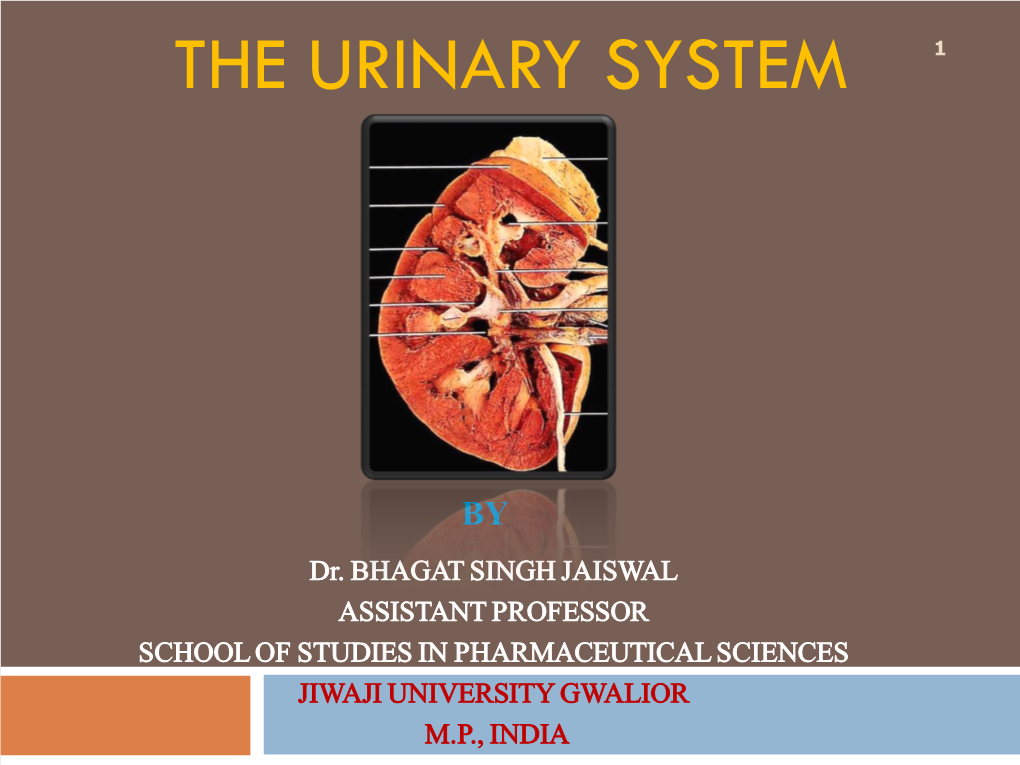
Urinary System 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Primary Excretory System Organs Kidneys Are Bean-Shaped Organs of a Reddish Brown Colour That Are Found in the Sides of the Vertebral Column
Organs in the Excretory System and Their Functions The excretory system is essential to one’s health. Its responsibility is to remove waste from the body. The excretory system is made up of numerous organs that work in unison to ensure that waste is effectively removed from your body. Below are the details of the organs of excretory system, along with the roles they play in detoxification. Primary Excretory System Organs Kidneys are bean-shaped organs of a reddish brown colour that are found in the sides of the vertebral column. Once the body has extracted what it needs from food and drink, it sends the wastes to the kidneys. The kidneys filter the wastes, including urea, salt and excess water, which are flushed out of the body as urine. s 2. Skin The skin performs its excretory function via the sweat glands. These glands produce sweat that contains salt, excess oils, water, and other unnecessary substances which are then excreted out of the body through small pores. Sweating also helps to cool the body during evaporation. 3. Lungs The lungs are very important excretory organs as they expel carbon dioxide from the body via exhalation. The lungs use cells known as alveoli to remove the carbon dioxide from our blood. Otherwise, the carbon dioxide would accumulate and have a detrimental effect to our body. Accessary Excretory System Organs 1. Liver Although considered a secondary, or accessary excretory system organ, the liver plays a vital part in keeping the body clean. Harmful poisons and chemicals that are either produced in the body or consumed are broken down and detoxified by the liver. -

Excretory Products and Their Elimination
290 BIOLOGY CHAPTER 19 EXCRETORY PRODUCTS AND THEIR ELIMINATION 19.1 Human Animals accumulate ammonia, urea, uric acid, carbon dioxide, water Excretory and ions like Na+, K+, Cl–, phosphate, sulphate, etc., either by metabolic System activities or by other means like excess ingestion. These substances have to be removed totally or partially. In this chapter, you will learn the 19.2 Urine Formation mechanisms of elimination of these substances with special emphasis on 19.3 Function of the common nitrogenous wastes. Ammonia, urea and uric acid are the major Tubules forms of nitrogenous wastes excreted by the animals. Ammonia is the most toxic form and requires large amount of water for its elimination, 19.4 Mechanism of whereas uric acid, being the least toxic, can be removed with a minimum Concentration of loss of water. the Filtrate The process of excreting ammonia is Ammonotelism. Many bony fishes, 19.5 Regulation of aquatic amphibians and aquatic insects are ammonotelic in nature. Kidney Function Ammonia, as it is readily soluble, is generally excreted by diffusion across 19.6 Micturition body surfaces or through gill surfaces (in fish) as ammonium ions. Kidneys do not play any significant role in its removal. Terrestrial adaptation 19.7 Role of other necessitated the production of lesser toxic nitrogenous wastes like urea Organs in and uric acid for conservation of water. Mammals, many terrestrial Excretion amphibians and marine fishes mainly excrete urea and are called ureotelic 19.8 Disorders of the animals. Ammonia produced by metabolism is converted into urea in the Excretory liver of these animals and released into the blood which is filtered and System excreted out by the kidneys. -

Essential Question: How Do Major Organ Systems Work Together in Living Organisms?
