Property & Asset Management Strategy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Orchard Main Street, Newstead, Melrose. TD6 9DE 060818 FINAL.Pub
‘The Orchard’ Main Street, Newstead, Melrose. TD6 9DE Development Opportunity The Orchard, Main Street, Newstead, Melrose. TD6 9DE A site extending to approximately 0.330 Ha (0.82 acre) providing a well positioned The southern terminus of the new established Borders Railway linking the Central Borders to residential development opportunity. The site is zoned within the Scottish Borders Edinburgh Waverley is Tweedbank Station approximately 2.5miles west. Supplementary Guidance on Housing 2017 with an indicative capacity of 6 houses. The Residential Development Opportunity A site extending to approximately 0.330ha (0.82 acres) or thereby with frontage to Main • Attractive position to the east of the sought after village of Newstead. Street, accessed off Back Road which runs around the east and north boundaries. This is • Zoned for housing with an indicative capacity of 6 houses. effectively an infill development site bounded by housing to the north, south and west. • Mature landscape setting • Development Strategy Report available for the site to Interested Parties The site is zoned for housing within the Scottish Borders Housing Local Development Plan • Convenient readily accessible edge of Village location within the Central Borders 2016 as modified by Supplementary Guidance on Housing 2017 with an indicative capacity of 6 houses. The site is within the settlements Conservation Area. Offers over £175,000 are invited Ref. GD4833 Development Strategy Report Page\Park have produced a Development Strategy Report for the site. General Information The Orchard is a site of 0.330 ha (0.82 acre) accessed off Back Row to the east of Newstead. This reports includes an indicative layout plan which reflects the character of the Newstead is a relatively small village with a population of approximately 260. -
Emergency Department Activity
NHS Scotland - Emergency Department Activity Attendances and Performance against the 4-hour Waiting Time Standard This is an ISD Scotland National Statistics release. The Scottish Government waiting time standard for emergency departments is that 98 % of all attendances should be seen within 4 hours. The figures presented in these tables detail the performance of each individual site and NHS board against the standard. Time Period: Apr-10 to Mar-11 Source: A&E data mart, ISD Scotland Date: 07 May 2012 List of Tables Table 1: Attendances and performance against 4-hour standard, Apr-10 to Mar-11 Total attendances, number of attendances breaching standard and attendances meeting standard (number and percentage). Figures are given at site and NHS Board level. Table 2: Attendances, Apr-10 to Mar-11 Summary table of attendances only. Figures are given at site and NHS Board level. Table 3: Performance against 4-hour standard, Apr-10 to Mar-11 Summary table of percentage of attendances meeting standard. Figures are given at site and NHS Board level. Notes: 1) The waiting time is defined as the time of arrival until the time of discharge, admission or transfer. 2) New presentations only; excludes planned return and recall attendances. 3) There are two types of site that provide emergency care; • ED - Emergency Departments; sites that provide a 24 hour emergency medicine consultant led service • MIU/Other - sites including minor injuries units (MIU), small hospitals and health centres in rural areas that carry out emergency department related activity and are GP or Nurse led. They may or may not be open 24 hours. -

The Galashiels and Selkirk Almanac and Directory for 1898
UMBRELLAS Re-Covered in One Hour from 1/9 Upwards. All Kinds of Repairs Promptly Executed at J. R. FULTON'S Umbrella Ware- house, 51 HIGH STREET, Galashiels. *%\ TWENTIETH YEAR OF ISSUE. j?St masr Ok Galasbiels and Selkirk %•* Almanac and Directorp IFOIR, X898 Contains a Variety of Useful information, County Lists for Roxburgh and Selkirk, Local Institutions, and a Complete Trade Directory. Price, - - One Penny. PUBLISHED BY JOH3ST ZMZCQ-CTiEiE] INT, Proprietor of the "Scottish Border Record," LETTERPRESS and LITHOGRAPHIC PRINTER, 25 Channel Street, Galashiels. ADVERTISEMENT. NEW MODEL OF THE People's Cottage Piano —^~~t» fj i «y <kj»~ — PATERSON & SONS would draw Special Attention to this New Model, which is undoubtedly the Cheapest and Best Cottage Piano ever offered, and not only A CHEAP PIANO, but a Thoroughly Reliable Instrument, with P. & Sons' Guakantee. On the Hire System at 21s per Month till paid up. Descriptive Price-Lists on Application, or sent Free by Post. A Large Selection of Slightly-used Instruments returned from Hire will be Sold at Great Reductions. Sole Agents for the Steinway and Bechstein Pianofortes, the two Greatest Makers of the present century. Catalogues on Application. PATEESON <Sc SONS, Musicsellers to the Queen, 27 George Street, EDINBURGH. PATERSON & SONS' Tuners visit the Principal Districts of Scotland Quarterly, and can give every information as to the Purchase or Exchanne of Pianofortes. Orders left with John McQueen, "Border Record" Office, Galashiels, shall receive prompt attention. A life V'C WELLINGTON KNIFE POLISH. 1 *™ KKL f W % Prepared for Oakey's Knife-Boards and all Patent Knife- UfgWa^^""Kmm ^"it— I U Clea-iing Machines. -

