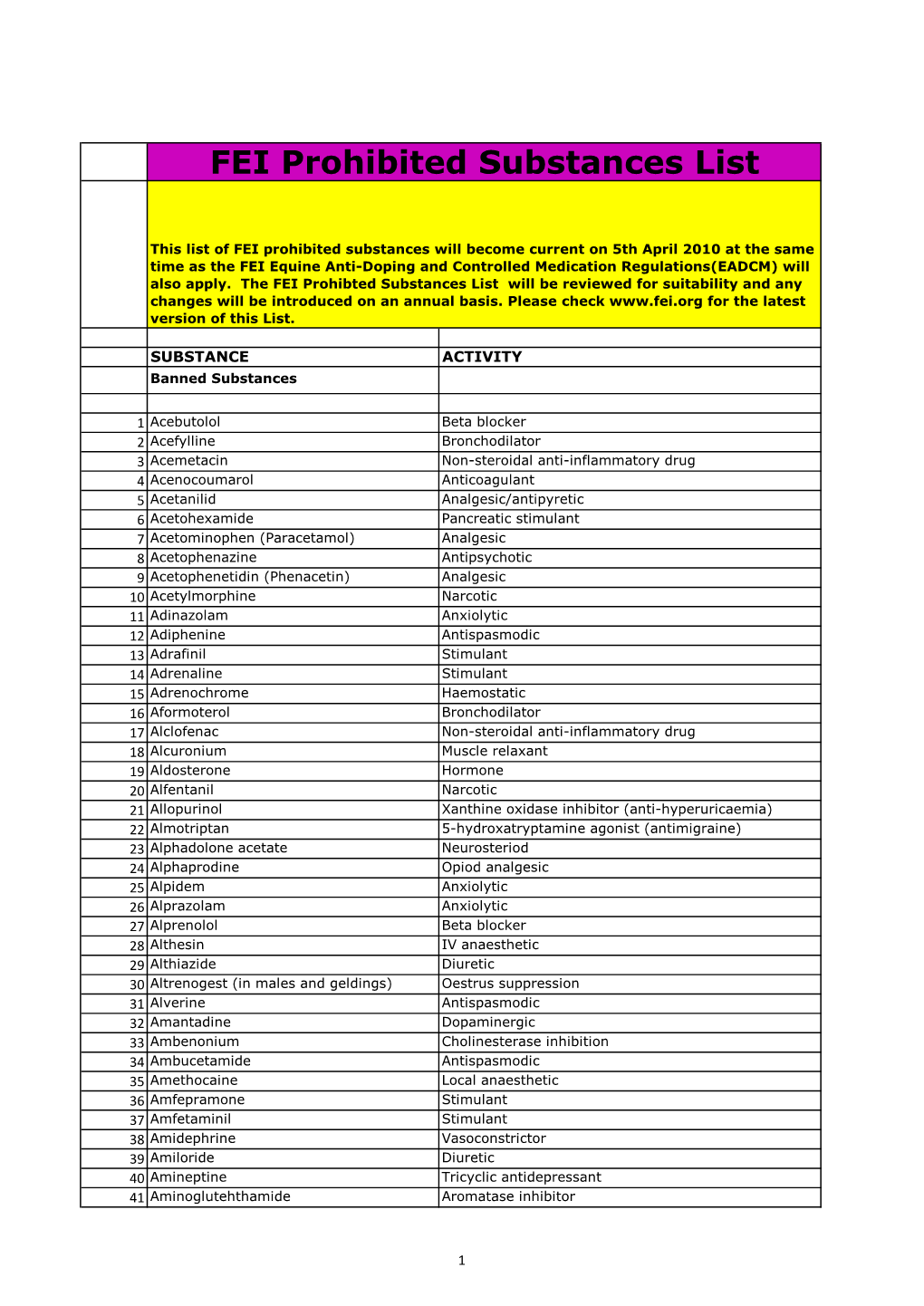
FEI Prohibited Substances List
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers with Topical Pharmaceutical Agents
Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers With Topical Pharmaceutical Agents Author Watts, Annabelle M, Cripps, Allan W, West, Nicholas P, Cox, Amanda J Published 2019 Journal Title FRONTIERS IN PHARMACOLOGY Version Version of Record (VoR) DOI https://doi.org/10.3389/fphar.2019.00294 Copyright Statement © Frontiers in Pharmacology 2019. The attached file is reproduced here in accordance with the copyright policy of the publisher. Please refer to the journal's website for access to the definitive, published version. Downloaded from http://hdl.handle.net/10072/386246 Griffith Research Online https://research-repository.griffith.edu.au fphar-10-00294 March 27, 2019 Time: 17:52 # 1 REVIEW published: 29 March 2019 doi: 10.3389/fphar.2019.00294 Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers With Topical Pharmaceutical Agents Annabelle M. Watts1*, Allan W. Cripps2, Nicholas P. West1 and Amanda J. Cox1 1 Menzies Health Institute Queensland, School of Medical Science, Griffith University, Southport, QLD, Australia, 2 Menzies Health Institute Queensland, School of Medicine, Griffith University, Southport, QLD, Australia Allergic rhinitis (AR) is a chronic upper respiratory disease estimated to affect between 10 and 40% of the worldwide population. The mechanisms underlying AR are highly complex and involve multiple immune cells, mediators, and cytokines. As such, the development of a single drug to treat allergic inflammation and/or symptoms is confounded by the complexity of the disease pathophysiology. Complete avoidance of allergens that trigger AR symptoms is not possible and without a cure, the available therapeutic options are typically focused on achieving symptomatic relief. -

Comparison of Norepinephrine and Cafedrine/Theodrenaline Regimens for Maintaining Maternal Blood Pressure During
IBIMA Publishing Obstetrics & Gynecology: An International Journal http://www.ibimapublishing.com/journals/GYNE/gyne.html Vol. 2015 (2015), Article ID 714966, 12 pages DOI: 10.5171/2015.714966 Research Article Comparison of Norepinephrine and Cafedrine/Theodrenaline Regimens for Maintaining Maternal Blood Pressure during Spinal Anaesthesia for Caesarean Section Hoyme, M.1, Scheungraber, C.2, Reinhart, K.3 and Schummer, W.3 1Department of Internal Medicine I (Cardiology, Angiology, Pneumology) Friedrich Schiller University, Jena, Germany 2Departments of Obstetrics and Gynecology, Friedrich Schiller University, Jena, Germany 3Clinic of Anaesthesiology and Intensive Care Medicine, Friedrich Schiller University, Jena, Germany Correspondence should be addressed to: Schummer, W.; [email protected] Received date: 9 January 2014; Accepted date: 4 April 2014; Published date: 26 August 2015 Academic Editor: