Thawing the Development History of Artemisinin in Introduction To
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Cambridge's 92 Nobel Prize Winners Part 2 - 1951 to 1974: from Crick and Watson to Dorothy Hodgkin
Cambridge's 92 Nobel Prize winners part 2 - 1951 to 1974: from Crick and Watson to Dorothy Hodgkin By Cambridge News | Posted: January 18, 2016 By Adam Care The News has been rounding up all of Cambridge's 92 Nobel Laureates, celebrating over 100 years of scientific and social innovation. ADVERTISING In this installment we move from 1951 to 1974, a period which saw a host of dramatic breakthroughs, in biology, atomic science, the discovery of pulsars and theories of global trade. It's also a period which saw The Eagle pub come to national prominence and the appearance of the first female name in Cambridge University's long Nobel history. The Gender Pay Gap Sale! Shop Online to get 13.9% off From 8 - 11 March, get 13.9% off 1,000s of items, it highlights the pay gap between men & women in the UK. Shop the Gender Pay Gap Sale – now. Promoted by Oxfam 1. 1951 Ernest Walton, Trinity College: Nobel Prize in Physics, for using accelerated particles to study atomic nuclei 2. 1951 John Cockcroft, St John's / Churchill Colleges: Nobel Prize in Physics, for using accelerated particles to study atomic nuclei Walton and Cockcroft shared the 1951 physics prize after they famously 'split the atom' in Cambridge 1932, ushering in the nuclear age with their particle accelerator, the Cockcroft-Walton generator. In later years Walton returned to his native Ireland, as a fellow of Trinity College Dublin, while in 1951 Cockcroft became the first master of Churchill College, where he died 16 years later. 3. 1952 Archer Martin, Peterhouse: Nobel Prize in Chemistry, for developing partition chromatography 4. -

Peptide Chemistry up to Its Present State
Appendix In this Appendix biographical sketches are compiled of many scientists who have made notable contributions to the development of peptide chemistry up to its present state. We have tried to consider names mainly connected with important events during the earlier periods of peptide history, but could not include all authors mentioned in the text of this book. This is particularly true for the more recent decades when the number of peptide chemists and biologists increased to such an extent that their enumeration would have gone beyond the scope of this Appendix. 250 Appendix Plate 8. Emil Abderhalden (1877-1950), Photo Plate 9. S. Akabori Leopoldina, Halle J Plate 10. Ernst Bayer Plate 11. Karel Blaha (1926-1988) Appendix 251 Plate 12. Max Brenner Plate 13. Hans Brockmann (1903-1988) Plate 14. Victor Bruckner (1900- 1980) Plate 15. Pehr V. Edman (1916- 1977) 252 Appendix Plate 16. Lyman C. Craig (1906-1974) Plate 17. Vittorio Erspamer Plate 18. Joseph S. Fruton, Biochemist and Historian Appendix 253 Plate 19. Rolf Geiger (1923-1988) Plate 20. Wolfgang Konig Plate 21. Dorothy Hodgkins Plate. 22. Franz Hofmeister (1850-1922), (Fischer, biograph. Lexikon) 254 Appendix Plate 23. The picture shows the late Professor 1.E. Jorpes (r.j and Professor V. Mutt during their favorite pastime in the archipelago on the Baltic near Stockholm Plate 24. Ephraim Katchalski (Katzir) Plate 25. Abraham Patchornik Appendix 255 Plate 26. P.G. Katsoyannis Plate 27. George W. Kenner (1922-1978) Plate 28. Edger Lederer (1908- 1988) Plate 29. Hennann Leuchs (1879-1945) 256 Appendix Plate 30. Choh Hao Li (1913-1987) Plate 31. -

