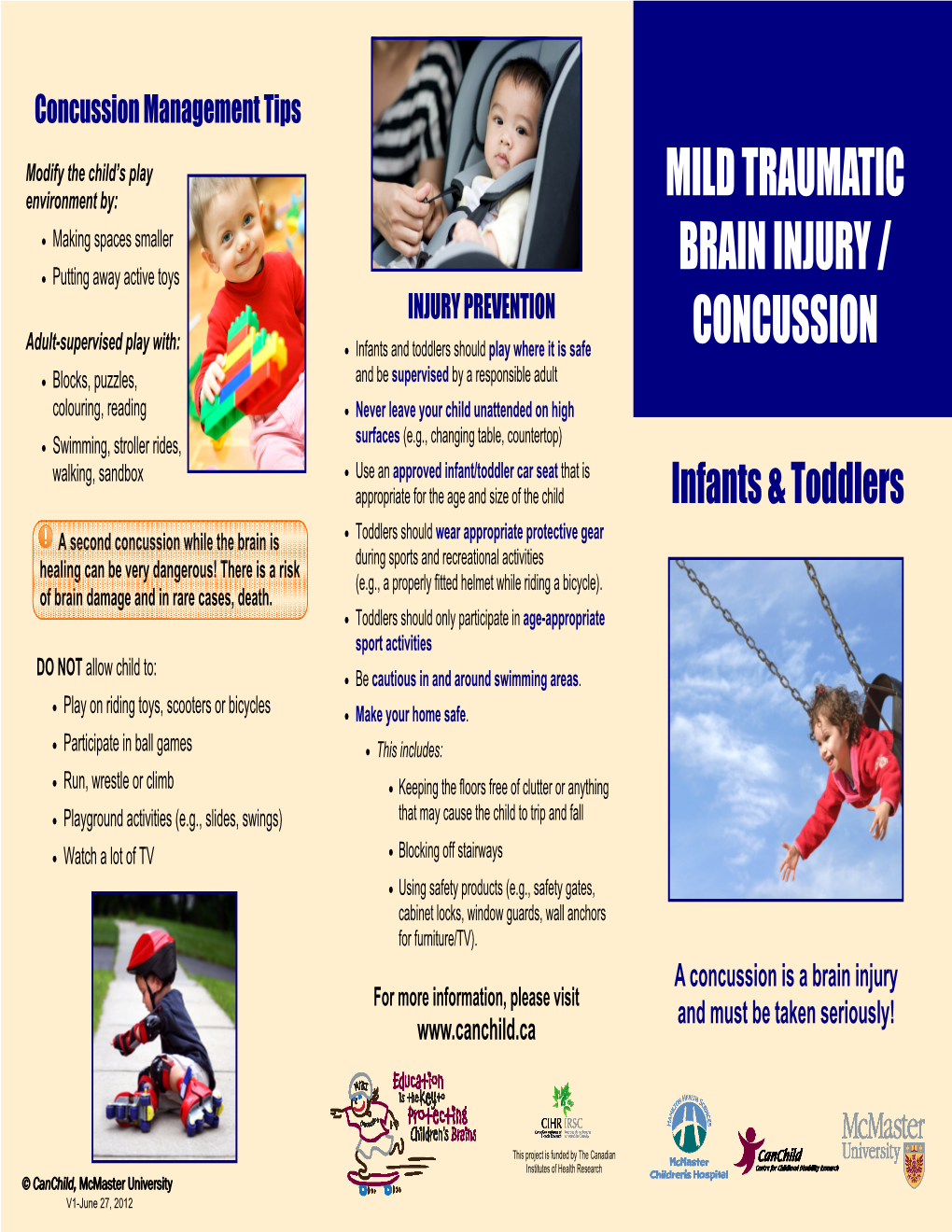
Mild Traumatic Brain Injury/Concussion
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Growing, Moving, Learning – Infant Toddler Toolkit
Growing, Moving, Learning Infant Toddler Toolkit May 2011 NOTICE: The University of Delaware does not discriminate on the basis of race, color, national origin, sex, disability, or age in its programs and activities. The following person has been designated to handle inquiries regarding the non-discrimination policies and to serve as the overall campus coordinator for purposes of Title IX compliance: Name and Title: Becki Fogerty Director, Office of Equity and Inclusion Address: 305 Hullihen Hall University of Delaware Newark, DE 19716 Telephone No.: (302) 831-8063 The following person has been designed to handle inquiries regarding the non-discrimination policies as those policies apply to the University’s Division of Intercollegiate Athletics and Recreation Services: Name and Title: Jennifer W. Davis Vice President for Finance and Administration Address: 220 Hullihen Hall University of Delaware Newark, DE 19716 Telephone: (302) 831-2769 Inquiries concerning the application of Title IX may be referred to the appropriate Title IX coordinator or to the Office for Civil Rights, United States Department of Education. For further information on notice of non-discrimination, visit http://wdcrobcolp01.ed.gov/CFAPPS/OCR/contactus.cfm for the address and phone number of the U.S. Department of Education office that serves your areas, or call (800) 421-3481. Acknowledgements We would like to acknowledge Penny Deiner, Ph.D., Professor Emerita and past Chair of the Department of Human Development and Family Studies, at the University of Delaware as the original author of the Infant Toddler Toolkit for Healthy Eating and Physical Activity. Dr. Deiner developed and piloted the original activities jointly with Nemours Health and Prevention Services. -

