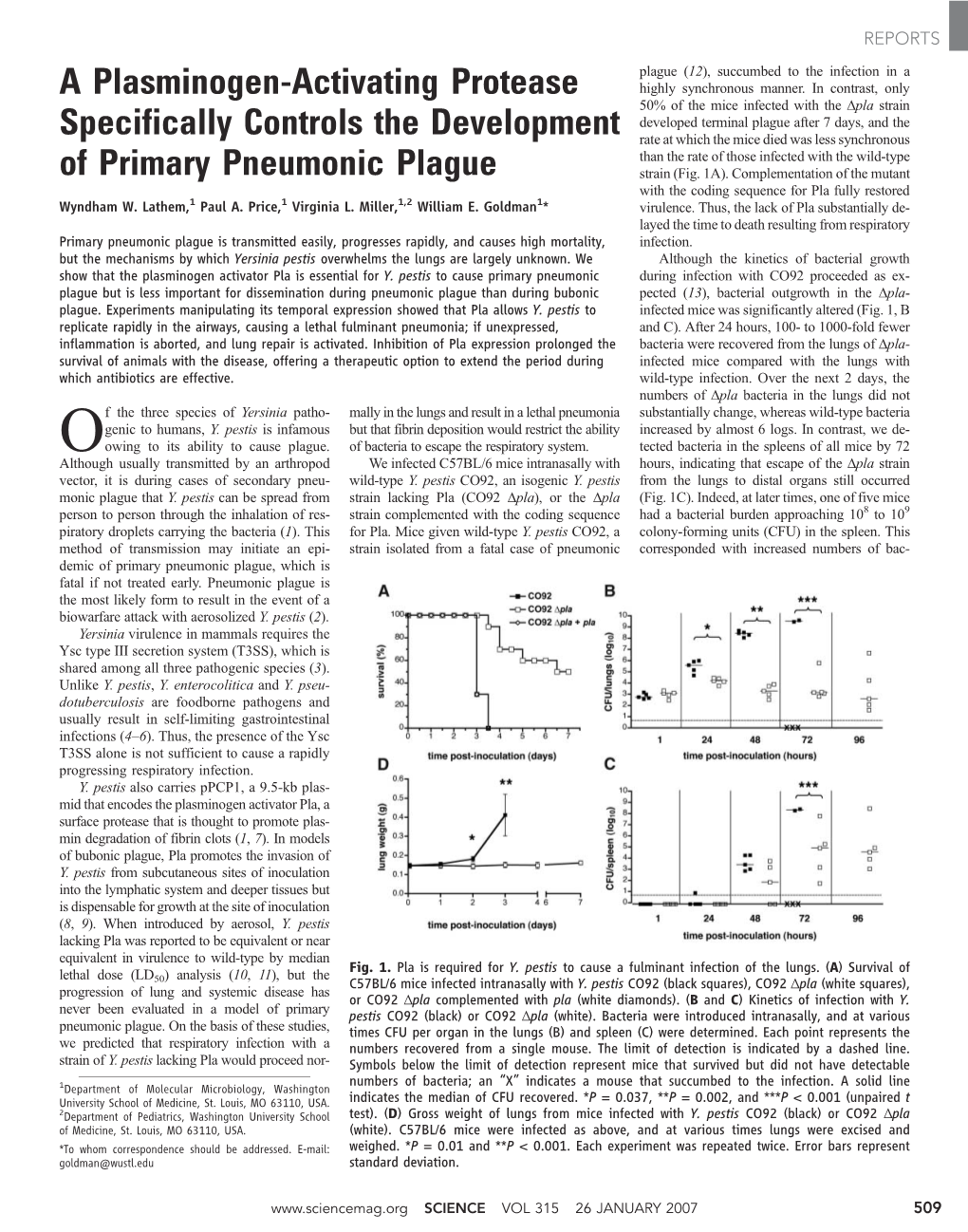
A Plasminogen-Activating Protease Specifically Controls The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Investigations on the Occurrence of Fungal Root Endophytes and an Associated Mycovirus in Context with Apple Replant Disease
Investigations on the occurrence of fungal root endophytes and an associated mycovirus in context with apple replant disease Von der Naturwissenschaftlichen Fakultät der Gottfried Wilhelm Leibniz Universität Hannover zur Erlangung des Grades Doktorin der Gartenbauwissenschaften (Dr. rer. hort.) genehmigte Dissertation von Gösta Carolin Dorette Popp, M. Sc. 2020 Referent: Prof. Dr. Edgar Maiss Korreferentin: Prof. Dr. Traud Winkelmann Tag der Promotion: 12.08.2020 Abstract I Abstract Apple replant disease (ARD) negatively affects the production in nurseries and orchards worldwide. A biotic cause of the disease is most likely since soil disinfection can restore plant growth. Fungi have appeared to contribute to the complex of biotic factors, but up to now the actual cause of the disease remains unknown. Further, environmentally friendly and practically applicable mitigation strategies are missing. Fungal root endophytes were isolated in two central experiments of the ORDIAmur consortium. Dark septate endophytes (Leptodontidium spp.) were frequently isolated from apple roots. An abundant occurrence of Nectriaceae fungi (Dactylonectria torresensis and Ilyonectria robusta) was found in ARD roots. Reference sites displayed a different characteristic fungal community. In roots grown in irradiated soil, a reduction of the number of isolated fungi and a changed composition of the fungal community was found. To investigate the effect of fungal endophytes on apple plants a quick and soil-free bio test in Petri dishes was developed using perlite. Inoculated fungi isolated from ARD roots induced neutral (Plectosphaerella, Pleotrichocladium, and Zalerion) to negative (Cadophora, Calonectria, Dactylonectria, Ilyonectria, and Leptosphaeria) plant reactions. After re-isolation, most of the Nectriaceae isolates were confirmed as pathogens. Microscopic analyses of ARD-affected roots revealed necroses caused by an unknown fungus that forms cauliflower-like (CF) structures in diseased cortex cells. -

Australia Biodiversity of Biodiversity Taxonomy and and Taxonomy Plant Pathogenic Fungi Fungi Plant Pathogenic
Taxonomy and biodiversity of plant pathogenic fungi from Australia Yu Pei Tan 2019 Tan Pei Yu Australia and biodiversity of plant pathogenic fungi from Taxonomy Taxonomy and biodiversity of plant pathogenic fungi from Australia Australia Bipolaris Botryosphaeriaceae Yu Pei Tan Curvularia Diaporthe Taxonomy and biodiversity of plant pathogenic fungi from Australia Yu Pei Tan Yu Pei Tan Taxonomy and biodiversity of plant pathogenic fungi from Australia PhD thesis, Utrecht University, Utrecht, The Netherlands (2019) ISBN: 978-90-393-7126-8 Cover and invitation design: Ms Manon Verweij and Ms Yu Pei Tan Layout and design: Ms Manon Verweij Printing: Gildeprint The research described in this thesis was conducted at the Department of Agriculture and Fisheries, Ecosciences Precinct, 41 Boggo Road, Dutton Park, Queensland, 4102, Australia. Copyright © 2019 by Yu Pei Tan ([email protected]) All rights reserved. No parts of this thesis may be reproduced, stored in a retrieval system or transmitted in any other forms by any means, without the permission of the author, or when appropriate of the publisher of the represented published articles. Front and back cover: Spatial records of Bipolaris, Curvularia, Diaporthe and Botryosphaeriaceae across the continent of Australia, sourced