Essential Question: How do major organ systems work together in living organisms? Standards: S7L2d. Explain that tissues, organs, and organ systems serve the needs cells have for oxygen, food, and waste removal. S7L2e. Explain the purpose of the major organ systems in the human body (i.e., digestion, respiration, reproduction, circulation, excretion, movement, control and coordination, and for protection from disease). Watch the video clip below and identify which system of the body has a similar function. http://www.youtube.com/ watch?v=8erOa6W67IM [watch 1 min 30 seconds] Digestive System Role of the Digestive System Series of organs that convert food into essential nutrients, and moves unwanted waste out How does it do it? Chewing • Mechanical Digestion – Breaking down food into smaller pieces • Teeth are used to break food into smaller pieces Esophagus Pipe connecting the mouth to the stomach (involuntary muscles) Stomach Food is chemically broken down by acid to form paste called Chyme Chemical Digestion Food is converted (changed) into substances that can be absorbed by the body Small Intestine Where the nutrients (glucose, protein, etc.) are absorbed into the bloodstream Large Intestine • Pulls out water from left overs • Last portion called rectum • Anus is the opening at the end Finish the Story Because Mrs. Fizzle’s class doesn’t want to exit Arnold “the back way”, they decide to go back the way they came. Write a brief explanation of the route they will take and what they will see and experience as they go back the way they -

Excretory System
Excretory System Excretory System • Functions • Removes wastes from blood • Removes harmful substances from blood • Regulates body fluids • Maintains homeostasis • Main Parts • Kidneys • Urinary bladder • Large intestine • Lungs • Skin Urinary System: • Not all the waste products that leave the body are solid. • Most liquid wastes formed by the body are excreted by the urinary system. Bladder • Muscular sac in the pelvis • Urine is made in the kidneys and travels down two tubes called ureters to the bladder • Urine exits the bladder into the urethra, which carries out of the body Large Intestine: • The undigested material not absorbed by the large intestine forms a semi- solid waste product known as feces. These solid wastes are removed by the body through the rectum. Kidneys: • The main organs of the urinary system • Bean-shaped organs in your abdomen that filter blood and remove waste. • The wastewater, or urine, that has been filtered out of the blood moves into the ureters, tubes that connect the kidneys to the bladder. • The bladder is a muscular sac that holds urine until it exits the body through the urethra. The Lungs: • The lungs are another part of the excretory system. • Lungs are part of the respiratory system, also. • Wastes removed by the lungs include carbon dioxide and water vapor produced by cellular respiration. The Skin • The skin also functions in excretion. • Sweat glands in the skin produce perspiration. • When a person perspires, the skin excretes water and salts. Working Together Works with the circulatory system in transporting blood through kidneys. Urea, uric acid, and water are removed from the blood and most of the water is put back in the system. -

Ch. 38 Excretory System Vena Cava Aorta
Digestive System Mouth • Digestion begins in the ________Mouth . ________Chewing begins the process of digestion • __________________Mechanical digestion - is the physical breakdown of large pieces of food into smaller pieces. • __________________Chemical digestion - large food molecules are broken down into smaller food molecules with the help of different enzymes. Mouth • _______________salivary glands secrete saliva, which contains the enzyme _________amylase to break the bonds in _________starches (which is what type of macromolecule: ______________)Carbohydrate and releases sugar. It also contains the enzyme __________lysozyme that fights infection by digesting the cell walls of ________bacteria . The saliva also helps ___________moisten the food and make it easier to chew. The release of saliva is under the control of the ________________nervous system Esophagus • Your ________tongue and your throat_______ muscles help you swallow your food, which (after swallowing) is now called a _______bolus . As you swallow, the epiglottis________ closes over the _______trachea and the bolus enters the __________.esophagus Gravity______ is not responsible for food going down into the stomach. Esophagus • A series of contractions of _______smooth muscle squeeze the food through the ___________esophagus . This is called peristalsis_________ . A thick ring of muscle called the cardiac_____________sphincter closes the esophagus and prevents the contents of the ________stomach from moving back into the esophagus (also known as acid reflux____). ***Remember: No Digestion_ occurs in the esophagus. Stomach • Food from the esophagus empties into a large muscular sac called the ___________stomach . Alternating contractions of the stomach’s ____3 smooth muscle layers churn_____ and mix the food____. Stomach- Chemical digestion: • The stomach contains microscopic _______________Gastric glands that produce and release various substances. Some of these include: • ________Mucus - a fluid that __________lubricates and _________protects the stomach wall. -

