2008 Indiana Report of Infectious Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Official Nh Dhhs Health Alert
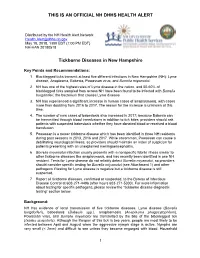
THIS IS AN OFFICIAL NH DHHS HEALTH ALERT Distributed by the NH Health Alert Network [email protected] May 18, 2018, 1300 EDT (1:00 PM EDT) NH-HAN 20180518 Tickborne Diseases in New Hampshire Key Points and Recommendations: 1. Blacklegged ticks transmit at least five different infections in New Hampshire (NH): Lyme disease, Anaplasma, Babesia, Powassan virus, and Borrelia miyamotoi. 2. NH has one of the highest rates of Lyme disease in the nation, and 50-60% of blacklegged ticks sampled from across NH have been found to be infected with Borrelia burgdorferi, the bacterium that causes Lyme disease. 3. NH has experienced a significant increase in human cases of anaplasmosis, with cases more than doubling from 2016 to 2017. The reason for the increase is unknown at this time. 4. The number of new cases of babesiosis also increased in 2017; because Babesia can be transmitted through blood transfusions in addition to tick bites, providers should ask patients with suspected babesiosis whether they have donated blood or received a blood transfusion. 5. Powassan is a newer tickborne disease which has been identified in three NH residents during past seasons in 2013, 2016 and 2017. While uncommon, Powassan can cause a debilitating neurological illness, so providers should maintain an index of suspicion for patients presenting with an unexplained meningoencephalitis. 6. Borrelia miyamotoi infection usually presents with a nonspecific febrile illness similar to other tickborne diseases like anaplasmosis, and has recently been identified in one NH resident. Tests for Lyme disease do not reliably detect Borrelia miyamotoi, so providers should consider specific testing for Borrelia miyamotoi (see Attachment 1) and other pathogens if testing for Lyme disease is negative but a tickborne disease is still suspected. -

Melioidosis: a Clinical Model for Gram-Negative Sepsis
J. Med. Microbiol. Ð Vol. 50 2001), 657±658 # 2001 The Pathological Society of Great Britain and Ireland ISSN 0022-2615 EDITORIAL Melioidosis: a clinical model for gram-negative sepsis The recently published study of recombinant human clinical sepsis model over the current heterogeneous activated protein C drotrecogin-á, Eli Lilly, Indiana- clinical trials. Our knowledge of melioidosis and its polis, IN, USA) in severe sepsis makes welcome causative organism, Burkholderia formerly Pseudomo- reading. At last a clinical trial of an augmentative nas) pseudomallei, has expanded considerably over the therapy in severe sepsis has managed to show a last 15 years. Melioidosis was originally described in mortality bene®t from the trial agent [1]. Most studies Myanmar then Burma) in 1911 and came to of augmentative treatments in serious sepsis have failed prominence during the Vietnam con¯ict, when French to show clear bene®t. Sepsis studies commonly involve and American soldiers became infected. It has been a syndrome caused by a myriad of organisms, occurring described in most countries of south-east Asia, in a very heterogeneous group of patients, who may be including the Peoples Republic of China and the Lao enrolled in one of several centres. This introduces PDR [5], but Thailand has the greatest reported disease multiple confounding factors. Agood model for clinical burden [6]. It is also endemic to northern Australia [7]. sepsis studies would ideally cause disease in a relatively Understanding of the epidemiology of the disease has homogeneous population, be acquired in a community been improved by the demonstration of two pheno- setting, present in large numbers to a single institution, typically similar but genetically distinct biotypes in the be caused by a single organism, and ordinarily result in environment [8], only one of which appears to be a substantial mortality rate. -

