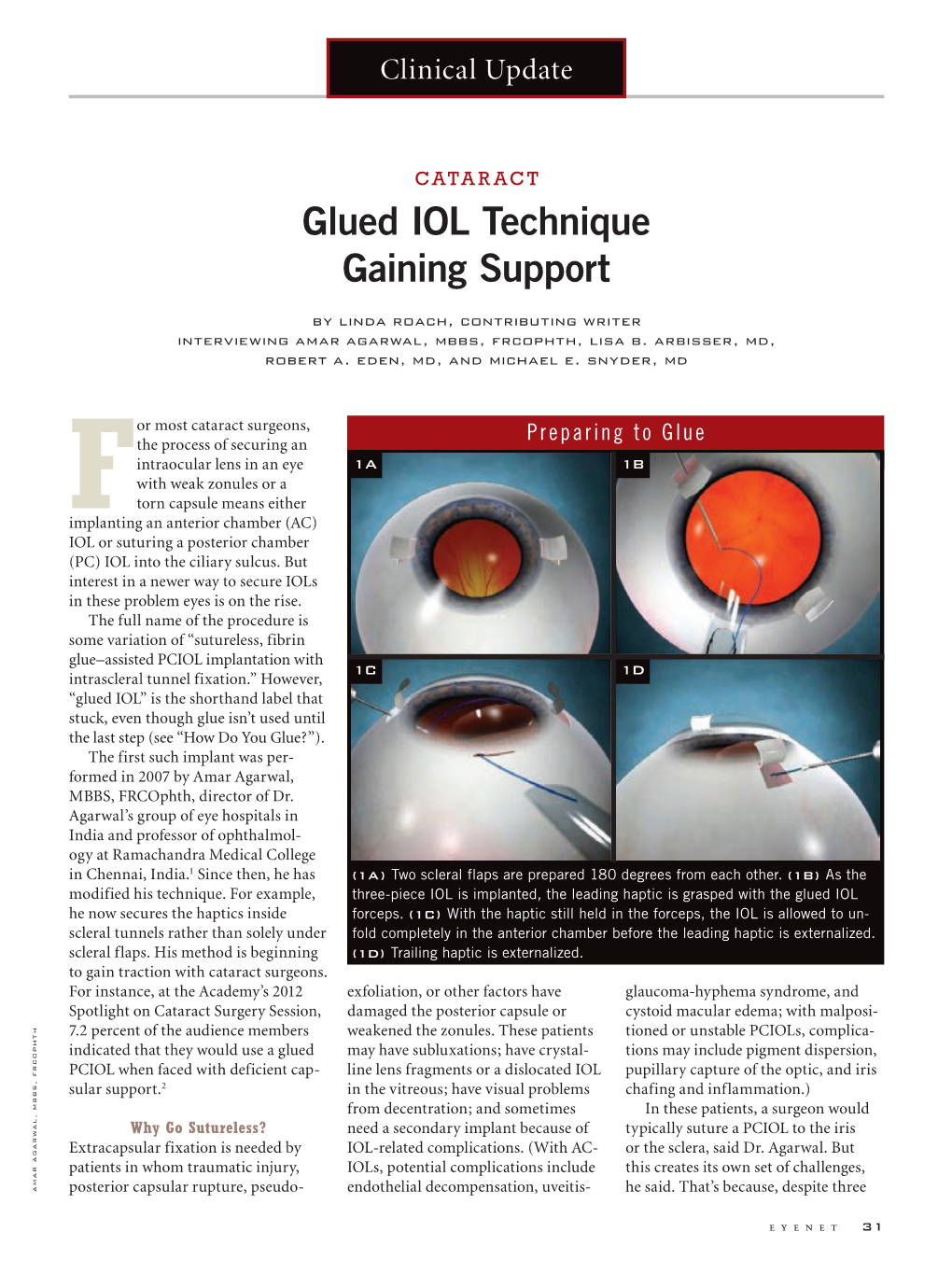
Glued IOL Technique Gaining Support
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