Excretory System
Excretory system Components The excretory system, or urinary system, is made up of the two kidneys, ureters, bladder and urethra, together with the branches of the two renal arteries and veins. Functions The kidneys are responsible for osmoregulation and the elimination of toxic wastes, including nitrogenous excretion. Osmoregulation is important as extracellular fluid must not induce osmosis either by causing cells to lose water and shrink or to gain water and swell up. Nitrogenous excretion is necessary as amino acids cannot be stored by the body. Proteins obtained in food invariably contain an imbalance of certain amino acids – they are not in the correct Figure 1 The excretory system. proportions for use in protein synthesis in the body. Those that cannot be assimilated are deaminated by the liver, forming fatty acids and ammonia. Most of the highly toxic ammonia is rapidly converted to urea to be removed from the body by the kidneys in urine. The kidneys not only excrete metabolic wastes including ammonia, urea, uric acid and creatinine, but have the main responsibility for maintaining the stability of extracellular fluid volume, inorganic ion composition and osmolarity (solute concentration). They contribute to maintenance of pH and also secrete certain hormones. Key mechanisms The functional unit in a kidney is the nephron (kidney tubule). Blood is filtered: Each nephron is made up of a filtering unit - Bowman’s capsule, and a tubule. Each capsule contains a tight knot of capillaries, called the glomerulus. Blood flows into the glomeruli under pressure forcing a filtrate free of cells and protein through the capillary walls. -

Human Systems
CONSEJERÍA DE EDUCACIÓN Dirección General de Participación e Innovación Educativa Identificación del material AICLE TÍTULO Human systems NIVEL LINGÜÍSTICO A1.2 SEGÚN MCER IDIOMA Inglés ÁREA / MATERIA Conocimiento del Medio Natural, Social y Cultural Aspectos básicos sobre los diferentes aparatos del ser humano, los órganos NÚCLEO TEMÁTICO que los componen y cómo funcionan. Secuencia didáctica que describe los diferentes aparatos que conforman el ser humano, destacando el aparato digestivo, respiratorio, circulatorio, reproductor GUIÓN TEMÁTICO y digestivo, así como sus órganos y las funciones y procesos que desarrollan en el ser humano. FORMATO PDF CORRESPONDENCIA 4º de Educación Primaria CURRICULAR AUTORÍA Miguel Ángel Cabo Sánchez. TEMPORALIZACIÓN 7-8 sesiones APROXIMADA - Aprender a aprender: los alumnos/as trabajan de forma autónoma en múlti- ples de las actividades a lo largo de la unidad. - Competencia lingüística: los alumnos/as interactúan de forma oral y escrita en diversidad de actividades. Se integran todas las destrezas en las diferentes actividades. También se presenta el proyecto de forma oral. - Competencia en el conocimiento e interacción con el mundo físico: los alum- nos/as conocen y descubren su cuerpo y funcionamiento de este. COMPETENCIAS - Competencia digital y tratamiento de la información: los alumnos/as hacen BÁSICAS uso de las TIC para ampliar información en torno al ser humano y sus carac- terísticas. - Competencia cultural y artística: los alumnos/as realizan un proyecto sobre un aparato humano usando diferentes materiales de reciclado u otros. Fo- mento de la creatividad. - Autonomía e iniciativa personal: los alumnos/as investigan y eligen el aparato que desean para llevar a cabo su proyecto. -
Human Anatomy and Body Systems Levels of Organization