Crystal Vision Dorothy Hodgkin & the Nobel Prize “Few Were Her Equal in Generosity of Spirit, Breadth of Mind, Cultivated Humaneness, Or Gift for Giving
Crystal Vision Dorothy Hodgkin & the Nobel Prize “Few were her equal in generosity of spirit, breadth of mind, cultivated humaneness, or gift for giving. She should be remembered not only for a lifetime’s succession of brilliantly achieved structures. While those who knew her, experienced her quiet and modest and extremely powerful influence, learned from her more than the positioning of atoms in the three-dimensional molecule, she will be remembered not only with respect, and reverence, and gratitude, but more than anything else, with love. Let that be her lasting memorial.” Anne Sayre, in the Autumn 1995 Newsletter of the American Crystallographic Association Cover image © Emilio Segre Visual Archives/American Institute of Physics/Science Photo Library Letter from the Principal Dr Alice Prochaska, Somerville College Many remarkable woman scientists have passed through Somerville, but few rival Dorothy Hodgkin, whose path-breaking work in crystallography showed a mind not only attuned to high science but one also able to envision a crystal structure from the pattern made by its X-ray diffraction. Her ability to ‘see’ molecules such as cholesterol, penicillin, vitamin B and insulin transformed her field. 2014 sees the fiftieth anniversary of Professor Hodgkin’s Nobel prize. It is also the International Year of Crystallography, marking the 100th anniversary of Max von Laue’s Nobel Prize for Physics, awarded for his discovery that X-rays could be diffracted by crystals. That discovery underpinned Dorothy Hodgkin’s work. We are proud that Somerville supported her at a time when there was widespread opposition to married women pursuing academic careers. -
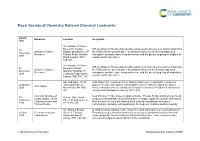
RSC Branding
Royal Society of Chemistry National Chemical Landmarks Award Honouree Location Inscription Date The Institute of Cancer Research, Chester ICR scientists on this site and elsewhere pioneered numerous new cancer drugs from 10 Institute of Cancer Beatty Laboratories, 237 the 1950s until the present day – including the discovery of chemotherapy drug December Research Fulham Road, Chelsea carboplatin, prostate cancer drug abiraterone and the genetic targeting of olaparib for 2018 Road, London, SW3 ovarian and breast cancer. 6JB, UK The Institute of Cancer ICR scientists on this site and elsewhere pioneered numerous new cancer drugs from 10 Research, Royal Institute of Cancer the 1950s until the present day – including the discovery of chemotherapy drug December Marsden Hospital, 15 Research carboplatin, prostate cancer drug abiraterone and the genetic targeting of olaparib for 2018 Cotswold Road, Sutton, ovarian and breast cancer. London, SM2 5NG, UK Ape and Apple, 28-30 John Dalton Street was opened in 1846 by Manchester Corporation in honour of 26 October John Dalton Street, famous chemist, John Dalton, who in Manchester in 1803 developed the Atomic John Dalton 2016 Manchester, M2 6HQ, Theory which became the foundation of modern chemistry. President of Manchester UK Literary and Philosophical Society 1816-1844. Chemical structure of Near this site in 1903, James Colquhoun Irvine, Thomas Purdie and their team found 30 College Gate, North simple sugars, James a way to understand the chemical structure of simple sugars like glucose and lactose. September Street, St Andrews, Fife, Colquhoun Irvine and Over the next 18 years this allowed them to lay the foundations of modern 2016 KY16 9AJ, UK Thomas Purdie carbohydrate chemistry, with implications for medicine, nutrition and biochemistry. -
Nobel Lectures™ 2001-2005
World Scientific Connecting Great Minds 逾10 0 种 诺贝尔奖得主著作 及 诺贝尔奖相关图书 我们非常荣幸得以出版超过100种诺贝尔奖得主著作 以及诺贝尔奖相关图书。 我们自1980年代开始与诺贝尔奖得主合作出版高品质 畅销书。一些得主担任我们的编辑顾问、丛书编辑, 并于我们期刊发表综述文章与学术论文。 世界科技与帝国理工学院出版社还邀得其中多位作了公 开演讲。 Philip W Anderson Sir Derek H R Barton Aage Niels Bohr Subrahmanyan Chandrasekhar Murray Gell-Mann Georges Charpak Nicolaas Bloembergen Baruch S Blumberg Hans A Bethe Aaron J Ciechanover Claude Steven Chu Cohen-Tannoudji Leon N Cooper Pierre-Gilles de Gennes Niels K Jerne Richard Feynman Kenichi Fukui Lawrence R Klein Herbert Kroemer Vitaly L Ginzburg David Gross H Gobind Khorana Rita Levi-Montalcini Harry M Markowitz Karl Alex Müller Sir Nevill F Mott Ben Roy Mottelson 诺贝尔奖相关图书 THE PERIODIC TABLE AND A MISSED NOBEL PRIZES THAT CHANGED MEDICINE NOBEL PRIZE edited by Gilbert Thompson (Imperial College London) by Ulf Lagerkvist & edited by Erling Norrby (The Royal Swedish Academy of Sciences) This book brings together in one volume fifteen Nobel Prize- winning discoveries that have had the greatest impact upon medical science and the practice of medicine during the 20th “This is a fascinating account of how century and up to the present time. Its overall aim is to groundbreaking scientists think and enlighten, entertain and stimulate. work. This is the insider’s view of the process and demands made on the Contents: The Discovery of Insulin (Robert Tattersall) • The experts of the Nobel Foundation who Discovery of the Cure for Pernicious Anaemia, Vitamin B12 assess the originality and significance (A Victor Hoffbrand) • The Discovery of -