What to Expect After Having a Subarachnoid Hemorrhage (SAH) Information for Patients and Families Table of Contents
What to expect after having a subarachnoid hemorrhage (SAH) Information for patients and families Table of contents What is a subarachnoid hemorrhage (SAH)? .......................................... 3 What are the signs that I may have had an SAH? .................................. 4 How did I get this aneurysm? ..................................................................... 4 Why do aneurysms need to be treated?.................................................... 4 What is an angiogram? .................................................................................. 5 How are aneurysms repaired? ..................................................................... 6 What are common complications after having an SAH? ..................... 8 What is vasospasm? ...................................................................................... 8 What is hydrocephalus? ............................................................................... 10 What is hyponatremia? ................................................................................ 12 What happens as I begin to get better? .................................................... 13 What can I expect after I leave the hospital? .......................................... 13 How will the SAH change my health? ........................................................ 14 Will the SAH cause any long-term effects? ............................................. 14 How will my emotions be affected? .......................................................... 15 When should -

What%Is%Epilepsy?%
What%is%Epilepsy?% Epilepsy(is(a(brain(disorder(in(which(a(person(has(repeated(seizures((convulsions)(over(time.(Seizures(are( episodes(of(disturbed(brain(activity(that(cause(changes(in(attention(or(behavior.( Causes( Epilepsy(occurs(when(permanent(changes(in(brain(tissue(cause(the(brain(to(be(too(excitable(or(jumpy.( The(brain(sends(out(abnormal(signals.(This(results(in(repeated,(unpredictable(seizures.((A(single(seizure( that(does(not(happen(again(is(not(epilepsy.)( Epilepsy(may(be(due(to(a(medical(condition(or(injury(that(affects(the(brain,(or(the(cause(may(be( unknown((idiopathic).( Common(causes(of(epilepsy(include:( •Stroke(or(transient(ischemic(attack((TIA)( •Dementia,(such(as(Alzheimer's(disease( •Traumatic(brain(injury( •Infections,(including(brain(abscess,(meningitis,(encephalitis,(and(AIDS( •Brain(problems(that(are(present(at(birth((congenital(brain(defect)( •Brain(injury(that(occurs(during(or(near(birth( •Metabolism(disorders(present(at(birth((such(as(phenylketonuria)( •Brain(tumor( •Abnormal(blood(vessels(in(the(brain( •Other(illness(that(damage(or(destroy(brain(tissue( •Use(of(certain(medications,(including(antidepressants,(tramadol,(cocaine,(and(amphetamines( Epilepsy(seizures(usually(begin(between(ages(5(and(20,(but(they(can(happen(at(any(age.(There(may(be(a( family(history(of(seizures(or(epilepsy.( Symptoms( Symptoms(vary(from(person(to(person.(Some(people(may(have(simple(staring(spells,(while(others(have( violent(shaking(and(loss(of(alertness.(The(type(of(seizure(depends(on(the(part(of(the(brain(affected(and( cause(of(epilepsy.( -