Human Anatomy and Body Systems Levels of Organization Remember, the human body is organized in several levels, from the simplest to the most complex. Cells – the basic unit of life Tissues – clusters of cells performing a similar function Organs – made of tissues that perform one specific function Organ Systems – groups of organs that perform a specific purpose in the human body ***The purpose of the 11 organ systems is for the human body to maintain homeostasis. 4- Cell types muscle tissue most abundant tissue controls internal movement digestion, blood through veins external movement of body epithelial tissue covering for body & organs linings of organs & vessels connective tissue holds organs in place ligaments, tendons, some keep organs in place nervous tissue receives messages from body’s internal and external messages analyze data & direct response The 11 Human Body Systems The 11 human body systems are as follows: -- nervous system -- integumentary system -- respiratory system -- digestive system -- excretory system -- skeletal system -- muscular system -- circulatory system -- endocrine system -- reproductive system -- lymphatic (immune) system The Circulatory System Purpose: to deliver oxygenated blood to the various cells and organ systems in your body so they can undergo cellular respiration Cell type - Muscle Major Organs and Their Functions Heart – the major muscle of the circulatory system -- pumps deoxygenated blood into the lungs, where it gets oxygenated, returned to the heart, and then pumped out through the aorta to -
The Human Body—Respiratory and Excretory Systems April 20 – April 24 Time Allotment: 30 Minutes Per Day
Life Science 7: The Human Body—Respiratory and Excretory Systems April 20 – April 24 Time Allotment: 30 minutes per day Student Name: ________________________________ Teacher Name: ________________________________ Life Science 7: Respiratory and Excretory Systems April 20 – April 24 Packet Overview Date Objective(s) Page Number Monday, April 20 1. Explain the functions of the respiratory system. 2 2. Assess the importance of gas exchange and surface area in the respiratory system. Tuesday, April 21 1. Explain how humans breathe and what other 4 organ systems are directly involved with the respiratory system. 2. Assess how speech is formed and compare speech in humans to communication in elephants. Wednesday, April 22 1. Analyze the respiratory system function through 6 hands on lab. Thursday, April 23 1. Explain the function of the excretory system. 8 2. Analyze what chemical analysis of urine can tell us about human health. Friday, April 24 School Holiday N/A Additional Notes: Welcome to your fifth week of Life Science distance learning. Your lab on Wednesday will include a write up of your observations and conclusions, which will count for a minor assessment grade. I encourage you all to attend Zoom sessions, even if you don’t think you have questions about the material…we’ve had great discussions to augment the material in the packets! Be well, my fine Great-Hearted scholars! Zoom Office Hours: 2nd Period: Monday & Wednesday, 11:00 am to 11:50 am 3rd Period: Monday & Wednesday, 1:00 pm to 1:50 pm 4th Period: Tuesday & Thursday, 10:00 am to 10:50 am 5th Period: Tuesday & Thursday, 11:00 am to 11:50 am 6th Period: Tuesday & Thursday, 1:00 pm to 1:50 pm Academic Honesty I certify that I completed this assignment I certify that my student completed this independently in accordance with the GHNO assignment independently in accordance with Academy Honor Code. -
NOTES: Urinary (Excretory) System (CH 15) Part 1 – Anatomy of the Urinary System Urinary (Excretory) System…
NOTES: Urinary (Excretory) System (CH 15) Part 1 – Anatomy of the Urinary System Urinary (Excretory) System… *The urinary system consists of the kidneys, ureters, urinary bladder, and urethra.. Functions of the Urinary System: 1) remove salts and nitrogenous wastes from the blood 2) maintain normal water and electrolyte concentrations within body fluids 3) regulates pH and volume of body fluids 4) helps control red blood cell production and blood pressure ORGANS OF THE URINARY SYSTEM 1) KIDNEYS: remove substances from the blood; form urine 2) URETERS: transport urine from the kidneys 3) URINARY BLADDER : stores urine 4) URETHRA : conveys urine to the outside of the body ● KIDNEYS located high on the posterior abdominal wall each kidney is divided