AC Joint • Osteoarthritis SC Joint Glenohumeral • *Rotator Cuff Tear Acromioclavicular S.I.T.S. Muscles • Osteolysis Distal clavicle Shoulder Landmarks A A good place for a chart More Shoulder Landmarks A A good place for a chart Musculoskeletal Exam • Inspection • Palpation * • Range of Motion • Resisted Strength • Sensation • Provocative Testing * One joint above; one below www.jacksonortho.org ACUTE CHRONIC • Fractures • Impingement Syndrome Clavicle • Frozen Shoulder Humerus Adhesive capsulitis Scapula • Biceps Tendonitis • *Dislocations • Labral Injury Humerus SLAP Tear AC Joint • Osteoarthritis SC Joint Glenohumeral • *Rotator Cuff Tear Acromioclavicular S.I.T.S. -

Bones of the Skeletal System
BIOLOGY 211: HUMAN ANATOMY & PHYSIOLOGY ********************************************************************************************************* BONES OF THE SKELETAL SYSTEM ********************************************************************************************************** Reference: Saladin, KS: Anatomy & Physiology, The Unity of Form and Function, 6th ed. (2012) or 7th ed. (2015) Please review Chapters 7 & 8 before beginning this lab. INTRODUCTION The skeletal system has a number of important functions in the human body. It is the framework around which the body is organized, it provides levers for muscles to pull against, and it surrounds and protects many soft organs. Equally important, bones serve as a "buffer" in which calcium and other ions can be deposited and withdrawn according to the changing needs of the body, and they are the site of almost all blood cell production. Contrary to our popular conceptions, bones are not rigid, inflexible structures: they are constantly changing, and can have a remarkable degree of flexibility before they break. The organs of the skeletal system are the bones and joints, and like all organs are composed of different types of tissue. Although we tend to classify them into "types" such as "long bones", "flat bones", etc., each is in fact unique and ideally suited to its particular location and function. We classify bones as belonging to either: a) the axial skeleton (head and trunk) b) the appendicular skeleton (arms and legs), However, you should always bear in mind that the entire skeletal system functions as a unit. If you look at any bone, you will see that it is rarely flat or smooth. Bones have a variety of bumps, grooves, holes, etc. which allow them to serve their specific functions. -

A Finite Element Model of a Realistic Foot and Ankle for Flatfoot Analysis
A Finite Element Model of a Realistic Foot and Ankle for Flatfoot Analysis Item Type text; Electronic Thesis Authors Williams, Lindsey Leigh Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 27/09/2021 13:32:56 Link to Item http://hdl.handle.net/10150/626145 A FINITE ELEMENT MODEL OF A REALISTIC FOOT AND ANKLE FOR FLATFOOT ANALYSIS by Lindsey Leigh Williams ___________________________ Copyright © Lindsey Leigh Williams 2017 A Thesis Submitted to the Faculty of the DEPARTMENT OF AEROSPACE AND MECHANICAL ENGINEERING In Partial Fulfillment of the Requirements For the Degree of MASTER OF SCIENCE WITH A MAJOR IN MECHANICAL ENGINEERING In the Graduate College THE UNIVERSITY OF ARIZONA 2017 STATEMENT BY AUTHOR The thesis titled A Finite Element Model of a Realistic Foot and Ankle for Flatfoot Analysis prepared by Lindsey Williams has been submitted in partial fulfillment of requirements for a master’s degree at the University of Arizona and is deposited in the University Library to be made available to borrowers under rules of the Library. Brief quotations from this thesis are allowable without special permission, provided that an accurate acknowledgement of the source is made. Requests for permission for extended quotation from or reproduction of this manuscript in whole or in part may be granted by the head of the major department or the Dean of the Graduate College when in his or her judgment the proposed use of the material is in the interests of scholarship. -

Anatomy and Physiology II
Anatomy and Physiology II Review Bones of the Upper Extremities Muscles of the Upper Extremities Anatomy and Physiology II Review Bones of the Upper Extremities Questions From Shoulder Girdle Lecture • Can you name the following structures? A – F • Acromion F – B B • Spine of the Scapula G – C • Medial (Vertebral) Border H – E C • Lateral (Axillary) Border – A • Superior Angle E I – D • Inferior Angle – G • Head of the Humerus D – H • Greater Tubercle of Humerus – I • Deltoid Tuberosity Questions From Shoulder Girdle Lecture • Would you be able to find the many of the same landmarks on this view (angles, borders, etc)? A • Can you name the following? – D • Coracoid process of scapula C – C D B • Lesser Tubercle – A • Greater Tubercle – B • Bicipital Groove (Intertubercular groove) Questions From Upper Extremities Lecture • Can you name the following structures? – B • Lateral epicondyle – A • Medial epicondyle A B Questions From Upper Extremities Lecture • Can you name the following landmarks? – C • Olecranon process – A • Head of the radius – B D • Medial epicondyle B A – D C • Lateral epicondyle Questions From Upper Extremities Lecture • Can you name the following bones and landmarks? – Which bone is A pointing to? • Ulna – Which bone is B pointing A to? • Radius E – C B • Styloid process of the ulna – D • Styloid process of the radius C – E D • Interosseous membrane of forearm Questions From Upper Extremities Lecture • Can you name the following bony landmarks? – Which landmark is A pointing to? • Lateral epicondyle of humerus – Which -

Biomechanical Efficacy of Four Different Dual Screws Fixations in Treatment
Fan et al. Journal of Orthopaedic Surgery and Research (2020) 15:45 https://doi.org/10.1186/s13018-020-1560-8 RESEARCH ARTICLE Open Access Biomechanical efficacy of four different dual screws fixations in treatment of talus neck fracture: a three-dimensional finite element analysis Zhengrui Fan1,2†, Jianxiong Ma1,2†, Jian Chen1,2, Baocheng Yang1,2, Ying Wang1,2, Haohao Bai1,2, Lei Sun1,2, Yan Wang1,2, Bin Lu1,2, Ben-chao Dong1,2, Aixian Tian1,2 and Xinlong Ma1,2,3* Abstract Background: Current there are different screws fixation methods used for fixation of the talar neck fracture. However, the best method of screws internal fixation is still controversial. Few relevant studies have focused on this issue, especially by finite element analysis. The purpose of this study was to explore the mechanical stability of dual screws internal fixation methods with different approaches and the best biomechanical environment of the fracture section, so as to provide reliable mechanical evidence for the selection of clinical internal fixation. Methods: The computed tomography (CT) image of the healthy adult male ankle joint was used for three- dimensional reconstruction of the ankle model. Talus neck fracture and screws were constructed by computer-aided design (CAD). Then, 3D model of talar neck fracture which fixed with antero-posterior (AP) parallel dual screws, antero-posterior (AP) cross dual screws, postero-anterior (PA) parallel dual screws, and postero-anterior (PA) cross dual screws were simulated. Finally, under the condition of 2400N vertical load, finite element analysis (FEA) were carried out to compare the outcome of the four different internal fixation methods.