Rocky Mountain Spotted Fever
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recognizing and Treating New and Emerging Infections Encountered in Everyday Practice
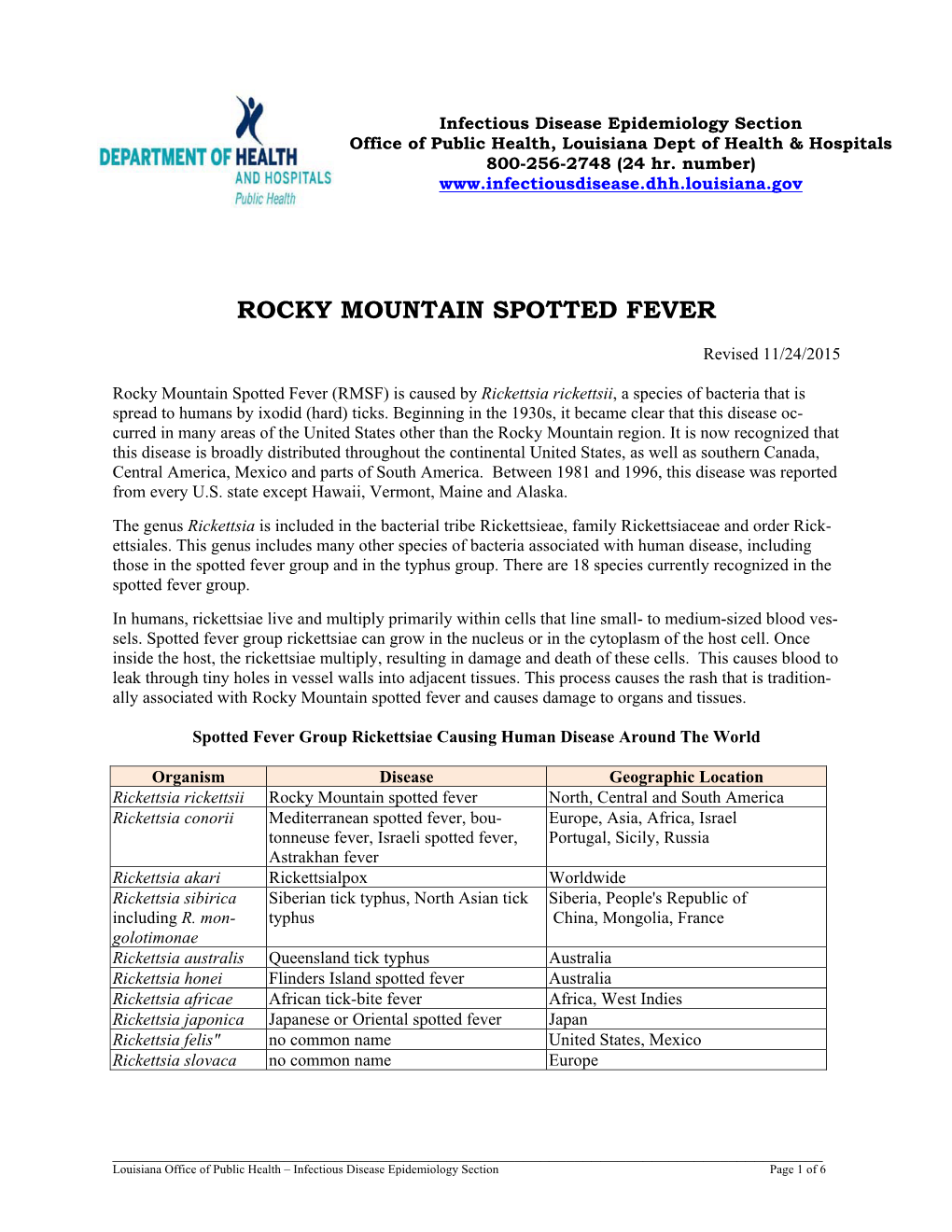
Recognizing and treating new and emerging infections encountered in everyday practice STEVEN M. GORDON, MD NFECTIOUS DISEASES, pre- MiikWirj:« Although infectious diseases were once considered a dicted earlier in this cen- diminishing threat, new pathogens are constantly challenging tury to be eliminated as a the health care system. This article reviews the clinical presen- public health problem, re- tation, diagnosis, and treatment of seven emerging infections I main the chief cause of death that primary care physicians are likely to encounter. worldwide and a significant cause of death and morbidity in i Parvovirus B19 attacks erythrocyte precursors; the United States.1 Challenging infection is usually benign and self-limiting but can cause the US public health system are aplastic crises in patients with chronic hemolytic disorders. several newly identified patho- Hemorrhagic colitis due to Escherichia coli 0157:H7 infection gens (eg, human immunodefi- can lead to the hemolytic-uremic syndrome, especially in chil- ciency virus [HIV], Escherichia dren; it also can cause thrombotic thrombocytopenia purpura. coli 0157:H7, hepatitis C) and a Chlamydia pneumoniae causes a mild pneumonia that resem- resurgence of old diseases pre- bles mycoplasmal pneumonia. Bacillary angiomatosis primar- sumed to be under control (eg, ily affects immunocompromised patients, especially those tuberculosis, syphilis). Further, infected with human immunodeficiency virus (HIV). At least multiple-drug resistance in two organisms can cause bacillary angiomatosis: Bartonella hense- strains of pneumococci, gono- lae and Bartonella quintana. Hantavirus pulmonary syndrome cocci, enterococci, staphylo- is spread by exposure to the droppings of infected rodents. cocci, salmonella, and mycobac- Contrary to previous thought, HIV continues to replicate teria undermines efforts to throughout the course of the illness and does not have a latency control the diseases they cause.2 phase. -