Robert Burns Woodward
The Life and Achievements of Robert Burns Woodward Long Literature Seminar July 13, 2009 Erika A. Crane “The structure known, but not yet accessible by synthesis, is to the chemist what the unclimbed mountain, the uncharted sea, the untilled field, the unreached planet, are to other men. The achievement of the objective in itself cannot but thrill all chemists, who even before they know the details of the journey can apprehend from their own experience the joys and elations, the disappointments and false hopes, the obstacles overcome, the frustrations subdued, which they experienced who traversed a road to the goal. The unique challenge which chemical synthesis provides for the creative imagination and the skilled hand ensures that it will endure as long as men write books, paint pictures, and fashion things which are beautiful, or practical, or both.” “Art and Science in the Synthesis of Organic Compounds: Retrospect and Prospect,” in Pointers and Pathways in Research (Bombay:CIBA of India, 1963). Robert Burns Woodward • Graduated from MIT with his Ph.D. in chemistry at the age of 20 Woodward taught by example and captivated • A tenured professor at Harvard by the age of 29 the young... “Woodward largely taught principles and values. He showed us by • Published 196 papers before his death at age example and precept that if anything is worth 62 doing, it should be done intelligently, intensely • Received 24 honorary degrees and passionately.” • Received 26 medals & awards including the -Daniel Kemp National Medal of Science in 1964, the Nobel Prize in 1965, and he was one of the first recipients of the Arthur C. -

Max Perutz (1914–2002)
PERSONAL NEWS NEWS Max Perutz (1914–2002) Max Perutz died on 6 February 2002. He Nobel Prize for Chemistry in 1962 with structure is more relevant now than ever won the Nobel Prize for Chemistry in his colleague and his first student John as we turn attention to the smallest 1962 after determining the molecular Kendrew for their work on the structure building blocks of life to make sense of structure of haemoglobin, the red protein of haemoglobin (Perutz) and myoglobin the human genome and mechanisms of in blood that carries oxygen from the (Kendrew). He was one of the greatest disease.’ lungs to the body tissues. Perutz attemp- ambassadors of science, scientific method Perutz described his work thus: ted to understand the riddle of life in the and philosophy. Apart from being a great ‘Between September 1936 and May 1937 structure of proteins and peptides. He scientist, he was a very kindly and Zwicky took 300 or more photographs in founded one of Britain’s most successful tolerant person who loved young people which he scanned between 5000 and research institutes, the Medical Research and was passionately committed towards 10,000 nebular images for new stars. Council Laboratory of Molecular Bio- societal problems, social justice and This led him to the discovery of one logy (LMB) in Cambridge. intellectual honesty. His passion was to supernova, revealing the final dramatic Max Perutz was born in Vienna in communicate science to the public and moment in the death of a star. Zwicky 1914. He came from a family of textile he continuously lectured to scientists could say, like Ferdinand in The Tempest manufacturers and went to the Theresium both young and old, in schools, colleges, when he had to hew wood: School, named after Empress Maria universities and research institutes. -