Dan Benhamou Copyright © 2015. Hoyme, M., Scheungraber, C., Reinhart, K. and Schummer, W. Distributed under Creative Commons CC-BY 4.0 Abstract Common phenomena of spinal anaesthesia for caesarean sections are hypotension and cardiovascular depression, both of which require immediate action. Akrinor® (theodrenaline and cafedrine), a sympathomimetic agent commonly used in Germany for such cases, was phased out with little notice at the end of 2005. Phenylephrine was not and is not an approved drug. Norepinephrine became the first-line drug. The outcome in neonates delivered by elective caesarean section under spinal anaesthesia was studied. At our university hospital, all elective caesarean sections under spinal anaesthesia from 2005 and 2006 were analysed regarding hypotension and the vasopressor administered. If maternal arterial pressure decreased by more than 20% of baseline, patients in 2005 received Akrinor®; patients in 2006 received norepinephrine. -

Hypotension After Spinal Anesthesia for Cesarean
REVIEW CURRENT OPINION Hypotension after spinal anesthesia for cesarean section: how to approach the iatrogenic sympathectomy Christina Massotha, Lisa To¨pelb, and Manuel Wenkb Purpose of review Hypotension during cesarean section remains a frequent complication of spinal anesthesia and is associated with adverse maternal and fetal events. Recent findings Despite ongoing research, no single measure for sufficient treatment of spinal-induced hypotension was 05/25/2020 on BhDMf5ePHKbH4TTImqenVDezntqwKeJGjCYTUOBBz0EyVSh+WquM7uJo3U//pWTO by http://journals.lww.com/co-anesthesiology from Downloaded Downloaded identified so far. Current literature discusses the efficacy of low-dose spinal anesthesia, timing and solutions for adequate fluid therapy and various vasopressor regimens. Present guidelines favor the use of from phenylephrine over ephedrine because of decreased umbilical cord pH values, while norepinephrine is http://journals.lww.com/co-anesthesiology discussed as a probable superior alternative with regard to maternal bradycardia, although supporting data is limited. Alternative pharmacological approaches, such as 5HT3-receptor antagonists and physical methods may be taken into consideration to further improve hemodynamic stability. Summary Current evidence favors a combined approach of low-dose spinal anesthesia, adequate fluid therapy and vasopressor support to address maternal spinal-induced hypotension. As none of the available vasopressors by is associated with relevantly impaired maternal and fetal outcomes, none of them should -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group R01 (Nasal preparations) Table of Contents Page INTRODUCTION 5 DISCLAIMER 7 GLOSSARY OF TERMS USED IN THIS DOCUMENT 8 ACTIVE SUBSTANCES Cyclopentamine (ATC: R01AA02) 10 Ephedrine (ATC: R01AA03) 11 Phenylephrine (ATC: R01AA04) 14 Oxymetazoline (ATC: R01AA05) 16 Tetryzoline (ATC: R01AA06) 19 Xylometazoline (ATC: R01AA07) 20 Naphazoline (ATC: R01AA08) 23 Tramazoline (ATC: R01AA09) 26 Metizoline (ATC: R01AA10) 29 Tuaminoheptane (ATC: R01AA11) 30 Fenoxazoline (ATC: R01AA12) 31 Tymazoline (ATC: R01AA13) 32 Epinephrine (ATC: R01AA14) 33 Indanazoline (ATC: R01AA15) 34 Phenylephrine (ATC: R01AB01) 35 Naphazoline (ATC: R01AB02) 37 Tetryzoline (ATC: R01AB03) 39 Ephedrine (ATC: R01AB05) 40 Xylometazoline (ATC: R01AB06) 41 Oxymetazoline (ATC: R01AB07) 45 Tuaminoheptane (ATC: R01AB08) 46 Cromoglicic Acid (ATC: R01AC01) 49 2 Levocabastine (ATC: R01AC02) 51 Azelastine (ATC: R01AC03) 53 Antazoline (ATC: R01AC04) 56 Spaglumic Acid (ATC: R01AC05) 57 Thonzylamine (ATC: R01AC06) 58 Nedocromil (ATC: R01AC07) 59 Olopatadine (ATC: R01AC08) 60 Cromoglicic Acid, Combinations (ATC: R01AC51) 61 Beclometasone (ATC: R01AD01) 62 Prednisolone (ATC: R01AD02) 66 Dexamethasone (ATC: R01AD03) 67 Flunisolide (ATC: R01AD04) 68 Budesonide (ATC: R01AD05) 69 Betamethasone (ATC: R01AD06) 72 Tixocortol (ATC: R01AD07) 73 Fluticasone (ATC: R01AD08) 74 Mometasone (ATC: R01AD09) 78 Triamcinolone (ATC: R01AD11) 82 -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Rhinitis - Allergic (1 of 15)
Rhinitis - Allergic (1 of 15) 1 Patient presents w/ signs & symptoms of rhinitis 2 • Consider other classifi cations of rhinitis DIAGNOSIS No - Please see Rhinitis Is allergic rhinitis - Nonallergic disease confi rmed? management chart Yes 3 ASSESS DURATION & SEVERITY OF ALLERGIC RHINITIS A Non-pharmacological therapy • Allergen avoidance • Patient education VAS <5 VAS ≥5 B Pharmacological therapy B Pharmacological therapy • Antihistamines (oral/nasal), &/or • Corticosteroids (nasal), w/ or without • Corticosteroids (nasal), or • Antihistamines (nasal), or • Cromone (nasal), or • LTRA • Leukotriene receptor antagonists (LTRA)MIMS TREATMENT © See next page Specifi cally for patients w/ asthma Not all products are available or approved for above use in all countries. Specifi c prescribing information may be found in the latest MIMS. B167 © MIMS Pediatrics 2020 Rhinitis - Allergic (2 of 15) Previously treated symptomatic Previously treated symptomatic patient (VAS <5) on antihistamines patient (VAS ≥5) on intensifi ed (oral/nasal) &/or corticosteroids (nasal) therapy w/ corticosteroids (nasal) w/ or without antihistamines (nasal) Intermittent Persistent symptoms, symptoms or without allergen w/ allergen exposure exposure B Pharmacological therapy B Pharmacological therapy • Step down or discontinue therapy • Continue or step up therapy Untreated REASSESS DISEASE SEVERITY VAS symptomatic patient DAILY UP TO DAY 3 (VAS <5 or ≥5) 4 CONTINUE Yes THERAPY & STEP EVALUATION VAS <5 DOWN THERAPY1 Improvement of symptoms? No VAS ≥5 B Pharmacological therapy • Step-up therapy REASSESS DISEASE SEVERITY MIMSVAS DAILY UP TO DAY 7 4 Yes EVALUATION VAS <5 Improvement of symptoms? No TREATMENT © VAS ≥5 See next page Continue therapy if symptomatic; consider step-down or discontinuation of therapy if symptoms subside Not all products are available or approved for above use in all countries. -