Lyme Disease Weather Also Means That Ticks Become More Active and This Can Agent by Feeding As Larvae on Certain Rodent Species
Spring and summer bring warm temperatures, just right for small and medium sized animals, but will also feed on people. walking in the woods and other outdoor activities. Warm These ticks typically become infected with the Lyme disease weather also means that ticks become more active and this can agent by feeding as larvae on certain rodent species. increase the risk of a tick-borne disease. The tick-borne dis- In the fall, the nymphs become adults and infected nymphs eases that occur most often in Virginia are Lyme disease, become infected adults. Adult blacklegged ticks prefer to feed Rocky Mountain spotted fever, and ehrlichiosis. on deer. However, adult ticks will occasionally bite people on warm days of the fall and winter and can transmit Lyme disease Lyme Disease at that time. Lyme disease is caused by infection with a bacterium called Borrelia burgdorferi. The number of Lyme disease cases Transmission of Lyme disease by the nymph or adult ticks reported in Virginia has increased substantially in recent years. does not occur until the tick has been attached and feeding on a human or animal host for at least 36 hours. The Tick The blacklegged tick (Ixodes scapularis), formerly known as The Symptoms the deer tick, is the only carrier of Lyme disease in the Eastern Between three days to several weeks after being bitten by an U.S. The blacklegged tick's name comes from it being the only infected tick, 70-90% of people develop a circular or oval rash, tick in the Eastern U.S. that bites humans and has legs that are called erythema migrans (or EM), at the site of the bite. -