Pediatric Respiratory Rates Age Rate (Breaths Per Minute)
Pediatric Respiratory Rates Age Rate (breaths per minute) Infant (birth–1 year) 30–60 Toddler (1–3 years) 24–40 Preschooler (3–6 years) 22–34 School-age (6–12 years) 18–30 Adolescent (12–18 years) 12–16 Pediatric Pulse Rates Age Low High Infant (birth–1 year) 100 160 Toddler (1–3 years) 90 150 Preschooler (3–6 years) 80 140 School-age (6–12 years) 70 120 Adolescent (12–18 years) 60 100 Pulse rates for a child who is sleeping may be 10 percent lower than the low rate listed. Low-Normal Pediatric Systolic Blood Pressure Age* Low Normal Infant (birth–1 year) greater than 60* Toddler (1–3 years) greater than 70* Preschooler (3–6 years) greater than 75 School-age (6–12 years) greater than 80 Adolescent (12–18 years) greater than 90 *Note: In infants and children aged three years or younger, the presence of a strong central pulse should be substituted for a blood pressure reading. Pediatric CUPS Assessment Category Assessment Actions Example Critical Absent airway, Perform rapid initial Severe traumatic injury breathing, or interventions and transport with respiratory arrest or circulation simultaneously cardiac arrest Unstable Compromised airway, Perform rapid initial Significant injury with breathing, or interventions and transport respiratory distress, circulation with simultaneously active bleeding, shock; altered mental status near-drowning; unresponsiveness Potentially Normal airway, Perform initial assessment Minor fractures; unstable breathing, circulation, with interventions; transport pedestrian struck by car and mental status BUT -

ACT Early Milestone Moments
Milestone Moments Learn the Signs. Act Early. Learn the Signs. Act Early. www.cdc.gov/milestones 1-800-CDC-INFO Adapted from CARING FOR YOUR BABY AND YOUNG CHILD: BIRTH TO AGE 5, Fifth Edition, edited by Steven Shelov and Tanya Remer Altmann © 1991, 1993, 1998, 2004, 2009 by the American Academy of Pediatrics and You can follow your child’s development by watching how he or BRIGHT FUTURES: GUIDELINES FOR HEALTH SUPERVISION OF INFANTS, CHILDREN, AND ADOLESCENTS, Third she plays, learns, speaks, and acts. Edition, edited by Joseph Hagan, Jr., Judith S. Shaw, and Paula M. Duncan, 2008, Elk Grove Village, IL: American Academy of Pediatrics. Special acknowledgements to Susan P. Berger, PhD; Jenny Burt, PhD; Margaret Greco, MD; Katie Green, MPH, Look inside for milestones to watch for in your child and how you CHES; Georgina Peacock, MD, MPH; Lara Robinson, PhD, MPH; Camille Smith, MS, EdS; Julia Whitney, BS; and can help your child learn and grow. Rebecca Wolf, MA. Centers for Disease Centers for Disease Control and Prevention Control and Prevention www.cdc.gov/milestones www.cdc.gov/milestones 1-800-CDC-INFO 1-800-CDC-INFO 220788 Milestone Moments How your child plays, learns, speaks, and acts offers important clues about your child’s development. Developmental milestones are things most children can do by a certain age. The lists that follow have milestones to look for when your child is: 2 Months ............................................................... page 3 – 6 Check the milestones your child has reached at each age. 4 Months ............................................................... page 7 –10 Take this with you and talk with your child’s doctor at every visit about the milestones your child has reached and what to 6 Months .............................................................. -

Brain Injury and Opioid Overdose
Brain Injury and Opioid Overdose: Acquired Brain Injury is damage to the brain 2.8 million brain injury related occurring after birth and is not related to congenital or degenerative disease. This includes anoxia and hospital stays/deaths in 2013 hypoxia, impairment (lack of oxygen), a condition consistent with drug overdose. 70-80% of hospitalized patients are discharged with an opioid Rx Opioid Use Disorder, as defined in DSM 5, is a problematic pattern of opioid use leading to clinically significant impairment, manifested by meaningful risk 63,000+ drug overdose-related factors occurring within a 12-month period. deaths in 2016 Overdose is injury to the body (poisoning) that happens when a drug is taken in excessive amounts “As the number of drug overdoses continues to rise, and can be fatal. Opioid overdose induces respiratory doctors are struggling to cope with the increasing number depression that can lead to anoxic or hypoxic brain of patients facing irreversible brain damage and other long injury. term health issues.” Substance Use and Misuse is: The frontal lobe is • Often a contributing factor to brain injury. History of highly susceptible abuse/misuse is common among individuals who to brain oxygen have sustained a brain injury. loss, and damage • Likely to increase for individuals who have misused leads to potential substances prior to and post-injury. loss of executive Acute or chronic pain is a common result after brain function. injury due to: • Headaches, back or neck pain and other musculo- Sources: Stojanovic et al 2016; Melton, C. Nov. 15,2017; Devi E. skeletal conditions commonly reported by veterans Nampiaparampil, M.D., 2008; Seal K.H., Bertenthal D., Barnes D.E., et al 2017; with a history of brain injury. -