Phosphodiesterase (PDE)
Phosphodiesterase (PDE) Phosphodiesterase (PDE) is any enzyme that breaks a phosphodiester bond. Usually, people speaking of phosphodiesterase are referring to cyclic nucleotide phosphodiesterases, which have great clinical significance and are described below. However, there are many other families of phosphodiesterases, including phospholipases C and D, autotaxin, sphingomyelin phosphodiesterase, DNases, RNases, and restriction endonucleases, as well as numerous less-well-characterized small-molecule phosphodiesterases. The cyclic nucleotide phosphodiesterases comprise a group of enzymes that degrade the phosphodiester bond in the second messenger molecules cAMP and cGMP. They regulate the localization, duration, and amplitude of cyclic nucleotide signaling within subcellular domains. PDEs are therefore important regulators ofsignal transduction mediated by these second messenger molecules. www.MedChemExpress.com 1 Phosphodiesterase (PDE) Inhibitors, Activators & Modulators (+)-Medioresinol Di-O-β-D-glucopyranoside (R)-(-)-Rolipram Cat. No.: HY-N8209 ((R)-Rolipram; (-)-Rolipram) Cat. No.: HY-16900A (+)-Medioresinol Di-O-β-D-glucopyranoside is a (R)-(-)-Rolipram is the R-enantiomer of Rolipram. lignan glucoside with strong inhibitory activity Rolipram is a selective inhibitor of of 3', 5'-cyclic monophosphate (cyclic AMP) phosphodiesterases PDE4 with IC50 of 3 nM, 130 nM phosphodiesterase. and 240 nM for PDE4A, PDE4B, and PDE4D, respectively. Purity: >98% Purity: 99.91% Clinical Data: No Development Reported Clinical Data: No Development Reported Size: 1 mg, 5 mg Size: 10 mM × 1 mL, 10 mg, 50 mg (R)-DNMDP (S)-(+)-Rolipram Cat. No.: HY-122751 ((+)-Rolipram; (S)-Rolipram) Cat. No.: HY-B0392 (R)-DNMDP is a potent and selective cancer cell (S)-(+)-Rolipram ((+)-Rolipram) is a cyclic cytotoxic agent. (R)-DNMDP, the R-form of DNMDP, AMP(cAMP)-specific phosphodiesterase (PDE) binds PDE3A directly. -

Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

7-Nose II.Docx ( Updated F1 )
1 [Color index: Important | Notes | Extra] Editing 2 Diseases of the nose Supernumerary nostril Midline nasal sinus: Nasal clefts: Proboscis lateralis: Incomplete fusion of the right Failure of frontal nasal Due to imperfect fusion and left medial nasal process to develop between the maxillary process prominence. appropriately results into and the lateral nasal process. two separated halves of the nose. Polyrrhinia: Arrhinia: due to bilateral Half nose: due to unilateral absence of nasal placode Duplication of the medial nasal absence of nasal placodes. processes. This is serious because the newborn is a nose breather. mouth breathing is a learning process. Atresia of posterior nares ❖ Types: ● Bony (most commonly) ● Membranous ● Mixed ● Complete unilateral (most commonly) ● Complete bilateral surgical emergency ● Incomplete unilateral ● Incomplete bilateral ❖ Diagnosis: ● Total absence of nasal air flow ● Plastic catheter cannot be passed through the nose ● Post-rhinoscopy ● Radiographs 3 ● Emergency ● Transnasal perforation ● Trans-palatal excision ❖ Management: ﻧﻔﺘﺢ ﻓﻤﻪ ﻓﯿﻀﻄﺮ ﯾﺘﻨﻔﺲ ﻣﻦ ﻓﻤﻪ (Put something to open the mouth (oral airway ● ● Perforate it If membranous ● Surgery (endoscopic) ● In bilateral it is an emergency, in unilateral it is not an emergency and we can wait until the child gains weight then we do surgery. ● Rhinitis refers to inflammatory changes in the nasal mucosa. As the nasal mucosa is continuous over the nose and sinuses, there is nearly always some inflammatory change in the sinuses as 1 well. Hence Rhinosinusitis is a better term. ● Types: - acute rhinitis (less than 4 weeks) - chronic rhinitis (more than four consecutive weeks) ● Types based on etiology: 1) Infectious rhinitis(viral/bacterial) 2)Non-allergic Rhinitis,Non-infectious rhinitis -Eosinophilic syndromes(Nares/Nasal polyposis) -NonEosinophilic syndromes(Vasomotor rhinitis/Rhinitis medicamentosa/occupational rhinitis/Rhinitis of pregnancy/hypothyroidism/Medication(OCP). -

Pharmaceuticals Appendix
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ADAPALENE 106685-40-9 ABANOQUIL 90402-40-7 ADAPROLOL 101479-70-3 ABECARNIL 111841-85-1 ADEMETIONINE 17176-17-9 ABLUKAST 96566-25-5 ADENOSINE PHOSPHATE 61-19-8 ABUNIDAZOLE 91017-58-2 ADIBENDAN 100510-33-6 ACADESINE 2627-69-2 ADICILLIN 525-94-0 ACAMPROSATE 77337-76-9 ADIMOLOL 78459-19-5 ACAPRAZINE 55485-20-6 ADINAZOLAM 37115-32-5 ACARBOSE 56180-94-0 ADIPHENINE 64-95-9 ACEBROCHOL 514-50-1 ADIPIODONE 606-17-7 ACEBURIC ACID 26976-72-7 ADITEREN 56066-19-4 ACEBUTOLOL 37517-30-9 ADITOPRIME 56066-63-8 ACECAINIDE 32795-44-1 ADOSOPINE 88124-26-9 ACECARBROMAL 77-66-7 ADOZELESIN 110314-48-2 ACECLIDINE 827-61-2 ADRAFINIL 63547-13-7 ACECLOFENAC 89796-99-6 ADRENALONE 99-45-6 ACEDAPSONE 77-46-3 AFALANINE 2901-75-9 ACEDIASULFONE SODIUM 127-60-6 AFLOQUALONE 56287-74-2 ACEDOBEN 556-08-1 AFUROLOL 65776-67-2 ACEFLURANOL 80595-73-9 AGANODINE 86696-87-9 ACEFURTIAMINE 10072-48-7 AKLOMIDE 3011-89-0 ACEFYLLINE CLOFIBROL 70788-27-1 -

In Silico Methods in Prediction of Drug Metabolism, Mass Fragmentation, and Chromatographic Behavior
Hjelt Institute Department of Forensic Medicine University of Helsinki Finland IN SILICO METHODS IN PREDICTION OF DRUG METABOLISM, MASS FRAGMENTATION, AND CHROMATOGRAPHIC BEHAVIOR APPLICATION TO TOXICOLOGICAL DRUG SCREENING BY LIQUID CHROMATOGRAPHY/TIME-OF-FLIGHT MASS SPECTROMETRY Elli Tyrkkö ACADEMIC DISSERTATION To be publicly discussed, with the permission of the Medical Faculty of the University of Helsinki, in the auditorium of Department of Forensic Medicine on April 25th 2014, at 12 noon. Helsinki 2014 