Accident and Emergency: Performance Update
Accident and Emergency Performance update Prepared by Audit Scotland May 2014 Auditor General for Scotland The Auditor General’s role is to: • appoint auditors to Scotland’s central government and NHS bodies • examine how public bodies spend public money • help them to manage their finances to the highest standards • check whether they achieve value for money. The Auditor General is independent and reports to the Scottish Parliament on the performance of: • directorates of the Scottish Government • government agencies, eg the Scottish Prison Service, Historic Scotland • NHS bodies • further education colleges • Scottish Water • NDPBs and others, eg Scottish Police Authority, Scottish Fire and Rescue Service. You can find out more about the work of the Auditor General on our website: www.audit-scotland.gov.uk/about/ags Audit Scotland is a statutory body set up in April 2000 under the Public Finance and Accountability (Scotland) Act 2000. We help the Auditor General for Scotland and the Accounts Commission check that organisations spending public money use it properly, efficiently and effectively. Accident and Emergency | 3 Contents Summary 4 Key messages 7 Part 1. A&E waiting times 9 Part 2. Reasons for delays in A&E 20 Part 3. Action by the Scottish Government 37 Endnotes 41 Appendix 1. NHS Scotland A&E departments and minor injury units 43 Appendix 2. National context for A&E and unscheduled care, 2004 to 2014 45 Exhibit data When viewing this report online, you can access background data by clicking on the graph icon. The data file will -

95 Galashiels Road, Stow
95 Galashiels Road, Stow 95 Galashiels Road is a well-presented two/three-bedroom ground floor flat situated in the popular Borders village of Stow. Within walking distance of the Borders Railway station, which runs to Edinburgh, there are amenities in the village which include a village shop with post office, a coffee shop, a primary school, a health centre and open countryside on the doorstep. Forming part of a larger detached house, there is lapsed planning permission for the erection of a dwellinghouse on the garden ground adjacent to the property. Currently used as private parking off-street parking for two to three cars, it offers excellent potential for something like a garage with studio or hobby space over – subject to the necessary permissions. Internally, the accommodation comprises two double bedrooms, a bathroom, a sitting room, a dining kitchen, a study/bedroom three and a utility room. Externally, the property has garden ground to the front, with lawn and borders, which is ideal for sitting out, plus a large area of terraced garden ground to the side, which provides the private parking for two to three cars whilst offering an excellent space for the erection of a garage or such. Edinburgh and most Border towns are also readily available from this highly accessible location with the A7 running through Stow providing links to Edinburgh in the North and Carlisle in the South. Galashiels 7.5 miles. Edinburgh 26 miles. Melrose 12 miles. Lauder 5.5 miles (All mileage is approximate) Location: 95 Galashiels Road is situated in popular Borders village of Stow, which benefits from a railway station on the Tweedbank to Edinburgh Borders Railway, which is soon to have a bar and bistro at the station. -