5267830313.Pdf
DR. AGARWAL’S EYE HOSPITAL LIMITED 1 CONTENTS Page No. Company Information 2 Financial Highlights 3 Notice to Shareholders 4 Directors’ Report 11 Management Discussion and Analysis 15 Corporate Governance Report 15 Auditors’ Certificate on Corporate Governance 26 Independent Auditors’ Report to the Members 28 Secretarial Compliance Certificate 32 Balance Sheet 36 Profit and Loss Account 37 Cash Flow Statement 38 Notes on Financial Statement 41 Attendance Slip and Proxy Form 59 2 DR. AGARWAL’S EYE HOSPITAL LIMITED COMPANY INFORMATION Board of Directors Dr. Amar Agarwal (Chairman cum Managing Director) Dr. Athiya Agarwal (Wholetime Director) Dr. Adil Agarwal (Wholetime Director) Dr. Anosh Agarwal (Wholetime Director) Dr. Jasvinder Singh Saroya Mr. M. R. G. Apparao Mr. Prabhat Toshniwal Mr. Sanjay Anand Auditors M/s. M. K. Dandeker & Co. Chartered Accountants, 244, Angappa Naicken Street, Chennai 600 001. Registered Office 19 (Old No.13), Cathedral Road, Chennai 600 086. Bankers (1) State Bank of India, Gopalapuram Branch, Chennai - 600 086. (2) State Bank of India, Industrial Finance Branch, Chennai 600 002. Share Transfer Agents Integrated Enterprises (India) Ltd. 2nd Floor, Kences Towers, No.1, Ramakrishna Street, North Usman Road, T.Nagar, Chennai 600 017. Tel: 2814 0801-03 Email: [email protected] DR. AGARWAL’S EYE HOSPITAL LIMITED HOSPITAL EYE AGARWAL’S DR. Financial Highlights Rs. in crore For the year ended 2012-13 2011-12 2010-11 2009-10 2008-09 2007-08 2006-07 2005-06 2004-05 2003-04 Total Income 109.73 105.68 104.01 -

Novel Yamane Technique Modification for Haptic Exposure After Glued Intrascleral Haptic Fixation
American Journal of Ophthalmology Case Reports 14 (2019) 101–104 Contents lists available at ScienceDirect American Journal of Ophthalmology Case Reports journal homepage: www.elsevier.com/locate/ajoc Case report Novel yamane technique modification for haptic exposure after glued intrascleral haptic fixation T ∗ Rachel A. Gelman, Sumit Garg Gavin Herbert Eye Institute, University of California, Irvine, 92697, United States ARTICLE INFO ABSTRACT Keywords: The field of intraocular lens fixation in the setting of inadequate capsular support is a dynamic one as surgical Yamane technique approaches are constantly evolving. There has been a paradigm shift towards the use of sutureless methods of Haptic exposure scleral fixation to avoid suture-related complications. In the latest described style of scleral fixation, IOLs can be Intraocular lens (IOL) secured without suture or “glue”, and rather with the creation of a flange on each haptic that allows for firm intrascleral fixation. We describe a modification of the flange technique to refixate patients with glued IOLs who developed haptic extrusion and required surgical intervention. 1. Introduction 48% of eyes with a sutured IOL. The risk of postoperative glaucoma was also found to be lower, occurring 16% of the time with glued IOLs 1.1. Sutureless techniques for scleral fixation versus 40% with sutured IOLs.5 Furthermore, the use of glue over su- ture precludes problems such as suture breakage and exposure, which In 2007, Agarwal et al. described the use of fibrin glue for fixation of in a retrospective study by McAllister et al. occurred at a rate of 6.1% a posterior chamber IOL in the setting of deficient capsular support in a and 11% respectively with the use of 10–0 polypropylene.2 Degradation technique referred to as “glued IOL fixation”. -