SUPERVISORS Professor Ilkka Ojanperä Hjelt Institute Department of Forensic Medicine University of Helsinki, Finland Dr. Anna Pelander Hjelt Institute Department of Forensic Medicine University of Helsinki, Finland REVIEWERS Docent Tuulia Hyötyläinen VTT, Technical Research Centre of Finland Helsinki, Finland Docent Ari Tolonen Admescope Oulu, Finland OPPONENT Dr. Frank T. Peters Forensic and Clinical Toxicology Institute of Forensic Medicine University of Jena, Germany ISBN 978-952-10-9574-0 (paperback) ISBN 978-952-10-9575-7 (PDF) http://ethesis.helsinki.fi Unigrafia Helsinki 2014 Any fool can know. The point is to understand. Albert Einstein CONTENTS CONTENTS ............................................................................................................................4 ABBREVIATIONS ..................................................................................................................6 LIST OF ORIGINAL PUBLICATIONS ................................................................................. 7 ABSTRACT -

Rhinitis (415) 833-3780
Department of Allergy, Asthma & Immunology Kaiser Permanente San Francisco 1635 Divisadero Street, Suite 101 San Francisco, California 94115 RHINITIS (415) 833-3780 RHINITIS Nasal congestion, runny nose, sneezing, itching, post nasal drip, and sometimes headache are signs of a sensitive and inflamed nose or rhinitis. Rhinitis affects more than 40 million people in the United States. Rhinitis can be allergic or non-allergic. Allergy testing will help differentiate between allergic and non-allergic rhinitis. In addition, allergic rhinitis and non-allergic rhinitis can be present in the same person. ALLERGIC RHINITIS Allergic rhinitis is caused by allergens such as pollens, dust mite, animal dander or mold. Seasonal allergies caused by airborne pollens occur during spring, summer and fall. In contrast, allergies that can occur at any time of the year are caused by indoor allergens such as house dust mite, animals and mold. Eye symptoms, such as itching, tearing, red eye as well as asthma may be present with allergic rhinitis. Testing can be helpful in identifying both seasonal and non-seasonal allergens. For further help on controlling your allergies, please refer to the brochure, Controlling Your Airborne Allergies. Management of Allergic Rhinitis 1. Avoid allergens when possible. 2. Medical Management. The first line of medical therapy is nasal inhaled steroids. Oral medications like antihistamines and decongestants and can be helpful. If you want to use decongestants, you need to discuss their use with your provider. Other medications may be considered by your provider as well. 3. Allergy immunotherapy (shots) may be an option for some patients. NON-ALLERGIC RHINITIS If it isn’t an allergy, what is it? If it isn’t an allergy, most likely it is a condition that mimics allergic rhinitis, known as vasomotor rhinitis.