from the Atlas of Living Australia (http://www.ala. org.au). Accessed 12 March 2019. Taxonomy and biodiversity of plant pathogenic fungi from Australia Taxonomie en biodiversiteit van plantpathogene schimmels van Australië (met een samenvatting in het Nederlands) Proefschrift ter verkrijging van de graad van doctor aan de Universiteit Utrecht op gezag van de rector magnificus, prof. dr. H.R.B.M. Kummeling, ingevolge het besluit van het college voor promoties in het openbaar te verdedigen op donderdag 9 mei 2019 des ochtends te 10.30 uur door Yu Pei Tan geboren op 16 december 1980 te Singapore, Singapore Promotor: Prof. -

A Worldwide List of Endophytic Fungi with Notes on Ecology and Diversity
Mycosphere 10(1): 798–1079 (2019) www.mycosphere.org ISSN 2077 7019 Article Doi 10.5943/mycosphere/10/1/19 A worldwide list of endophytic fungi with notes on ecology and diversity Rashmi M, Kushveer JS and Sarma VV* Fungal Biotechnology Lab, Department of Biotechnology, School of Life Sciences, Pondicherry University, Kalapet, Pondicherry 605014, Puducherry, India Rashmi M, Kushveer JS, Sarma VV 2019 – A worldwide list of endophytic fungi with notes on ecology and diversity. Mycosphere 10(1), 798–1079, Doi 10.5943/mycosphere/10/1/19 Abstract Endophytic fungi are symptomless internal inhabits of plant tissues. They are implicated in the production of antibiotic and other compounds of therapeutic importance. Ecologically they provide several benefits to plants, including protection from plant pathogens. There have been numerous studies on the biodiversity and ecology of endophytic fungi. Some taxa dominate and occur frequently when compared to others due to adaptations or capabilities to produce different primary and secondary metabolites. It is therefore of interest to examine different fungal species and major taxonomic groups to which these fungi belong for bioactive compound production. In the present paper a list of endophytes based on the available literature is reported. More than 800 genera have been reported worldwide. Dominant genera are Alternaria, Aspergillus, Colletotrichum, Fusarium, Penicillium, and Phoma. Most endophyte studies have been on angiosperms followed by gymnosperms. Among the different substrates, leaf endophytes have been studied and analyzed in more detail when compared to other parts. Most investigations are from Asian countries such as China, India, European countries such as Germany, Spain and the UK in addition to major contributions from Brazil and the USA. -

Plant Host and Drought Shape the Root Associated Fungal Microbiota in Rice
Plant host and drought shape the root associated fungal microbiota in rice Beatriz Andreo-Jimenez1,2, Philippe Vandenkoornhuyse3, Amandine Lê Van3, Arvid Heutinck1, Marie Duhamel3,4, Niteen Kadam5, Krishna Jagadish5,6, Carolien Ruyter-Spira1 and Harro Bouwmeester1,7 1 Laboratory of Plant Physiology, Wageningen University, Wageningen, Netherlands 2 Biointeractions & Plant Health Business Unit, Wageningen University & Research, Wageningen, Netherlands 3 EcoBio, Université Rennes I, Rennes, France 4 IBL Plant Sciences and Natural Products, Leiden University, Leiden, Netherlands 5 International Rice Research Institute, Los Baños, Philippines 6 Department of Agronomy, Kansas State University, Manhattan, KS, United States of America 7 Plant Hormone Biology group, Swammerdam Institute for Life Sciences, University of Amsterdam, Amsterdam, Netherlands ABSTRACT Background and Aim. Water is an increasingly scarce resource while some crops, such as paddy rice, require large amounts of water to maintain grain production. A better understanding of rice drought adaptation and