Are You Suprised ?
B DAMB 721 Microbiology Final Exam B 100 points December 11, 2006 Your name (Print Clearly): _____________________________________________ I. Matching: The questions below consist of headings followed by a list of phrases. For each phrase select the heading that best describes that phrase. The headings may be used once, more than once or not at all. Mark the answer in Part 2 of your answer sheet. 1. capsid 7. CD4 2. Chlamydia pneumoniae 8. Enterococcus faecalis 3. oncogenic 9. hyaluronidase 4. pyruvate 10. interferon 5. Koplik’s spot 11. hydrophilic viruses 6. congenital Treponema pallidum 12. Streptococcus pyogenes 1. “spreading factor” produced by members of the staphylococci, streptococci and clostridia 2. viral protein coat 3. central intermediate in bacterial fermentation 4. persistant endodontic infections 5. a cause of atypical pneumonia 6. nonspecific defense against viral infection 7. has a rudimentary life cycle 8. HIV receptor 9. Hutchinson’s Triad 10. measles 11. resistant to disinfection 12. β-hemolytic, bacitracin sensitive, cause of suppurative pharyngitis 2 Matching (Continued): The questions below consist of diseases followed by a list of etiologic agents. Match each disease with the etiologic agent. Continue using Part 2 of your answer sheet. 1. dysentery 6. Legionnaire’s 2. botulism 7. gas gangrene 3. cholera 8. tuberculosis 4. diphtheria 9. necrotizing fascitis 5. enteric fever 10. pneumoniae/meningitis 13. Clostridium botulinum 14. Vibrio cholera 15. Mycobacterium bovis 16. Shigella species 17. Streptococcus pneumoniae 18. Clostridium perfringens 19. Salmonella typhi 20. Streptococcus pyogenes 3 II. Multiple Choice: Choose the ONE BEST answer. Mark the correct answer on Part 1 of the answer sheet. -

Recognizing and Treating New and Emerging Infections Encountered in Everyday Practice
Recognizing and treating new and emerging infections encountered in everyday practice STEVEN M. GORDON, MD NFECTIOUS DISEASES, pre- MiikWirj:« Although infectious diseases were once considered a dicted earlier in this cen- diminishing threat, new pathogens are constantly challenging tury to be eliminated as a the health care system. This article reviews the clinical presen- public health problem, re- tation, diagnosis, and treatment of seven emerging infections I main the chief cause of death that primary care physicians are likely to encounter. worldwide and a significant cause of death and morbidity in i Parvovirus B19 attacks erythrocyte precursors; the United States.1 Challenging infection is usually benign and self-limiting but can cause the US public health system are aplastic crises in patients with chronic hemolytic disorders. several newly identified patho- Hemorrhagic colitis due to Escherichia coli 0157:H7 infection gens (eg, human immunodefi- can lead to the hemolytic-uremic syndrome, especially in chil- ciency virus [HIV], Escherichia dren; it also can cause thrombotic thrombocytopenia purpura. coli 0157:H7, hepatitis C) and a Chlamydia pneumoniae causes a mild pneumonia that resem- resurgence of old diseases pre- bles mycoplasmal pneumonia. Bacillary angiomatosis primar- sumed to be under control (eg, ily affects immunocompromised patients, especially those tuberculosis, syphilis). Further, infected with human immunodeficiency virus (HIV). At least multiple-drug resistance in two organisms can cause bacillary angiomatosis: Bartonella hense- strains of pneumococci, gono- lae and Bartonella quintana. Hantavirus pulmonary syndrome cocci, enterococci, staphylo- is spread by exposure to the droppings of infected rodents. cocci, salmonella, and mycobac- Contrary to previous thought, HIV continues to replicate teria undermines efforts to throughout the course of the illness and does not have a latency control the diseases they cause.2 phase. -