Living with Infants, Toddlers, and Children Who Have Been Prenatally Exposed to Alcohol
Living with Infants, Toddlers, and Children who have been Prenatally Exposed to Alcohol This section includes practical information about what to look for and how to successfully deal with your infant, toddler, or child who has been affected by prenatal alcohol exposure. Much of the information comes directly from parent experiences. Also included is information that we encourage you to copy and share with your child's teachers and other caregivers. It is crucial for everyone involved in the care and education of a child with disabilities to remember that they are first a child and second, a child with a disability. Children with FAS or ARND, like all children, will move through various stages of normal development. They may not move as quickly or as distinctly, but they will move and grow. With growth come struggles and challenges. A typically developing child may demonstrate some of the behaviors described in this section, but because he or she does not present a disability, their behavior is dealt with and accepted as a normal part of growing up. Conversely, children with disabilities often display appropriate or typically challenging behaviors for a child at their developmental level, but because they have a disability, their behavior becomes amplified by those who are working with and caring for them. Because this happens so frequently and unconsciously, readers are urged to balance their perceptions of their child's behavior with their knowledge and experience of normal/typical child development and behavior. � How Parents Can Help -

Traumatic Brain Injury and Domestic Violence
TRAUMATIC BRAIN INJURY AND DOMESTIC VIOLENCE Women who are abused often suffer injury to their head, neck, and face. The high potential for women who are abused to have mild to severe Traumatic Brain Injury (TBI) is a growing concern, since the effects can cause irreversible psychological and physical harm. Women who are abused are more likely to have repeated injuries to the head. As injuries accumulate, likelihood of recovery dramatically decreases. In addition, sustaining another head trauma prior to the complete healing of the initial injury may be fatal. Severe, obvious trauma does not have to occur for brain injury to exist. A woman can sustain a blow to the head without any loss of consciousness or apparent reason to seek medical assistance, yet display symptoms of TBI. (NOTE: While loss of consciousness can be significant in helping to determine the extent of the injury, people with minor TBI often do not lose consciousness, yet still have difficulties as a result of their injury). Many women suffer from a TBI unknowingly and misdiagnosis is common since symptoms may not be immediately apparent and may mirror those of mental health diagnoses. In addition, subtle injuries that are not identifiable through MRIs or CT scans may still lead to cognitive symptoms. What is Traumatic Brain Injury? Traumatic brain injury (TBI) is defined as an injury to the brain that is caused by external physical force and is not present at birth or degenerative. TBI can be caused by: • A blow to the head, o e.g., being hit on the head forcefully with object or fist, having one’s head smashed against object/wall, falling and hitting head, gunshot to head. -

Typical Child Development
TYPICAL CHILD DEVELOPMENT ADOLESCENTS Physical • Rapid growth, maturity of sexual organs, development of secondary sexual characteristics • Girls generally physically mature before boys • Learning to accept changes in their bodies and adapt their behavior based on these changes Cognitive • Begin to think hypothetically and see different points of view • During middle and late adolescents the ability to see multiple perspectives is refined Social • Group values guide individual behavior. In early adolescence most peer groups are still same sex • Become interested in sexual relationships but most contact is through groups. May begin to experiment in sexual behavior • In early adolescence social roles still largely defined by external sources • During middle and late adolescence • Choose friends based on personal characteristics and mutual interest. Peer group declines in interest. • Experiment with social roles and explore options for career choices Emotional • Depend upon peers for emotional stability, support and to help mold their emerging identities • Self-esteem greatly affected by acceptance of peers • Early adolescents are moody, dramatic and very vulnerable to emotional stress • Middle and late adolescence, identity is more individualized and a sense of self develops and stabilizes • Self- esteem in middle and late adolescence is influenced by his/her ability to live up to internalized standards for behavior SCHOOL AGE Physical • The ability to sit still and attend increases as they move through this stage • Practice, refine, and -

Traumatic Brain Injury (TBI)
Traumatic Brain Injury (TBI) Carol A. Waldmann, MD raumatic brain injury (TBI), caused either by blunt force or acceleration/ deceleration forces, is common in the general population. Homeless persons Tare at particularly high risk of head trauma and adverse outcomes to TBI. Even mild traumatic brain injury can lead to persistent symptoms including cognitive, physical, and behavioral problems. It is important to understand brain injury in the homeless population so that appropriate referrals to specialists and supportive services can be made. Understanding the symptoms and syndromes caused by brain injury sheds light on some of the difficult behavior observed in some homeless persons. This understanding can help clinicians facilitate and guide the care of these individuals. Prevalence and Distribution recover fully, but up to 15% of patients diagnosed TBI and Mood Every year in the USA, approximately 1.5 with MTBI by a physician experience persistent Swings. million people sustain traumatic brain injury disabling problems. Up to 75% of brain injuries This man suffered (TBI), 230,000 people are hospitalized due to TBI are classified as MTBI. These injuries cost the US a gunshot wound and survive, over 50,000 people die from TBI, and almost $17 billion per year. The groups most at risk to the head and many subsequent more than 1 million people are treated in emergency for TBI are those aged 15-24 years and those aged traumatic brain rooms for TBI. In persons under the age of 45 years, 65 years and older. Men are twice as likely to sustain injuries while TBI is the leading cause of death. -