into the: *CORTEX : outer region *MEDULLA : inner region *PELVIS : funnel-shaped region where superior end of ureters expands KIDNEY FUNCTIONS: 1) remove metabolic wastes from the blood & combine them with water formation of urine 2) secrete hormone erythropoietin control of red blood cell formation 3) involved in activation of vitamin D 4) help to maintain blood pressure KIDNEY BLOOD SUPPLY: • RENAL ARTERIES : arise from abdominal aorta ; supply blood to kidney branches into smaller arteries & eventually into the AFFERENT ARTERIOLES • blood returns to the inferior vena cava through the RENAL VEINS ● URETERS each ureter is about 25 cm long begin at the renal pelvis; extend downward and join the URINARY BLADDER from underneath ● URETERS 3 layers: 1) inner layer (mucous coat): continuous -

Respiratory & Excretory Systems Respiratory System Path of Air
34.2 and 34.3 Respiratory and Excretory Systems Respiratory System Respiratory · sustains cellular respiration (making ATP) by supplying O2 to body cells & Excretory Systems removing CO2 waste from cells Sections 34.2 & 34.3 · 2 processes breathing = moving air into and out of lungs respiration = exchange of gases in the body external = gas exchange between air and blood internal = gas exchange between blood and body cells Path of Air · enters mouth and nose Breathing hairs filter out dust and lg. particles · rate controlled by brain cilia sweep foreign particles responds to levels of CO2 toward throat in bloodstream mucous membranes warm and · inhalation moisten diaphragm contracts, · filtered air enters the pharynx (throat) ribcage expands, and · passes through epiglottis into the air fills lungs larynx (voice box) · exhalation · trachea (windpipe) bronchi lungs diaphragm relaxes, · inside each lung bronchi branch into ribcage contracts, and air flows out of lungs bronchioles · bronchioles lead to alveoli (little air sacs) where external respiration occurs O2 into capillaries CO2 back into lungs for exhale Excretory System Kidneys · aka urinary system · bean-shaped · functions · filter out wastes, water, and remove water (nitrogen-based) and excess water salts from the blood from body · renal cortex - outer layer maintain pH of blood · renal medulla - inner layer · structures · composed of nephrons kidneys, ureters, urinary bladder, urethra 34.2 and 34.3 Respiratory and Excretory Systems Nephrons · filtering unit of the kidney about 1 million in each kidney · blood is filtered in the glomerulus · anything the body needs or can reuse is reabsorbed as it travels through the nephron ex. -

The Excretory System
www.ck12.org Concept 1. The Excretory System CONCEPT 1 The Excretory System Lesson Objectives • Identify the functions of the excretory system. • List the organs of the excretory system. • Describe the parts of urinary system. • Outline how the kidneys filter blood. • Identify three disorders of the urinary system. Check Your Understanding • What are some "wastes" that must be removed from your body? • Do your circulatory and respiratory systems remove "waste?" Vocabulary • excretion • excretory system • kidney • kidney dialysis • kidney failure • nephron • urinary bladder • urinary system • urinary tract infection (UTI) • urination • urine The Excretory System One of the most important ways your body maintains homeostasis is by keeping the right amount of water and salts inside your body. If you have too much water in your body, your cells can swell and burst. If you have too little water in your body, your cells can shrivel up like an old apple. Either extreme can cause illness and death of cells, tissues, and organs. The organs of your excretory system help to keep the correct balance of water and salts within your body. Your body also needs to remove the wastes that build up from cell activity and from digestion. These wastes include carbon dioxide, urea, and certain plant materials. If these wastes are not removed, your cells can stop working and you can get very sick. The excretory system can also help to release wastes from the body. Excretion is the process of removing wastes from the body. The organs of the excretory system are also parts of other organ systems. For example, your lungs are part of the respiratory system.