Invasive Group a Streptococcal Disease Communicable Disease Control Unit
Public Health and Primary Health Care Communicable Disease Control 4th Floor, 300 Carlton St, Winnipeg, MB R3B 3M9 T 204 788-6737 F 204 948-2040 www.manitoba.ca November, 2015 Re: Streptococcal Invasive Disease (Group A) Reporting and Case Investigation Reporting of Streptococcal invasive disease (Group A) (Streptococcus pyogenes) is as follows: Laboratory: All specimens isolated from sterile sites (refer to list below) that are positive for S. pyogenes are reportable to the Public Health Surveillance Unit by secure fax (204-948-3044). Health Care Professional: Probable (clinical) cases of Streptococcal invasive disease (Group A) are reportable to the Public Health Surveillance Unit using the Clinical Notification of Reportable Diseases and Conditions form (http://www.gov.mb.ca/health/publichealth/cdc/protocol/form13.pdf) ONLY if a positive lab result is not anticipated (e.g., poor or no specimen taken, person has recovered). Cooperation in Public Health investigation (when required) is appreciated. Regional Public Health or First Nations Inuit Health Branch (FNIHB): Cases will be referred to Regional Public Health or FNIHB. Completion and return of the Communicable Disease Control Investigation Form is generally not required, unless otherwise directed by a Medical Officer of Health. Sincerely, “Original Signed By” “Original Signed By” Richard Baydack, PhD Carla Ens, PhD Director, Communicable Disease Control Director, Epidemiology & Surveillance Public Health and Primary Health Care Public Health and Primary Health Care Manitoba Health, Healthy Living and Seniors Manitoba Health, Healthy Living and Seniors The sterile and non-sterile sites listed below represent commonly sampled body sites for the purposes of diagnosis, but the list is not exhaustive. -

Toxic Shock-Like Syndrome Associated with Necrotizing Streptococcus Pyogenes Infection
Henry Ford Hospital Medical Journal Volume 37 Number 2 Article 5 6-1989 Toxic Shock-like Syndrome Associated with Necrotizing Streptococcus Pyogenes Infection Thomas J. Connolly Donald J. Pavelka Eugene F. Lanspa Thomas L. Connolly Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Life Sciences Commons, Medical Specialties Commons, and the Public Health Commons Recommended Citation Connolly, Thomas J.; Pavelka, Donald J.; Lanspa, Eugene F.; and Connolly, Thomas L. (1989) "Toxic Shock- like Syndrome Associated with Necrotizing Streptococcus Pyogenes Infection," Henry Ford Hospital Medical Journal : Vol. 37 : No. 2 , 69-72. Available at: https://scholarlycommons.henryford.com/hfhmedjournal/vol37/iss2/5 This Article is brought to you for free and open access by Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Henry Ford Hospital Medical Journal by an authorized editor of Henry Ford Health System Scholarly Commons. Toxic Shock-like Syndrome Associated with Necrotizing Streptococcus Pyogenes Infection Thomas J. Connolly,* Donald J. Pavelka, MD,^ Eugene F. Lanspa, MD, and Thomas L. Connolly, MD' Two patients with toxic shock-like syndrome are presented. Bolh patients had necrotizing cellulitis due to Streptococcus pyogenes, and both patients required extensive surgical debridement. The association of Streptococcus pyogenes infection and toxic shock-like syndrome is discussed. (Henry Ford Hosp MedJ 1989:37:69-72) ince 1978, toxin-producing strains of Staphylococcus brought to the emergency room where a physical examination revealed S aureus have been implicated as the cause of the toxic shock a temperature of 40.9°C (I05.6°F), blood pressure of 98/72 mm Hg, syndrome (TSS), which is characterized by fever and rash and respiration of 36 breaths/min, and a pulse of 72 beats/min. -

Lyme Disease Weather Also Means That Ticks Become More Active and This Can Agent by Feeding As Larvae on Certain Rodent Species
Spring and summer bring warm temperatures, just right for small and medium sized animals, but will also feed on people. walking in the woods and other outdoor activities. Warm These ticks typically become infected with the Lyme disease weather also means that ticks become more active and this can agent by feeding as larvae on certain rodent species. increase the risk of a tick-borne disease. The tick-borne dis- In the fall, the nymphs become adults and infected nymphs eases that occur most often in Virginia are Lyme disease, become infected adults. Adult blacklegged ticks prefer to feed Rocky Mountain spotted fever, and ehrlichiosis. on deer. However, adult ticks will occasionally bite people on warm days of the fall and winter and can transmit Lyme disease Lyme Disease at that time. Lyme disease is caused by infection with a bacterium called Borrelia burgdorferi. The number of Lyme disease cases Transmission of Lyme disease by the nymph or adult ticks reported in Virginia has increased substantially in recent years. does not occur until the tick has been attached and feeding on a human or animal host for at least 36 hours. The Tick The blacklegged tick (Ixodes scapularis), formerly known as The Symptoms the deer tick, is the only carrier of Lyme disease in the Eastern Between three days to several weeks after being bitten by an U.S. The blacklegged tick's name comes from it being the only infected tick, 70-90% of people develop a circular or oval rash, tick in the Eastern U.S. that bites humans and has legs that are called erythema migrans (or EM), at the site of the bite. -