Mental Health Bed Census
Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Data Collection Documentation Document Type: Guidance Notes Collections: 1. Mental Health and Learning Disability Bed Census: One Day Audit 2. Mental Health and Learning Disability Patients: Out of Scotland and Out of NHS Placements SG deadline: 30th November 2014 Coverage: Census date: Midnight, 29th Oct 2014 Page 1 – 10 Nov 2014 Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Document Details Issue History Version Status Authors Issue Date Issued To Comments / changes 1.0 Draft Moira Connolly, NHS Boards Beth Hamilton, Claire Gordon, Ellen Lynch 1.14 Draft Beth Hamilton, Ellen Lynch, John Mitchell, Moira Connolly, Claire Gordon, 2.0 Final Beth Hamilton, 19th Sept 2014 NHS Boards, Ellen Lynch, Scottish John Mitchell, Government Moira Connolly, website Claire Gordon, 2.1 Final Ellen Lynch 9th Oct 2014 NHS Boards, Further clarification included for the following data items:: Scottish Government Patient names (applicable for both censuses) website ProcXed.Net will convert to BLOCK CAPITALS, NHS Boards do not have to do this in advance. Other diagnosis (applicable for both censuses) If free text is being used then separate each health condition with a comma. Mental Health and Learning Disability Bed Census o Data item: Mental Health/Learning Disability diagnosis on admission Can use full description option or ICD10 code only option. o Data item: Last known Mental Health/Learning Disability diagnosis Can use full description option or ICD10 code only option. -

Borders College Melrose Road – Galashiels June 2009
Scottish Borders Local Plan Supplementary Planning Guidance on Draft Planning Brief – Borders College Melrose Road – Galashiels June 2009 Contents Page No: 1. Introduction 2 2. Site Context 2 3. History of Site 4 4. Policy Context 6 4.1 National 4.2 Structure Plan 4.3 Local Plan 4.4 Supplementary Planning Guidance 5. Development Vision 7 6. Development Guidance 10 6.1 Energy Efficiency 6.2 Parking and the External Environment 6.3 Ecology and Habitat 6.4 Waste management 7. Constraints 10 7.1 Listed Building 7.2 Access (vehicular & pedestrian) 7.3 Water, Drainage and Sustainable Urban Drainage Systems 8. Development Contributions 12 8.1 Education 8.2 Waverley Line 8.3 Play Areas 9. Housing Density 13 Alternative Format/Language Paragraph 14 Appendix One – Historic Scotland Listed Building Report 15 Appendix Two – Contacts within Scottish Borders Council 18 List of Images Image 1: Entrance to Borders College 2 Image 2: Example of surrounding houses 2 Image 3: Southern aspect of Thorniedean House 10 Image 4: Listed gates of Thorniedean House 10 Image 5: Access to Sports Centre 11 Image 6: Entrance to Langhaugh Lane 11 List of Figures Figure 1: Local context 3 Figure 2: Existing buildings 5 Figure 3: Redevelopment plans 9 1 1. Introduction 1.1 This planning brief sets out the main opportunities and constraints relating to the redevelopment site at Borders College, Melrose Road, Galashiels. It provides a framework for the future development of the site within the period of the recently adopted Local Plan, over the next five years. 1.2 The brief identifies where detailed attention to specific issues is required and where development contributions will be sought. -
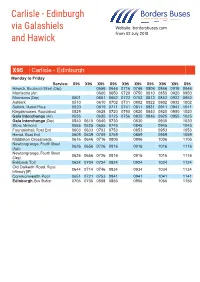
Carlisle - Edinburgh Via Galashiels Website: Bordersbuses.Com and Hawick from 02 July 2018
Carlisle - Edinburgh via Galashiels Website: bordersbuses.com and Hawick From 02 July 2018 X95 Carlisle - Edinburgh Monday to Friday Service: X95 X95 X95 X95 X95 X95 X95 X95 X95 X95 Hawick, Buccleuch Street (Dep) 0556 0646 0716 0746 0806 0846 0916 0946 Morrisons (Arr) 0600 0650 0720 0750 0810 0850 0920 0950 Morrisons (Dep) 0501 0601 0652 0722 0752 0812 0852 0922 0952 Ashkirk 0510 0610 0702 0731 0802 0822 0902 0932 1002 Selkirk, Market Place 0520 0619 0711 0741 0811 0831 0911 0941 1011 Kingsknowes, Roundabout 0529 0628 0720 0750 0820 0840 0920 0950 1020 Gala Interchange (Arr) 0535 0635 0725 0756 0825 0846 0925 0955 1025 Gala Interchange (Dep) 0540 0610 0640 0730 0830 0930 1030 Stow, Memorial 0555 0625 0655 0745 0845 0945 1045 Fountainhall, Road End 0603 0633 0703 0753 0853 0953 1053 Heriot, Road End 0609 0639 0709 0759 0859 0959 1059 Middleton Crossroads 0616 0646 0716 0806 0906 1006 1106 Newtongrange, Fourth Street 0626 0656 0726 0816 0916 1016 1116 (App) Newtongrange, Fourth Street 0626 0656 0726 0816 0916 1016 1116 (Dep) Eskbank Toll 0634 0704 0734 0824 0924 1024 1124 Old Dalkeith Road, Royal 0644 0714 0746 0834 0934 1034 1134 Infirmary [IF] Commonwealth Pool 0651 0721 0753 0841 0941 1041 1141 Edinburgh, Bus Station 0706 0736 0808 0856 0956 1056 1156 X95 Carlisle - Edinburgh Monday to Friday Service:Service: X95X95 X95X95 X95X95 X95X95 X95X95 X95X95 X95X95 X95X95 X95X95 X95X95 HawickCarlisle, Buccleuch, English St, Street The Courts(Dep) [A] 0855 05560955 0646 07161055 0746 08061155 0846 09161255 0946 MorrisonsKingstown (Arr) Road , -