Reportable Disease Surveillance in Virginia, 2013
Reportable Disease Surveillance in Virginia, 2013 Marissa J. Levine, MD, MPH State Health Commissioner Report Production Team: Division of Surveillance and Investigation, Division of Disease Prevention, Division of Environmental Epidemiology, and Division of Immunization Virginia Department of Health Post Office Box 2448 Richmond, Virginia 23218 www.vdh.virginia.gov ACKNOWLEDGEMENT In addition to the employees of the work units listed below, the Office of Epidemiology would like to acknowledge the contributions of all those engaged in disease surveillance and control activities across the state throughout the year. We appreciate the commitment to public health of all epidemiology staff in local and district health departments and the Regional and Central Offices, as well as the conscientious work of nurses, environmental health specialists, infection preventionists, physicians, laboratory staff, and administrators. These persons report or manage disease surveillance data on an ongoing basis and diligently strive to control morbidity in Virginia. This report would not be possible without the efforts of all those who collect and follow up on morbidity reports. Divisions in the Virginia Department of Health Office of Epidemiology Disease Prevention Telephone: 804-864-7964 Environmental Epidemiology Telephone: 804-864-8182 Immunization Telephone: 804-864-8055 Surveillance and Investigation Telephone: 804-864-8141 TABLE OF CONTENTS INTRODUCTION Introduction ......................................................................................................................................1 -

Lyme Disease Rocky Mountain Spotted Fever Tick Paralysis Haemobartonellosis Tularemia Ehrlichiosis Anaplasmosis
Fall is the beginning of tick season in our area. However, you can find ticks all year round if you like to hike or camp in the woods, or other type of outdoor activities. Ticks are not as easy to kill as fleas, but there are several different ways to control ticks from oral to topical medications and well as collars. If you find a tick embedded in your pet and you choose to try and remove it, be aware that you can accidentally leave the head behind. This can cause a local irritation even possibly an infection. We will be happy to assist with removing a tick for you to help prevent any problems. Protecting your cat or dog (or both) from ticks is an important part of disease prevention. In fact, there are several diseases that can be transmitted to your pet from a tick bite. Some of the most common tick-borne diseases seen in the Western United States are: Lyme Disease Rocky Mountain Spotted Fever Tick Paralysis Haemobartonellosis Tularemia Ehrlichiosis Anaplasmosis Lyme Disease Also called borreliosis, Lyme disease is caused by the bacteria Borrelia burgdorferi. Deer ticks carry these bacteria, transmitting them to the animal while sucking its blood. The tick must be attached to the dog (or cat) for about 48 hours in order to transmit the bacteria to the animal's bloodstream. If the tick is removed before this, transmission will usually not occur. Common signs of Lyme disease include lameness, fever, swollen lymph nodes and joints, and a reduced appetite. In severe cases, animals may develop kidney disease, heart conditions, or nervous system disorders. -

Melioidosis in Northern Tanzania: an Important Cause of Febrile Illness?
Melioidosis and serological evidence of exposure to Burkholderia pseudomallei among patients with fever, northern Tanzania Michael Maze Department of Medicine University of Otago, Christchurch Melioidosis Melioidosis caused by Burkholderia pseudomallei • Challenging to identify when cultured Soil reservoir, with human infection from contact with contaminated water Most infected people are asymptomatic: 1 clinical illness for 4,500 antibody producing exposures Febrile illness with a variety of presentations and bacteraemia is present in 40-60% of people with acute illness Estimated 89,000 deaths globally Gavin Koh CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=4975784 Laboratory diagnosis of febrile inpatients, northern Tanzania, 2007-8 (n=870) Malaria (1.6%) Bacteremia (9.8%) Mycobacteremia (1.6%) Fungemia (2.9%) Brucellosis (3.5%) Leptospirosis (8.8%) Q fever (5.0%) No diagnosis (50.1%) Spotted fever group rickettsiosis (8.0%) Typhus group rickettsiosis (0.4%) Chikungunya (7.9%) Crump PLoS Neglect Trop Dis 2013; 7: e2324 Predicted environmental suitability for B. pseudomallei in East Africa Large areas of Africa are predicted to be highly suitable for Burkholderia pseudomallei East Africa is less suitable but pockets of higher suitability including northern Tanzania Northern Tanzania Increasing suitability for B. pseudomallei Limmathurotsakul Nat Microbiol. 2016;1(1). Melioidosis epidemiology in Africa Paucity of empiric data • Scattered case reports • Report from Kilifi, Kenya identified 4 bacteraemic cases from 66,000 patients who had blood cultured1 • 5.9% seroprevalence among healthy adults in Uganda2 • No reports from Tanzania 1. Limmathurotsakul Nat Microbiol. 2016;1(1). 2. Frazer J R Army Med Corps. 1982;128(3):123-30. -