Posterior Chamber Scleral Fixation of Intraocular Lenses in Post
DOI: 10.7860/JCDR/2017/20989.9533 Original Article Posterior Chamber Scleral Fixation of Intraocular Lenses in Post- Ophthalmology Section Vitrectomised Aphakic Eyes FRANCIS KWASI OBENG1, VIPAN KUMAR VIG2, PREETAM SINGH3, RAJBIR SINGH4, BODHRAJ DHAWAN5, NIKHIL SAHAJPAL6 ABSTRACT Materials and Methods: Records of all patients who had Introduction: The best method of aphakia correction is in the undergone secondary PCSFIOL implantation with sutures bag implantation of Posterior Chamber Intraocular Lens (PCIOL). after combined PPV and lensectomy from 2010 to 2014 were When this ideal procedure is not possible due to lack of integrity reviewed retrospectively for visual outcomes and complications. of posterior capsule or zonules, the other alternatives are broadly Patients’ demographic data, indication for PPV, best corrected categorized into two: extraocular and intraocular. Whereas, the preoperative and postoperative visual acuities, complications former includes contact lenses and aphakic glasses, the latter of surgery, and indications of PCSFIOL and length of follow up ones are further divided into anterior and posterior chamber were collected and analyzed. methods. Anterior Chamber Intraocular Lenses (ACIOL) can be Results: A total of 148 eyes of 148 patients (127 males and with or without iris claw. At the posterior chamber, fixation of the 21 females) were identified. Mean age at surgery was 32.5+8 lenses can be with glue or sutures. years (range 2.5-73 years) with a mean follow up 23+14 months When there is combined Pars Plana Vitrectomy (PPV) and (range 3-114 months). A total of 95.27%, 2.70% and 2.02% lensectomy or if the indication of PPV is dropped nucleus or of patients had improvement, maintenance and worsening of intraocular lens, a modality of aphakia correction should be their final postoperative visual acuities respectively. -

Agarwal AR 19.Indd
Contents Page No Chairman’s Desk 3 Board of Directors 5 A Word from Chairman - Clinical Board 9 Industrial Update 12 Notice to Shareholders 15 Directors’ Report 29 Management Discussions and Analysis Report 46 Corporate Governance Report 50 A word from the CFO 61 Financial Highlights 62 Independent Auditor’s Report 65 Balance Sheet as at 31st March, 2019 72 Statement of Profit and Loss for the year ended 31st March 2019 73 Statement of changes in equity for the year ended 31st March 2019 74 Cash Flow Statement as on 31st March 2019 75 Notes Forming Part of the Financial Statements for the year ended 76 31st March 2019 Press Clippings 120 NABH Accredited 126 Route map to AGM venue 128 CORPORATE Chairman’s INFORMATION Desk DIRECTORS Dr. Amar Agarwal (DIN: 00435684) ..................... Chairman Cum Managing Director Dr. Athiya Agarwal (DIN: 01365659) .................... Whole-time Director Dr. Adil Agarwal (DIN: 01074272) ........................ Director Mr. Sanjay Anand (DIN: 02501139) ...................... Independent Director Mr T. R. Ramasubramanian (DIN: 08207929) ........ Independent Director Mrs. Lakshmmi Subramanian (DIN: 00001439) .... Independent Director CHIEF FINANCIAL OFFICER Dear Shareholders, Ms. Saradha Govindarajan I look back nearly 60 years to when we initially set out to build the first Eye care hospital under our name, and then to the journey thereafter, in nurturing it into the world-class Eye care institution it COMPANY SECRETARY & COMPLIANCE OFFICER has grown into today. Now the hospital chain in its 62nd year of service has a total presence of 22 Ms. Jully H. Jivani hospitals across India. Our motivation for the pursuit of our goals has not wavered a bit through this eventful and challenging journey.We believe we are best suited to lead the eye care space in the AUDITORS coming years M/s. -