Kellie ID Emergencies.Pptx
4/24/11 ID Alert! recognizing rapidly fatal infections Susan M. Kellie, MD, MPH Professor of Medicine Division of Infectious Diseases, UNMSOM Hospital Epidemiologist UNMHSC and NMVAHCS Fever and…. Rash and altered mental status Rash Muscle pain Lymphadenopathy Hypotension Shortness of breath Recent travel Abdominal pain and diarrhea Case 1. The cross-country trucker A 30 year-old trucker driving from Oklahoma to California is hospitalized in Deming with fever and headache He is treated with broad-spectrum antibiotics, but deteriorates with obtundation, low platelet count, and a centrifugal petechial rash and is transferred to UNMH 1 4/24/11 What is your diagnosis? What is the differential diagnosis of fever and headache with petechial rash? (in the US) Tickborne rickettsioses ◦ RMSF Bacteria ◦ Neisseria meningitidis Key diagnosis in this case: “doxycycline deficiency” Key vector-borne rickettsioses treated with doxycycline: RMSF-case-fatality 5-10% ◦ Fever, nausea, vomiting, myalgia, anorexia and headache ◦ Maculopapular rash progresses to petechial after 2-4 days of fever ◦ Occasionally without rash Human granulocytotropic anaplasmosis (HGA): case-fatality<1% Human monocytotropic ehrlichiosis (HME): case fatality 2-3% 2 4/24/11 Lab clues in rickettsioses The total white blood cell (WBC) count is typicallynormal in patients with RMSF, but increased numbers of immature bands are generally observed. Thrombocytopenia, mild elevations in hepatic transaminases, and hyponatremia might be observed with RMSF whereas leukopenia -

Melioidosis in Birds and Burkholderia Pseudomallei Dispersal, Australia
LETTERS 5. Mätz-Rensing K, Jentsch KD, Rensing S, Melioidosis in Birds However, these are mostly birds Langenhuynsen S, Verschoor E, Niphuis in captivity and often exotic to the H, et al. Fatal herpes simplex infection in and Burkholderia a group of common marmosets (Callithrix location, suggesting potential reduced jacchus). Vet Pathol. 2003;40:405–11. pseudomallei immunity. Little is known about doi:10.1354/vp.40-4-405 Dispersal, Australia melioidosis in wild birds. In Sabah, 6. Bruno SF, Liebhold M, Mätz-Rensing K, Malaysia, only 1 of 440 wild birds Romão MA, Didier A, Brandes A, et al. Herpesvirus infection in free-living black- To the Editor: Melioidosis is an admitted to a research center over 9 tufted-ear marmoset (Callithrix penicil- emerging infectious disease of humans years was found to have melioidosis lata E. Geoffroyi 1812) at the state park of and animals caused by the gram- (6). Serra da Tiririca, Niterói, Rio de Janeiro, negative bacterium Burkholderia Although birds are endotherms, Brazil. Berl Munch Tierarztl Wochenschr. 1997;110:427–30. pseudomallei, which inhabits soil and with high metabolic rates and body 7. Kalter SS, Heberling RL. Comparative surface water in the disease-endemic temperature (40°C–43°C) protecting virology of primates. Bacteriol Rev. regions of Southeast Asia and northern them from many diseases, some birds 1971;35:310–64. Australia (1). The aim of this study appear more susceptible to melioidosis. 8. Mansfi eld K. Emerging and re-emerging infectious diseases of nonhuman primates. was to assess the potential for birds Indeed, high body temperature would Proceedings of the American College to spread B. -