Rickettsialpox-A Newly Recognized Rickettsial Disease V
Public Health Reports Vol. 62 * MAY 30, 1947 * No. 22 Printed With the Approval of the Bureau of the Budget as Required by Rule 42 of the Joint-Committee on Printing RICKETTSIALPOX-A NEWLY RECOGNIZED RICKETTSIAL DISEASE V. RECOVERY OF RICKETTSIA AKARI FROM A HOUSE MOUSE (MUS MUSCULUS)1 By ROBERT J. HUEBNER, Senior Assistant Surgeon, WILLIAm L. JELLISON, Parasitologist, CHARLES ARMSTRONG, Medical Director, United States Public Health Service Ricketttia akari, the causative agent of rickettsialpox, was isolated from the blood of persons ill with this disease (1) and from rodent mites Allodermanyssus sanguineus Hirst inhabiting the domicile of ill per- sons (2). This paper describes the isolation of R. akari from a house mouse (Mus musculus) trapped on the same premises-a housing development in the citr of New York where more than 100 cases of rickettsialpox have occurred (3), (4), (5), (6). Approximately 60 house mice were trapped in the basements of this housing development where rodent harborage existed in store rooms and in incinerator ashpits. Engorged mites were occasionally found attached to the mice, the usual site of attachment being the rump. Mites were frequently found inside the box traps after the captured mice were removed. Early attempts to isolate the etiological agent of rickettisalpox from these mice were complicated by the presence of choriomeningitis among them. Twelve successive suspensions of mouse tissue, repre- senting 16 house mice, inoculated intracerebrally into laboratory mice (Swiss strain) and intraperitoneally into guinea pigs resulted in the production of a highly lethal disease in both species which was identified immunologically as choriomeningitis. -

Rocky Mountain Spotted Fever
Department of Public Health Office of Epidemiology 4041 N Central Ave. Ste 600 Phoenix, AZ 85012 Rocky Mountain Spotted Fever Rocky Mountain Spotted Fever (RMSF) is a disease caused by the bacteria Rickettsia rickettsii. The bacteria are transmitted to humans through the bite of an infected tick, most commonly the American dog tick (Dermacentor variabilis) or Rocky Mountain wood tick (Dermacentor andersoni). The disease was first recognized in the Rocky Mountain area, however, despite the disease’s name, relatively few cases occur in the Rocky Mountain west. Most cases of RMSF occur in the Southeast and South central regions of the United States between the months of April and August, but in Arizona tick activity has been seen from March to September. RMSF used to be a rare disease in Arizona, however, it has become increasingly common over the last several years. Between 2003 and 2012, over 250 cases and 19 fatalities occurred in Arizona. Almost all of these cases occurred in areas with large amounts of free-roaming dogs and severe tick infestations, including six Tribal lands. During 2010-2011, RMSF in Arizona occurred at a rate ~200 times the national average. RMSF can be rapidly fatal if not treated within the first 5 days of symptom onset. Before tetracycline antibiotics were available, case fatality rates ranged from 20-80%. Signs and Symptoms Symptoms usually present in 2-14 days usually with a sudden onset of moderate to high fever, significant malaise, deep muscle pain, severe headache, chills and conjunctival infection. The “typical” triad of fever, rash, and tick bite are only presented between 21-40% of the time. -