Galashiels/Coldstream-Newcastle/Metrocentre
Effective From: 04 September 2006 Service GALASHIELS/COLDSTREAM-NEWCASTLE/METROCENTRE 710 Via Galashiels,Darnick,Melrose,Newton St.Boswells,St.Boswells,Kelso,Coldstream,Cornhill,Branxton,Crookham,Milfield,Wooler,Powburn,Glanton,Whittingham,Bridge of Aln,Longframlington,Longhorsley,Morpeth,North Road,Gosforth High Street,North Road,Claremont Road,Queen Victoria Road,St.Thomas' Street.(Certain journeys continue to Metrocentre Coach Park) Wednesday And Satuday Only 710 710 710 W S W * z Coldstream .................................... 0915 0915 ... Wooler........................................... 0945 0945 1625 Powburn......................................... 0955 0955 1635 Glanton.......................................... 1000 1000 ... Whittingham .................................. 1005 1005 ... Longframlington............................. 1020 1020 1655 Longhorsley.................................... 1030 1030 1705 Morpeth ......................................... 1040 1040 ... Northumberland County Hall ......... 1045 1045 ... Gosforth High Street....................... ... 1100 ... Newcastle St.Thomas Street (M)...... 1105 1105 1728 Metrocentre Coach Park ................. ... 1125 ... Operated by: Glen Valley Tours Explanation of codes: : Commences from Galashiels at 0810,via Kelso at 0855. z: Commences from Kelso at 0855 *: Operated by Munros of Jedburgh Certain journeys are secured on your behalf by Northumberland County Council. Effective From: 04 September 2006 Service METROCENTRE/NEWCASTLE-KELSO/GALASHIELS 710 ( Certain journeys -

Residential Building Plots Wellrig St Boswells Melrose TD6 9ET
Residential Building Plots Wellrig St Boswells Melrose TD6 9ET rightmove.co.uk The UK’s number one property website Ref: 107 rural | forestry | environmental | commercial | residential | architectural & project management | valuation | investment | management | dispute resolution | renewable energy Residential Building Plots Wellrig, St Boswells, Melrose, TD6 9ET General Information The approved plans for each plot are available on the planning portal and Directions Wellrig Farm is situated approximately 1.7 miles south of St Boswells, in a are designed to provide spacious accommodation and take advantage of the Travelling south from St Boswells on the A68 trunk road, turn right after quiet rural location with outstanding views of the Eildon Hills. outstanding outlook. approximately 1.25 miles at the sign for Longnewton. The plots are easily accessible from the A68 trunk road and are within 11 Plot Planning Ref Description Wellrig Farm is situated on the right hand side after approximately ½ a mile. miles of the Borders towns of Melrose, Galashiels, Jedburgh, Kelso, Selkirk Plot 1 09/01265/AMC Two storey, 4 bed. and Earlston which offer a wide range of amenities, including 24 hour Plot 5 09/01268/AMC Two storey, 4 bed. Viewing supermarket, cafes, swimming pools, a range of sports clubs and secondary Strictly by prior appointment with the sole selling agents Edwin Thompson schools. Services LLP, Chartered Surveyors. The pipework for the water supply is installed to the edge of each plot with The new Borders railway, scheduled to open in September 2015, can be the purchaser responsible for the final connection to the Scottish Water main Price accessed from Galashiels from where it will take 50mins to get to Edinburgh in the public road verge. -