Anaplasmosis: an Emerging Tick-Borne Disease of Importance in Canada
IDCases 14 (2018) xxx–xxx Contents lists available at ScienceDirect IDCases journal homepage: www.elsevier.com/locate/idcr Case report Anaplasmosis: An emerging tick-borne disease of importance in Canada a, b,c d,e e,f Kelsey Uminski *, Kamran Kadkhoda , Brett L. Houston , Alison Lopez , g,h i c c Lauren J. MacKenzie , Robbin Lindsay , Andrew Walkty , John Embil , d,e Ryan Zarychanski a Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, University of Manitoba, Winnipeg, MB, Canada b Cadham Provincial Laboratory, Government of Manitoba, Winnipeg, MB, Canada c Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Medical Microbiology and Infectious Diseases, University of Manitoba, Winnipeg, MB, Canada d Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, Section of Medical Oncology and Hematology, University of Manitoba, Winnipeg, MB, Canada e CancerCare Manitoba, Department of Medical Oncology and Hematology, Winnipeg, MB, Canada f Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Pediatrics and Child Health, Section of Infectious Diseases, Winnipeg, MB, Canada g Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Internal Medicine, Section of Infectious Diseases, University of Manitoba, Winnipeg, MB, Canada h Rady Faculty of Health Sciences, Max Rady College of Medicine, Department of Community Health Sciences, University of Manitoba, Winnipeg, MB, Canada i Public Health Agency of Canada, National Microbiology Laboratory, Zoonotic Diseases and Special Pathogens, Winnipeg, MB, Canada A R T I C L E I N F O A B S T R A C T Article history: Human Granulocytic Anaplasmosis (HGA) is an infection caused by the intracellular bacterium Received 11 September 2018 Anaplasma phagocytophilum. -

2012 Case Definitions Infectious Disease
Arizona Department of Health Services Case Definitions for Reportable Communicable Morbidities 2012 TABLE OF CONTENTS Definition of Terms Used in Case Classification .......................................................................................................... 6 Definition of Bi-national Case ............................................................................................................................................. 7 ------------------------------------------------------------------------------------------------------- ............................................... 7 AMEBIASIS ............................................................................................................................................................................. 8 ANTHRAX (β) ......................................................................................................................................................................... 9 ASEPTIC MENINGITIS (viral) ......................................................................................................................................... 11 BASIDIOBOLOMYCOSIS ................................................................................................................................................. 12 BOTULISM, FOODBORNE (β) ....................................................................................................................................... 13 BOTULISM, INFANT (β) ................................................................................................................................................... -

Illness Reporting Log for Temporary Events and Volunteers
1020 6th Street SE Cedar Rapids, IA 52401 PH: 319-892-6000 www.linncounty.org/603/Food-Safety REPORTING OF ILLNESS FORM Worker Sign-in Sheet The purpose of this form is to inform food workers of their responsibility to notify the person in charge when they experience any of the health conditions listed below. The person in charge must take appropriate steps to prevent the transmission of foodborne illness. I AGREE TO REPORT TO THE PERSON IN CHARGE: Any onset of the following symptoms, either while at work or outside of work, including the onset date: 1. Diarrhea 2. Vomiting 3. Jaundice 4. Sore throat with fever 5. Infected cuts or wounds, or lesions containing pus on the hand, wrist , an exposed body part, or other body part and the cuts, wounds, or lesions are not properly covered (such as boils and infected wounds, however small) Medical Diagnosis: Whenever diagnosed as being ill with Norovirus, typhoid fever (Salmonella Typhi), non-typhoidal Salmonella, shigellosis (Shigella spp. infection), Escherichia coil 0157:H7 or other Enterohemorrhagic (EHEC) or Shiga toxin-producing Escherichia coli (STEC) infection or Hepatitis A (hepatitis A virus infection) Exposure to Foodborne Pathogens: 1. Exposure to or suspicion of causing any confirmed disease outbreak of Norovirus, typhoid fever, shigellosis, E. coli 0157:H7 or other Enterohemorrhagic (EHEC) or Shiga toxin-producing Escherichia coli (STEC) infection, or Hepatitis A. 2. A household member diagnosed with Norovirus, typhoid fever, shigellosis, E. coli 0157:H7 or other Enterohemorrhagic (EHEC) or Shiga toxin-producing Escherichia coli (STEC) infection, or Hepatitis A. 3. A household member attending or working in a setting experiencing a confirmed disease outbreak of Norovirus, typhoid fever, shigellosis, E.