tolerance mechanisms could help to reduce this problem. There is evidence of a possible role of root-associated fungi in drought adaptation. Here, we analyzed the endospheric fungal microbiota composition in rice and its relation to plant genotype and drought. Methods. Fifteen rice genotypes (Oryza sativa ssp. indica) were grown in the field, under well-watered conditions or exposed to a drought period during flowering. The effect of genotype and treatment on the root fungal microbiota composition was analyzed by 18S ribosomal DNA high throughput sequencing. Grain yield was determined after plant maturation. Results. There was a host genotype effect on the fungal community composition. Drought altered the composition of the root-associated fungal community and Submitted 12 November 2018 increased fungal biodiversity. -
Genera of Phytopathogenic Fungi: GOPHY 1
Accepted Manuscript Genera of phytopathogenic fungi: GOPHY 1 Y. Marin-Felix, J.Z. Groenewald, L. Cai, Q. Chen, S. Marincowitz, I. Barnes, K. Bensch, U. Braun, E. Camporesi, U. Damm, Z.W. de Beer, A. Dissanayake, J. Edwards, A. Giraldo, M. Hernández-Restrepo, K.D. Hyde, R.S. Jayawardena, L. Lombard, J. Luangsa-ard, A.R. McTaggart, A.Y. Rossman, M. Sandoval-Denis, M. Shen, R.G. Shivas, Y.P. Tan, E.J. van der Linde, M.J. Wingfield, A.R. Wood, J.Q. Zhang, Y. Zhang, P.W. Crous PII: S0166-0616(17)30020-9 DOI: 10.1016/j.simyco.2017.04.002 Reference: SIMYCO 47 To appear in: Studies in Mycology Please cite this article as: Marin-Felix Y, Groenewald JZ, Cai L, Chen Q, Marincowitz S, Barnes I, Bensch K, Braun U, Camporesi E, Damm U, de Beer ZW, Dissanayake A, Edwards J, Giraldo A, Hernández-Restrepo M, Hyde KD, Jayawardena RS, Lombard L, Luangsa-ard J, McTaggart AR, Rossman AY, Sandoval-Denis M, Shen M, Shivas RG, Tan YP, van der Linde EJ, Wingfield MJ, Wood AR, Zhang JQ, Zhang Y, Crous PW, Genera of phytopathogenic fungi: GOPHY 1, Studies in Mycology (2017), doi: 10.1016/j.simyco.2017.04.002. This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. -

Pdf Transporter Genes Are Contemporaneously Present in Mycorrhiza: an Ancient Symbiosis in Modern
Lectures 19 and 20: Mycorrhizas – Reading: Text, Chapter 17. ALSO great website from CSIRO in Austalia http://www.ffp.csiro.au/research/mycorrhiza/index.html http://mycorrhizas.info/index.html Rodriguez R and Redman R. 2008. More than 400 years of evolution and some plants still canʼt make it on their own. Journal of Experimental Botany 59: 1109-1114. Parniske M. 2008. Arbuscular mycorrhiza: the mother of plant root endosymbioses. Nature Reviews Microbiology 6: 763-773. Stinson, K.A. et al. 2006. Invasive plant suppresses the growth of native tree seedlings by disrupting belowground mutualisms. PLOS Biology Objectives: Understand the importance of mycorrhizas. Know how to recognize ectomycorrhizas, and the types of endomycorrhizas. Know how to prove that a mycorrhizal symbiosis has been formed (differentiating between what you expect with ecto- vs. endomycorrhizas). Know which groups of fungi (phyla, orders, families) form ectomycorrhizas, which form endomycorrhizas. Keywords: ectomycorrhiza, mantle, Hartig net, endomycorrhiza, vesicle, arbuscule, spore, Glomeromycota. Study questions: 1) What are the soil and root-associated structures found with VAM? With orchid mycorrhizas? Compare and contrast the structures of VAM, orchid mycorrhizas, and ECMs. Which fungal phyla form each of the three types of mycorrhizas that we have discussed? 2) Are VAM common in plant roots? Explain. 3) VAM appears to be a balanced mutualism – is this true? 4) You wish to prove that Russula mississaugii is a mycorrhizal fungus. How could you convince our class? Use your naked eye, a dissecting microscope, a compound microscope, and radio-isotope study of tree seedlings to prove your point! What are the controls? 5) What are the benefits to the plant and to the ecosystem of mycorrhizas? 6) Why do plant species that depend on mycorrhizas tend to lack root hairs? 7) Garlic mustard is very common around Mississauga and on this campus. -