Update on the Public Play Facilities Strategy
UPDATE ON THE PUBLIC PLAY FACILITIES STRATEGY Report by Service Director Assets & Infrastructure SCOTTISH BORDERS COUNCIL 27 August 2020 1 PURPOSE AND SUMMARY 1.1 Following the meeting Scottish Borders Council on 19 December 2019, this report sets out the process and outcomes of engagement with Ward Members on proposals for the decommissioning of some play equipment in some play parks within the Scottish Borders, as agreed. 1.2 The strategic review of Play facilities is integral to the planned future investment in Outdoor Community Spaces including Public Play parks, agreed as part of the 2018/19 Capital Investment Plan and updated within the Capital Investment Plan 2019-20 and 2020/21. The current 2020/21 capital budget includes funding of £4.809m into Outdoor Community Spaces over a 10-year period. This investment aims to unlock community aspirations in this area creating high quality destination play parks, as well as facilities for skating and small wheels, youth shelters and opportunities for people of all ages to take part in physical activity. Investment in these destination play parks has already completed in Galashiels (2018), Harestanes (2019), Selkirk(2016), Hawick (2017), Coldstream (2019) and Kelso (2019) with Peebles currently being procured and expected to be delivered in 2020. 1.3 The new investment creates a financial revenue burden and, in order to ensure a cost neutral impact of the investment to the Council, a programme of decommissioning of aged and underutilised play equipment is required. 1.4 Council agreed in May 2018 to review the distribution of play equipment provision across play parks in the Borders, to firstly inform decision making around future investment in communities and secondly guide the rationalisation of play facilities which are deemed no longer fit for purpose, ensuring a cost neutral impact on established budgets. -

Major Emergency Procedures
Borders MAJOR EMERGENCY PROCEDURES MAJOR INCIDENT DECLARED ACTIVATE PLAN ALERT STAFF ESTABLISH EMERGENCY RESPONSE TEAMS DEPLOY RESOURCES NHS BORDERS MAJOR EMERGENCY PROCEDURES MAJOR EMERGENCY PROCEDURES PLAN IN THE EVENT OF A MAJOR EMERGENCY TURN IMMEDIATELY TO THE ACTION CARD RELEVANT TO YOUR AREA Unique Identifier Master document held by Issue Date 1 Lorna Paterson 31 May 2011 Resilience Manager Review Date May 2012 CURRENT VERSION IS HELD ON THE NHS BORDERS INTRANET PAGE http://intranet/new_intranet/microsites/index.asp?siteid=32&uid=5 PLEASE CHECK THAT THIS PRINTED COPY IS THE LATEST VERSION NHS Borders Major Emergency Procedures Issue date 31 May 2011 Review date May 2012 NHS BORDERS MAJOR EMERGENCY PROCEDURES IMMEDIATE ACTIONS If you have received notification that a Major Incident has been declared and you have not read the plan DO NOT READ IT NOW Find your relevant action card in • Section 2a – Chief Executive or Executive on call, Consultant in Public Health Medicine on call • Section 5 – BGH Response • Section 7 – Primary and Community Services, Mental Health and Learning Disabilities AND FOLLOW THE INSTRUCTIONS NHS Borders Major Emergency Procedures Issue date 31 May 2011 Review date May 2012 NHS BORDERS MAJOR EMERGENCY PROCEDURES MAJOR EMERGENCY LOG Everyone involved in the Major response must keep a record of their actions and make copies available for debrief purposes. The Major Emergency Log must record dates and times of all information given and received, decisions, actions and all other communications relating to the incident. All written documents, letters, emails and fax messages should be dated and time of receipt recorded, with cross reference to the log where appropriate.