Guides to the Royal Institution of Great Britain: 1 HISTORY
Guides to the Royal Institution of Great Britain: 1 HISTORY Theo James presenting a bouquet to HM The Queen on the occasion of her bicentenary visit, 7 December 1999. by Frank A.J.L. James The Director, Susan Greenfield, looks on Front page: Façade of the Royal Institution added in 1837. Watercolour by T.H. Shepherd or more than two hundred years the Royal Institution of Great The Royal Institution was founded at a meeting on 7 March 1799 at FBritain has been at the centre of scientific research and the the Soho Square house of the President of the Royal Society, Joseph popularisation of science in this country. Within its walls some of the Banks (1743-1820). A list of fifty-eight names was read of gentlemen major scientific discoveries of the last two centuries have been made. who had agreed to contribute fifty guineas each to be a Proprietor of Chemists and physicists - such as Humphry Davy, Michael Faraday, a new John Tyndall, James Dewar, Lord Rayleigh, William Henry Bragg, INSTITUTION FOR DIFFUSING THE KNOWLEDGE, AND FACILITATING Henry Dale, Eric Rideal, William Lawrence Bragg and George Porter THE GENERAL INTRODUCTION, OF USEFUL MECHANICAL - carried out much of their major research here. The technological INVENTIONS AND IMPROVEMENTS; AND FOR TEACHING, BY COURSES applications of some of this research has transformed the way we OF PHILOSOPHICAL LECTURES AND EXPERIMENTS, THE APPLICATION live. Furthermore, most of these scientists were first rate OF SCIENCE TO THE COMMON PURPOSES OF LIFE. communicators who were able to inspire their audiences with an appreciation of science. -

Cover June 2011
z NOBEL LAUREATES IN Qui DNA RESEARCH n u SANGRAM KESHARI LENKA & CHINMOYEE MAHARANA F 1. Who got the Nobel Prize in Physiology or Medicine 1933) for discovering the famous concept that says chromosomes carry genes? a. Gregor Johann Mendel b. Thomas Hunt Morgan c. Aristotle d. Charles Darwin 5. Name the Nobel laureate (1959) for his discovery of the mechanisms in the biological 2. The concept of Mutations synthesis of ribonucleic acid and are changes in genetic deoxyribonucleic acid? information” awarded him a. Arthur Kornberg b. Har Gobind Khorana the Nobel Prize in 1946: c. Roger D. Kornberg d. James D. Watson a. Hermann Muller b. M.F. Perutz c. James D. Watson 6. Discovery of the DNA double helix fetched them d. Har Gobind Khorana the Nobel Prize in Physiology or Medicine (1962). a. Francis Crick, James Watson, Rosalind Elsie Franklin b. Francis Crick, James Watson and Maurice Willkins c. James Watson, Maurice Willkins, Rosalind Elsie Franklin 3. Identify the discoverer and d. Maurice Willkins, Rosalind Elsie Franklin and Francis Crick Nobel laureate of 1958 who found DNA in bacteria and viruses. a. Louis Pasteur b. Alexander Fleming c. Joshua Lederberg d. Roger D. Kornberg 4. A direct link between genes and enzymatic reactions, known as the famous “one gene, one enzyme” hypothesis, was put forth by these 7. They developed the theory of genetic regulatory scientists who shared the Nobel Prize in mechanisms, showing how, on a molecular level, Physiology or Medicine, 1958. certain genes are activated and suppressed. Name a. George Wells Beadle and Edward Lawrie Tatum these famous Nobel laureates of 1965. -

Honorary Graduates – 1966 - 2004
THE UNIVERSITY OF YORK HONORARY GRADUATES – 1966 - 2004 1966 MR PATRICK BLACKETT, physicist THE RT HON LORD GARDINER, Lord Chancellor SIR PETER HALL, director of plays and operas PRESIDENT KAUNDA, Head of State SIR HENRY MOORE, sculptor SIR ROBERT READ, poet and critic THE RT HON LORD ROBBINS, economist SIR MICHAEL TIPPETT, musician and composer THE RT HON BARONESS WOOTTON OF ABINGER 1967 SIR JOHN DUNNINGTON-JEFFERSON, for services to the University DR ARTHUR GLADWIN. For services to the University PROFESSOR F R LEAVIS, literary critic PROFESSOR WASSILY LEONTIEFF, economist PROFESSOR NIKLAUS PEVSNER, art & architecture critic and historian 1968 AMADEUS QUARTET NORBET BRAININ MARTIN LOVELL SIGMUND NISSELL PETER SCHIDLOF PROFESSOR F W BROOKS, historian LORD CLARK, art historian MRS B PAGE, librarian LORD SWANN, Biologist (and Director-General of the BBC) DAME EILEEN YOUNGHUSBAND, social administrator 1969 PROFESSOR L C KNIGHTS, literacy critic SIR PETER PEARS, singer SIR GEORGE PICKERING, scholar in medicine SIR GEORGE RUSSELL, industrial designer PROFESSOR FRANCIS WORMALD, historian 1969 Chancellor’s installation ceremony THE EARL OF CRAWFORD AND BALCARRES, patron of the arts MR JULIAN CAIN, scholar and librarian PROFESSOR DAVID KNOWLES, historian MR WALTER LIPPMAN, writer & journalist 1970 PROFESSOR ROGER BROWN, social psychologist THE RT HON THE VISCOUNT ESHER, PROFESSOR DOROTHY HODGKIN, chemist PROFESSOR A J P TAYLOR, historian 1971 DAME KITTY ANDERSON, headmistress DR AARON COPLAND, composer DR J FOSTER, secretary-General of the Association -