Visually Significant Traumatic Cataract
CATARACT SURGERY COMPLEX CASE MANAGEMENT Section Editors: Thomas A. Oetting, MS, MD; Tal Raviv, MD; and Audrey R. Talley Rostov, MD eyetube.net Visually Significant Traumatic Cataract BY PRIYA NARANG, MS; AMAR AGARWAL, MS, FRCS, FRCOPHTH; H. BURKHARD DICK, MD, PHD; TIM SCHULTZ, MD; RICHARD J. MACKOOL, MD; RICHARD J. MACKOOL JR, MD; AND TAL RAVIV, MD CASE PRESENTATION A 50-year-old man presents with a visually significant (Courtesy of Priya Narang, MS, and Amar Agarwal, FRCS, FRCOphth.) traumatic cataract (following blunt trauma 5 years ago). About 7 clock hours of zonular loss (Figure 1) and phaco- donesis are present. Small wisps of vitreous are visible at the edge of the lens. How would you approach this case? —Case prepared by Tal Raviv, MD. (Courtesy of Tal Raviv, MD.) Figure 2. The design of the glued ECR and its positioning in the direction of dialysis. the hemi-ring segment portion and are designed to sit Figure 1. A traumatic cataract with 7 clock hours of zonu- within the fornix of the capsular bag. The scrolls engage lar loss and mild vitreous prolapse in a young patient. the margin of the capsulorhexis, and the haptic anchors the entire bag transsclerally (Figure 2). Once the scrolls PRIYA NARANG, MS, AND have engaged the capsulorhexis’ margin, pulling on the AMAR AGARWAL, MS, FRCS, FRCOPHTH exteriorized haptic centers the entire capsular bag com- Figure 1 shows traumatic subluxation of the lens with plex. Phacoemulsification then commences. The choice 7 clock hours of zonular loss. The clinical picture is sug- and positioning of the IOL depend on the degree and gestive of phacodonesis, and small wisps of vitreous are location of zonular disruption. -

REFRACTIVE Laser
4 Cover Story REFRACTIVE Laser QUEST FOR PERFECTION LASIK banks on mature technology and reduced complication rates to stay ahead of the competition by Dermot McGrath aser-assisted in situ how many patients fall under the terminally complication rates in recent years. keratomileusis (LASIK) has dissatisfied category over the long term, the “There has definitely been an been assessed and improved by fact that the FDA in the US received just improvement over the past few years which I still believe many more than a decade of clinical 140 “negative reports relating to LASIK” I would attribute to improved technology, “patients disappear studiesL and technological innovation since for the time period 1998-2006 suggests to with better preoperative diagnostics and from their surgeon’s the procedure was first introduced. As some observers that LASIK complication also much better patient screening in terms practices after the one one of the most popular elective surgical and/or dissatisfaction rates are probably of anterior and posterior surface, corneal year of ‘free’ follow- procedures in the world, with one of the under-reported. thickness, and even family history to help up care that most highest safety profiles, LASIK remains the A 2008 study on LASIK complications prevent complications such as post-LASIK provide. Consequently, primary dynamo driving today’s global carried out at Wills Eye Institute (J ectasia,” said Francesco Carones MD, refractive surgery market. Cataract Refract Surg. 2008 Jan;34(1):32- Co-founder and medical director of the I do believe we have However, given the huge volume of 9.), for instance, found that only 29 per Carones Ophthalmology Centre in been underestimating procedures performed since its inception, cent of patients referred for problems Milan, Italy. -