A Virus in a Fungus in a Plant: Three-Way Symbiosis Required For
REPORTS to the Midwest Regional Center of Excellence for was supported by the NIH Institutional NRSA T32 SOM Text Biodefense and Emerging Infectious Disease Research GM07067 to the Washington University School of Figs. S1 to S4 (MRCE) and by NIH grant AI53298. The DDRCC is Medicine. Tables S1 and S2 supported by NIH grant DK52574. W.W.L. was supported References by the Clinical/Translational Fellowship Program of the Supporting Online Material MRCE, the W.M. Keck Foundation, and the NIH National www.sciencemag.org/cgi/content/full/315/5811/509/DC1 6 November 2006; accepted 14 December 2006 Research Service Award (NRSA) F32 AI069688-01. P.A.P. Materials and Methods 10.1126/science.1137195 S2). The 2.2-kb fragment (RNA 1) is involved in A Virus in a Fungus in a Plant: virus replication, as both of its ORFs are similar to viral replicases. The first, ORF1a, has 29% amino acid sequence identity with a putative Three-Way Symbiosis Required for RNA-dependent RNA polymerase (RdRp) from the rabbit hemorrhagic disease virus. The amino Thermal Tolerance acid sequence of the second, ORF1b, has 33% identity with the RdRp of a virus of the fungal 1 2,3 2,4 1 Luis M. Márquez, Regina S. Redman, Russell J. Rodriguez, Marilyn J. Roossinck * pathogen Discula destructiva.ThesetwoORFs overlap and could be expressed as a single A mutualistic association between a fungal endophyte and a tropical panic grass allows both protein by frameshifting, a common expression organisms to grow at high soil temperatures. We characterized a virus from this fungus that is strategy of viral replicases. -

Endophytic Fungi Associated with Pioneer Plants Growing on The
Endophytic Fungi Associated with Pioneer Plants Growing on the Athabasca Oil Sands By Xiaohui Bao Department of Biology University of Saskatchewan In partial fulfillment for the Degree of Master of Science Copyright Xiaohui Bao, April, 2009. All rights reserved. PERMISSION TO USE In presenting this thesis in partial fulfillment of the requirements for a postgraduate degree from the University of Saskatchewan, I agree that the Libraries of this University may make it freely available for inspection. I further agree that permission for copying this thesis in any manner, in whole or in part, for scholarly purposes may be granted by the professor or scientists who supervised my thesis work or, in their absence, by the Head of the Department of the Dean of the College in which my thesis work was done. It is understood that any copying or publication or use of this thesis or parts thereof for financial gain shall not be allowed without my written permission. It is also understood that due recognition shall be given to me and to the University of Saskatchewan in any scholarly use which may be made of any material in this thesis. Requests for permission to copy or to make other use of material in this thesis in whole or part should be addressed to: Head of the Department of Biology University of Saskatchewan Saskatoon, Saskatchewan (S7N 5E2) Canada i ABSTRACT Fungal endophytes live inside plants without causing apparent symptoms of infection. All plant species surveyed thus far, including liverworts, mosses, seedless vascular plants, conifers, and angiosperms, harbor one or more endophytic fungi. -