Rickettsia Felis, Bartonella Henselae, and B. Clarridgeiae, New Zealand
LETTERS Richard Reithinger,*† domestic and wild animals that also products obtained by PCR with Khoksar Aadil,† Samad Hami,† feeds readily on people. Recent stud- primers for the 17-kDa protein (4), and Jan Kolaczinski*† ies have implicated the cat flea as a citrate synthase (4), and PS 120 pro- *London School of Hygiene and Tropical vector of new and emerging infectious tein (5) genes. R. felis has been estab- Medicine, London, United Kingdom; and diseases (1). To determine the lished in tissue culture (XTC-2 and †HealthNet International, Peshawar, pathogens in C. felis in New Zealand, Vero cells) (6), and serologic testing Pakistan we collected 3 cat fleas from each of has been used to diagnose infections 11 dogs and 21 cats at the Massey (5). Reports indicate that patients References University Veterinary Teaching respond rapidly to doxycycline thera- 1. Ashford R, Kohestany K, Karimzad M. Hospital from May to June 2003. The py (5), and in vitro studies have Cutaneous leishmaniasis in Kabul: observa- fleas were stored in 95% alcohol until shown the organism is susceptible to tions on a prolonged epidemic. Ann Trop Med Parasitol 1992;86:361–71. they were identified by using morpho- rifampin, thiamphenicol, and fluoro- 2. Griffiths WDA. Old World cutaneous leish- logic criteria and washed in sterile quinolones. maniasis. In: Peters W, Killick-Kendrick R, phosphate-buffered saline. The DNA B. henselae is an agent of cat- editors. The leishmaniases in biology and from each flea was extracted individ- scratch disease, bacillary angiomato- medicine. London: Academic Press; 1987. p. 617–43. ually by using the QiaAmp Tissue Kit sis, bacillary peliosis, endocarditis, 3. -

Rocky Mountain Spotted Fever in Children
Rocky Mountain Spotted Fever in Children Charles R. Woods, MD, MS KEYWORDS Rocky mountain spotted fever Rickettsia rickettsii Rash Increased intracranial pressure Sepsis Doxycycline KEY POINTS Rocky Mountain spotted fever (RMSF) is typically undifferentiated from many other infec- tions in the first few days of illness. Treatment should not be delayed pending confirmation of infection when RMSF is suspected. Doxycycline is the drug of choice even for infants and children less than 8 years old. INTRODUCTION RMSF is caused by Rickettsia rickettsii, the prototypical member of the spotted fever subgroup of rickettsial species. RMSF was first recognized as a clinical entity in the 1890s in Idaho and Montana. In the past century, RMSF has been identified within 46 states in the United States. R rickettsii also causes disease in many parts of Central and South America, where the infection is given other names, such as Brazilian spotted fever or febre maculosa.1,2 The spotted fever subgroup of Rickettsia now consists of 20 known species that cause similar illnesses worldwide.3–5 R parkeri and other related species are present among tick populations in the United States. Infection by these related species may account in part for the apparent increase in probable, but not confirmed, cases of RMSF in the United States in recent years.6 RMSF remains a nationally notifiable disease, but reporting was changed in 2010 under the broader category of spotted fever rickettsiosis.7 The pathogenesis, clinical features, and management of infections caused by the various agents of spotted fever rickettsiosis are largely the same. Laboratory studies of R conorii, the cause of Mediterranean spotted fever, have provided many insights into R rickettsii infections. -

The Approved List of Biological Agents Advisory Committee on Dangerous Pathogens Health and Safety Executive
The Approved List of biological agents Advisory Committee on Dangerous Pathogens Health and Safety Executive © Crown copyright 2021 First published 2000 Second edition 2004 Third edition 2013 Fourth edition 2021 You may reuse this information (excluding logos) free of charge in any format or medium, under the terms of the Open Government Licence. To view the licence visit www.nationalarchives.gov.uk/doc/ open-government-licence/, write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email [email protected]. Some images and illustrations may not be owned by the Crown so cannot be reproduced without permission of the copyright owner. Enquiries should be sent to [email protected]. The Control of Substances Hazardous to Health Regulations 2002 refer to an ‘approved classification of a biological agent’, which means the classification of that agent approved by the Health and Safety Executive (HSE). This list is approved by HSE for that purpose. This edition of the Approved List has effect from 12 July 2021. On that date the previous edition of the list approved by the Health and Safety Executive on the 1 July 2013 will cease to have effect. This list will be reviewed periodically, the next review is due in February 2022. The Advisory Committee on Dangerous Pathogens (ACDP) prepares the Approved List included in this publication. ACDP advises HSE, and Ministers for the Department of Health and Social Care and the Department for the Environment, Food & Rural Affairs and their counterparts under devolution in Scotland, Wales & Northern Ireland, as required, on all aspects of hazards and risks to workers and others from exposure to pathogens. -