One Million Structures and Counting the Journey, the Insights, and the Future of the CSD
One Million Structures and Counting The journey, the insights, and the future of the CSD Suzanna Ward The Cambridge Crystallographic Data Centre ECM32 – Wednesday 21st August 2019 2 The Cambridge Structural Database (CSD) 1,013,731 ▪ Every published Structures structure An N-heterocycle published produced by a that year ▪ Inc. ASAP & early view chalcogen-bonding ▪ CSD Communications catalyst. Determined Structures at Shandong published ▪ Patents University in China by previously Yao Wang and his ▪ University repositories team. XOPCAJ - The millionth CSD structure. ▪ Every entry enriched and annotated by experts ▪ Discoverability of data and knowledge ▪ Sustainable for over 54 years 3 Inside the CSD Organic ligands Additional data Organic Metal-Organic • Drugs • 10,860 polymorph families 43% 57% • Agrochemicals • 169,218 melting points • At least one transition metal, Pigments • 840,667 crystal colours lanthanide, actinide or any of Al, • Explosives Ga, In, Tl, Ge, Sn, Pb, Sb, Bi, Po • 700,002 crystal shapes • Protein ligands • 23,622 bioactivity details Polymeric: 11% Polymeric: • 9,740 natural source data Not Polymeric Metal-Organic • > 250,000 oxidation states 89% • Metal Organic Frameworks • Models for new catalysts ligand Links/subsets • Porous frameworks for gas s • Drugbank storage • Druglike • Fundamental chemical bonding • MOFs Single Multi ligands • PDB ligands Component Component • PubChem 56% 44% • ChemSpider • Pesticides 4 1965 The sound of music • Film first released in 1965 • Highest grossing film of 1965 • Set in Austria 5 The 1960s Credits: NASA Credits: Thegreenj 6 The vision • Established in 1965 by Olga Kennard • She and J.D. Bernal had a vision that a collective use of data would lead to new knowledge and generate insights J.D. -

Notes and News
Notes and News Sir Aaron Klug, NL, The Discoverer of his Ph.D. degree in Physics in 1953 from the Trinity Crystallographic Electron Microscopy, College, Cambridge. Passes Away In late 1953, he moved to the Birkbeck College, University of London where he started collaborating with ubbed ‘one of the mildest, most broad-minded and the X-ray crystallographer Rosalind Franklin on her studies Dmost cultured of scientists’, Aaron Klug, who was on tobacco mosaic virus. The combined commendable awarded the Nobel Prize in Chemistry in 1982 for “his technical skill of Franklin in producing X-ray diffraction development of crystallographic electron microscopy and images and deep theoretical understanding of matter by his structural elucidation of biologically important nucleic Klug led to the determination of the general outline of the acid-protein complexes,” died on November 20, 2018 at structure of this virus just before the untimely demise of the age of 92 years. Franklin from cancer in 1958. Klug always acknowledged Klug was born on 11th August, 1926 in •elva, the help that he received from Rosalind in this domain of Lithuania to Jewish parents Lazar Klug, a cattleman, and research. Bella (née Silin) Klug. His family moved to South Africa In 1962, Klug joined the newly founded MRC when he was two years old. He had his early education in Laboratory of Molecular Biology (LMB) in Cambridge Durban High School. He received his B.Sc. degree with a where he used X-ray diffraction methods, microscopy and first class Honours from the University of the structural modelling to develop ‘crystallographic electron Witwaterstrand and his M.Sc.