DENSE, DISLOCATED, BRUNESCENT CATARACT Approaching Cataract Surgery in a Monocular Patient
CATARACT SURGERY CASE FILES s DENSE, DISLOCATED, BRUNESCENT CATARACT Approaching cataract surgery in a monocular patient. BY ASHVIN AGARWAL, MS; MARJAN FARID, MD; P. DEE G. STEPHENSON, MD, FACS; AND AUDREY R. TALLEY ROSTOV, MD CASE PRESENTATION An 84-year-old Russian woman presents for a cataract surgery evaluation. The patient has a history of a failed graft, retinal detachment, and glaucoma in her right eye. Visual acuity is light perception in her right eye and count- ing fingers in her left. A slit-lamp examination of the patient’s left eye finds a dense cataract, an inferiorly dislocated lens, loose zonules, and phacodonesis (Figure). The cornea is clear, and endothelial cell density is normal. B-scan ultrasonography shows no retinal detachment. The IOP measures 15 mm Hg. Examination reveals no other significant findings. How would you proceed? What form of anesthesia would you use? What would your preferences be in terms of surgical technique and IOL? —Case prepared by Audrey R. Talley Rostov, MD Figure. Examination of the patient’s left eye shows a dense cataract and loose zonules. I would begin by making a conjuncti- were well tucked into the Scharioth val peritomy at the 3 and 9 clock hours tunnels, I would seal them with glue. I and two partial-thickness scleral flaps would end the case with pupilloplasty located 180º apart. I would also create to optimize the outcome. the SICS tunnel but leave it unopened. ASHVIN AGARWAL, MS After performing continuous curvilinear capsulorhexis, in order to ensure that Because the patient is almost blind the zonules were manipulated as little as and her right eye has undergone mul- possible, I would pull the lens into the tiple surgeries, I would first attempt to anterior chamber. -
Model Curriculum Handbook
Ministry of Health and Family Welfare Allied Health Section 2015-16 Model Curriculum Handbook OPTOMETRY Model Curriculum Handbook OPTOMETRY Ministry of Health and Family Welfare Allied Health Section Contents Contributors to drafting and review ............................................................................................................... 3 List of Abbreviations ..................................................................................................................................... 5 Chapter 1: Introduction to the Handbook.................................................................................................... 11 Who is an Allied and Healthcare Professional? ......................................................................................... 11 Scope and need for allied and healthcare professionals in the Indian healthcare system ............................ 11 Learning goals and objectives for allied and healthcare professionals ....................................................... 12 Introduction of new elements in allied and healthcare education .............................................................. 17 Competency-based curriculum ............................................................................................................. 17 Promoting self-directed learning of the professionals ........................................................................... 17 Credit hours vs traditional system ....................................................................................................... -

SHOULD LASIK BE REBRANDED? Experts Debate Whether the Leading Refractive Surgery Procedure Needs a New Name
COVER FOCUS COVER POINT/COUNTERPOINT: SHOULD LASIK BE REBRANDED? Experts debate whether the leading refractive surgery procedure needs a new name. BY SOOSAN JACOB, MS, FRCS, DNB; AMAR AGARWAL, MS, FRCS, FRCOPHTH; MARC MULLIE, MD, FRCSC; MICHAEL LAWLESS, MBBS, FRANZCO, FRACS; DAN Z. REINSTEIN, MD, MA(CANTAB), FRCSC, DABO, FRCOPHTH, FEBO; VANCE THOMPSON, MD; AND J. TREVOR WOODHAMS, MD Point: refractive surgery procedure. The advantages that this tech- nique offers are numerous. For starters, the absence of a flap A LASIK Rebrand is in Order and the use of a small incision together act to eliminate flap- By Soosan Jacob, MS, FRCS, DNB; Amar Agarwal, MS, related complications such as striae, flap dislodgement, and FRCS, FRCOphth; and Marc Mullie, MD, FRCSC epithelial ingrowth. Similarly, because of decreased disruption of the anterior corneal innervation, there is faster recovery Rebrand Refractive Surgery of corneal sensitivity and less patient experience of dry eye by Introducing a New Procedure than is seen with LASIK.3 Most important, the presence of the Soosan Jacob, MS, FRCS, DNB; and nearly intact anterior stromal layer of the cornea allows better Amar Agarwal, MS, FRCS, FRCOphth maintenance of biomechanical strength after SMILE compared Corneal refractive surgery has evolved with LASIK.4,5 The entire procedure is completed with a single over the years, progressing through techniques from cuts in the cornea (RK), to excimer laser surface ablation (PRK), to intrastromal ablation under a flap (LASIK). The last of these approaches has been the most successful technique thus AT A GLANCE far, with widespread worldwide acceptance and penetration. WHAT YOUR PEERS ARE SAYING The LASIK flap itself has evolved, from being created with a ABOUT LASIK REBRANDING mechanical microkeratome to being cut with a femtosecond • Instead of rebranding LASIK specifically, it could be laser. -