Utilization of Microbial Endophytes on Crop Plants and Trees As
• Overview of symbiosis -of microbial endophytes (bacterial and fungal) • Symbiosis is a good fit in the biological sciences and classroom • Symbiosis has many positive applications for agriculture and forestry Utilization of microbial endophytes on crop plants and • Has direct application to Forest Bioresources: trees as mechanism to increase biomass, enhance 1. use of plant-microbe symbiotic systems can be applied directly to increasing plant fitness and survival in stressed habitats bioenergy 2. improve the efficiency and lower the cost of biofuel production by promoting growth enhancement in plants resulting in enhanced biomass Regina Redman 3. growth on poor soils or in harsher environmental conditions so that we reserve the high quality land for food agriculture. University of Washington 4. Increasing water use efficiency Department of Forest Resources other examples: -improve plant health and stress tolerance (cold, salt, drought) Seattle, WA -increase biomass, decrease lignin, enhance biofuel (bioethanol) production -grow plants in unfavorable soils (oligotrophic, diazatrophic) Adaptive Symbiotic Technologies -decrease use of chemical fertilizers (soil and water contamination) Seattle, WA -Crop disease protection without using harmful chemicals (pesticides and fungicides) -Phytoremediation of soils (orgnaic pollutants, heavy metals) • Best way to demonstrate positive benefits via symbiosis is by focusing and presenting some of my research: Centered around plant-fungal microbial symbionts (potential application and ubiquitous nature of symbionts) Symbiosis: A close association between two different species (Anton de Bary 1879). Plants are Communities with Several Habitat Zones •An intimate association between two or more organisms Philosopher A fundamental aspect of biology (endophytes) All complex life on earth is symbiotic on one level or another (epiphytes) - important for health and survival of their host All plants in natural ecosystems are - eg. -

Climate Change and Micro-Organism Genetic Resources for Food and Agriculture: State of Knowledge, Risks and Opportunities
BACKGROUND STUDY PAPER NO. 57 May 2011 E COMMISSION ON GENETIC RESOURCES FOR FOOD AND AGRICULTURE CLIMATE CHANGE AND MICRO-ORGANISM GENETIC RESOURCES FOR FOOD AND AGRICULTURE: STATE OF KNOWLEDGE, RISKS AND OPPORTUNITIES by Fen Beed1, Anna Benedetti2, Gianluigi Cardinali3, Sukumar Chakraborty4, Thomas Dubois,5 Karen Garrett6 and Michael Halewood7 This document has been prepared at the request of the Secretariat of the FAO Commission on Genetic Resources for Food and Agriculture, as a contribution to the crosssectoral theme, Consideration of scoping study on climate change and genetic resources for food and agriculture, which the Commission will consider at its Thirteenth Regular Session. The content of this document is entirely the responsibility of the authors, and does not necessarily represent the views of the FAO or its Members. 1 IITA, United Republic of Tanzania 2 Consiglio per la Ricerca e la Sperimentazione in Agricoltura (CRA), Italy 3 Università degli Studi di Perugia, Italy 4 CSIRO, Australia 5 IITA, Uganda 6 Kansas State University, United States of America 7 Bioversity International, Italy. For resaons of economy, this document is produced in a limited number of copies. Delegates and observers are kindly requested to bring their copies to meetings and to refrain from asking for additional copies, unless strictly necessary. The documents for this meeting are available on Internet at: http://www.fao.org ii BACKGROUND STUDY PAPER NO. 57 TABLE OF CONTENTS Page Executive Summary ..................................................................................................................................... -