Child Development-Prenatal-Toddler
St. Michael-Albertville High School Child Development Prenatal Through Toddler Teacher: Christie Larson September 2021 Content Skills Learning Targets Assessment Resources & Technology CEQ: WHAT ARE THE BENEFITS OF STUDYING CHILD DEVELOPMENT? UEQ: Unit 1 Learning About Children • What are the three areas of child development? •What are the reasons for studying children? •What are the principles of growth and development? • Who are some leading child development theorists? National Standards: 13.5.1 13.5.2 Child and Human Development Framework MCHD 2.1 MCHD 3.4 www.curriculummapper.com 113 Larson Child Development Prenatal Through Toddler St. Michael-Albertville High School A: Learning About A: Learning About A: Learning About A: Learning About A: Learning About Children Children Children Children Children A1: 3 developmental areas A1: Identify the three areas LT1: I can describe reasons A1: Development Poster A2: Reasons for studying of Child Development for studying children. A1: Ch. 1 "The Subject "Children:The Early Years, children. A2. Describe reasons for Matter of Child 2011" Chapter 1: Learning A3: Influences on studying children LT2: I can describe the Development" About Children development A3: Identify and describe factors that promote or A2: Ch. 1 "Parent's Aid in A4: Leading child the factors that promote inhibit growth and Growth and Development" "Developmental Theorists" development theorists growth and development development. WS DVD A4: Identify the leading A2: Ch. 1, "Individual Life theorists of child LT3: I can explain how Cycle" WS Chapter 1 VOCAB: Development (Maslow, brain development occurs. A3: Ch. 1 "Principles of Child Development Piaget, Erickson, and other Growth and Development" Intellectual Development current theorists) LT4: I can explain the WS Social-Emotional major principles and A3: Ch. -

Rapidly Progressive Tetraplegia and Cognitive Deterioration During Rehabilitation: a Case of Neurodegenerative Disease
J Surg Med. 2019;3(1):100-102. Case report DOI: 10.28982/josam.454181 Olgu sunumu Rapidly progressive tetraplegia and cognitive deterioration during rehabilitation: A case of neurodegenerative disease Rehabilitasyon sırasında hızlı ilerleyen tetrapleji ve bilişsel bozulma: Bir nörodejeneratif hastalık olgusu Sevgi İkbali Afşar 1, Oya Ümit Yemişçi 1 1 Department of Physical Medicine and Abstract Rehabilitation, Baskent University, Human prion diseases are fatal, progressive neurodegenerative disorders caused by neurolytic pathogen proteins, called Faculty of Medicine, Ankara, Turkey prions. The most common human prion disease is sporadic Creutzfeldt-Jakob disease, with an approximate annual prevalence of 0.5-1 per million. The symptoms and signs include rapidly progressive dementia, ataxia, myoclonic ORCID ID of the authors SİA: 0000-0002-4003-3646 seizures, akinetic mutism and other neurological and neurobehavioral disorders. The clinical spectrum of Creutzfeldt- OÜY: 0000-0002-0501-5127 Jakob disease is highly variable; therefore it can be difficult to diagnose premortem. This article describes a 78-year- old woman who initially presented with difficulty walking and balance disorder. As a result of the evaluation, the patient was transferred to rehabilitation clinic, with a diagnosis of cervical spinal stenosis. During hospitalization, she showed progressive decline in gait and balance and deteriorated rapidly. The patient was considered to be probable sporadic Creutzfeldt-Jakob disease after further investigations. Keywords: Neurodegenerative disease, Creutzfeldt-Jakob disease, Rehabilitation Öz Corresponding author / Sorumlu yazar: İnsan prion hastalıkları, prionlar olarak adlandırılan nörolitik patojen proteinlerin neden olduğu ilerleyici Sevgi İkbali Afşar Address / Adres: Fevzi Cakmak Cad. 5. Sokak nörodejeneratif hastalıklardır. En yaygın insan prion hastalığı sporadik Creutzfeldt-Jakob hastalığı olup, yıllık No: 48, 06490, Ankara, Türkiye prevalansı yaklaşık milyonda 0.5-1'dir.