WILDLIFE DISEASES and HUMANS Robert G
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln The aH ndbook: Prevention and Control of Wildlife Wildlife Damage Management, Internet Center for Damage 11-29-1994 WILDLIFE DISEASES AND HUMANS Robert G. McLean Chief, Vertebrate Ecology Section, Medical Entomology & Ecology Branch, Division of Vector-borne Infectious, Diseases National Center for Infectious Diseases, Centers for Disease Control and Prevention, Fort Collins, Colorado McLean, Robert G., "WILDLIFE DISEASES AND HUMANS" (1994). The Handbook: Prevention and Control of Wildlife Damage. Paper 38. http://digitalcommons.unl.edu/icwdmhandbook/38 This Article is brought to you for free and open access by the Wildlife Damage Management, Internet Center for at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in The aH ndbook: Prevention and Control of Wildlife Damage by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Robert G. McLean Chief, Vertebrate Ecology Section Medical Entomology & Ecology Branch WILDLIFE DISEASES Division of Vector-borne Infectious Diseases National Center for Infectious Diseases AND HUMANS Centers for Disease Control and Prevention Fort Collins, Colorado 80522 INTRODUCTION GENERAL PRECAUTIONS Precautions against acquiring fungal diseases, especially histoplasmosis, Diseases of wildlife can cause signifi- Use extreme caution when approach- should be taken when working in cant illness and death to individual ing or handling a wild animal that high-risk sites that contain contami- animals and can significantly affect looks sick or abnormal to guard nated soil or accumulations of animal wildlife populations. Wildlife species against those diseases contracted feces; for example, under large bird can also serve as natural hosts for cer- directly from wildlife. -

Bacteriology
SECTION 1 High Yield Microbiology 1 Bacteriology MORGAN A. PENCE Definitions Obligate/strict anaerobe: an organism that grows only in the absence of oxygen (e.g., Bacteroides fragilis). Spirochete Aerobe: an organism that lives and grows in the presence : spiral-shaped bacterium; neither gram-positive of oxygen. nor gram-negative. Aerotolerant anaerobe: an organism that shows signifi- cantly better growth in the absence of oxygen but may Gram Stain show limited growth in the presence of oxygen (e.g., • Principal stain used in bacteriology. Clostridium tertium, many Actinomyces spp.). • Distinguishes gram-positive bacteria from gram-negative Anaerobe : an organism that can live in the absence of oxy- bacteria. gen. Bacillus/bacilli: rod-shaped bacteria (e.g., gram-negative Method bacilli); not to be confused with the genus Bacillus. • A portion of a specimen or bacterial growth is applied to Coccus/cocci: spherical/round bacteria. a slide and dried. Coryneform: “club-shaped” or resembling Chinese letters; • Specimen is fixed to slide by methanol (preferred) or heat description of a Gram stain morphology consistent with (can distort morphology). Corynebacterium and related genera. • Crystal violet is added to the slide. Diphtheroid: clinical microbiology-speak for coryneform • Iodine is added and forms a complex with crystal violet gram-positive rods (Corynebacterium and related genera). that binds to the thick peptidoglycan layer of gram-posi- Gram-negative: bacteria that do not retain the purple color tive cell walls. of the crystal violet in the Gram stain due to the presence • Acetone-alcohol solution is added, which washes away of a thin peptidoglycan cell wall; gram-negative bacteria the crystal violet–iodine complexes in gram-negative appear pink due to the safranin counter stain.