Virus Latency and the Impact on Plants
fmicb-10-02764 December 5, 2019 Time: 16:12 # 1 REVIEW published: 06 December 2019 doi: 10.3389/fmicb.2019.02764 Virus Latency and the Impact on Plants Hideki Takahashi1,2*, Toshiyuki Fukuhara3, Haruki Kitazawa4,5 and Richard Kormelink6 1 Laboratory of Plant Pathology, Graduate School of Agricultural Science, Tohoku University, Sendai, Japan, 2 Plant Immunology Unit, International Education and Research Center for Food Agricultural Immunology, Graduate School of Agricultural Science, Tohoku University, Sendai, Japan, 3 Department of Applied Biological Sciences and Institute of Global Innovation Research, Tokyo University of Agriculture and Technology, Tokyo, Japan, 4 Food and Feed Immunology Group, Laboratory of Animal Products Chemistry, Graduate School of Agricultural Science, Tohoku University, Sendai, Japan, 5 Livestock Immunology Unit, International Education and Research Center for Food Agricultural Immunology, Graduate School of Agricultural Science, Tohoku University, Sendai, Japan, 6 Laboratory of Virology, Wageningen University, Wageningen, Netherlands Plant viruses are thought to be essentially harmful to the lives of their cultivated crop hosts. In most cases studied, the interaction between viruses and cultivated crop plants negatively affects host morphology and physiology, thereby resulting in disease. Native wild/non-cultivated plants are often latently infected with viruses without any clear symptoms. Although seemingly non-harmful, these viruses pose a threat to cultivated crops because they can be transmitted by vectors -

Development of an Expression Vector to Overexpress Or Downregulate Genes in Curvularia Protuberata
Journal of Fungi Article Development of an Expression Vector to Overexpress or Downregulate Genes in Curvularia protuberata Chengke Liu, Blake Cleckler and Mustafa Morsy * ID The Department of Biological and Environmental Sciences, University of West Alabama, Livingston, AL 35470, USA; [email protected] (C.L.); [email protected] (B.C.) * Correspondence: [email protected]; Tel.: +1-1205-652-5541 Received: 12 April 2018; Accepted: 3 May 2018; Published: 5 May 2018 Abstract: Curvularia protuberata, an endophytic fungus in the Ascomycota, provides plants with thermotolerance only when it carries a mycovirus known as Curvularia thermotolerance virus (CThTV), and forms a three-way symbiotic relationship among these organisms. Under heat stress, several genes are expressed differently between virus-free C. protuberata (VF) and C. protuberata carrying CThTV (AN). We developed an expression vector, pM2Z-fun, carrying a zeocin resistance gene driven by the ToxA promoter, to study gene functions in C. protuberata to better understand this three-way symbiosis. Using this new 3.7-kb vector, five genes that are differentially expressed in C. protuberata—including genes involved in the trehalose, melanin, and catalase biosynthesis pathways—were successfully overexpressed or downregulated in VF or AN C. protuberata strains, respectively. The VF overexpression lines showed higher metabolite and enzyme activity than in the control VF strain. Furthermore, downregulation of expression of the same genes in the AN strain resulted in lower metabolite and enzyme activity than in the control AN strain. The newly generated expression vector, pM2Z-fun, has been successfully used to express target genes in C. protuberata and will be useful in further functional expression studies in other Ascomycota fungi.