Glued Capsular Hook: Technique for Fibrin Glue-Assisted Sutureless
TECHNIQUE Glued capsular hook: Technique for fibrin glue–assisted sutureless transscleral fixation of the capsular bag in subluxated cataracts and intraocular lenses Soosan Jacob, MS, FRCS, DNB, Amar Agarwal, MS, FRCS, FRCOphth, Athiya Agarwal, MD, DO, Ashvin Agarwal, MS, Smita Narasimhan, MB BS, Dhivya Ashok Kumar, MD We describe a technique that uses a capsular hook to obtain sutureless fibrin glue–assisted trans- scleral fixation of the capsular bag. The hook passes through a sclerotomy created under a scleral flap and engages the capsulorhexis rim, providing scleral fixation intraoperatively and postoper- atively. A standard capsular tension ring expands the capsular fornix. The haptic of the hook is tucked into a scleral tunnel for postoperative fixation. The scleral flap is closed with fibrin glue. The glued capsular hook is used for subluxated cataracts and IOLs. It anchors the capsular bag to the sclera, providing vertical and horizontal stability, and stabilizes the bag intraoperatively and postoperatively. The technique was used in 7 patients, who were followed for more than 4 months. Financial Disclosure: Dr. Jacob has a patent pending for the glued capsular hook models. No other author has a financial or proprietary interest in any material or method mentioned. J Cataract Refract Surg 2014; 40:1958–1965 Q 2014 ASCRS and ESCRS Online Video The management of subluxated cataracts and intraoc- possibility of long-term suture-related complications. ular lenses (IOLs) depends on the degree of zonulo- We describe a technique that uses a glued capsular dialysis.1,2 For subluxations up to 3 to 4 clock hours, hook (Figure 1) to achieve sutureless fibrin glue–assis- a capsular tension ring (CTR) is often sufficient, but ted transscleral fixation of the capsular bag. -

Image of the Month the Human Choroid, Reconstructed in 3D
APRIL 2016 # 29 Image of the Month Upfront Profession Sitting Down With The human choroid, Growing your own Benchmarking your practice Amar Agarwal, Chairman of reconstructed in 3D crystalline lens against your peers Dr Agarwal’s Eye Hospital 03 08 – 10 60 – 64 66 – 67 www.theophthalmologist.com DUAL-SEGMENT PUMP TECHNOLOGY + Precise fluidics + Pulsatile-free + Quick vacuum rise + Versatile performance PERFORMANCE IN EVERY DETAIL Superior chamber stability through superior engineering.†,1,2 That’s the Centurion® Effect. Active Fluidics™ Technology • Helps to Maintain Chamber Stability: Detects and compensates to help provide superior chamber stability3 compared to INFINITI®4 • Less Surge: Less surge at any tested vacuum level3,5 • More Consistent IOP4 : Up to 80% less surge area3,5 Contact your Alcon representative to schedule a demonstration and experience the Centurion® Effect for yourself. †As compared to the INFINITI® Vision System, bottle gravity system. 1. Lorente R, Fanney D, Injev V, Sharif-Kashani P. Quantification of occlusion break surge in peristaltic-based phacoemulsification systems. ASCRS-ASOA Symposium and Congress; April 25-29, 2014; Boston, USA.2. Nicoli M, Miller K, Dimalanta R, Loke D; Jules Stein Eye Institute, UCLA. IOP Stability Measurement and Comparison Between Gravity-Fed and Actively Controlled Phacoemulsification Systems. 2014. 3. Sharif-Kashani P, Fanney D, Injev V. Comparison of occlusion break responses and vacuum rise times of phacoemulsification systems. BMC Ophthalmol. 2014;14:96. 4. Nicoli CM, Dimalanta R, Miller K. Experimental anterior chamber maintenance in active versus passive phacoemulsification fluidics systems. J Cataract Refract Surg. 2016;42(1):157-162. 5. Alcon data on file. -

Educational Qualifications
CURRICULUM VITAE PERSONAL NAME : Dr. Sunita Agarwal I have been fortunate to be born in a family of ophthalmologists. My grandfather Dr. Raghvir S. Agarwal was a noted ophthalmologist of his time in India. My father Dr. Jaivir Agarwal is the founder of Dr. Agarwal ‘s Eye Institute, Chennai, mother Dr. Mrs. Tahira Agarwal is also a renowned ophthalmic surgeon currently practicing as a corneal specialist. My brother Dr. Amar Agarwal and myself both are ophthalmic surgeons, extensively engaged in ophthalmic research, teaching are currently practicing with our parents at Chennai. Dr. Athiya Agarwal, wife of Dr Amar Agarwal is also a part of the team. EDUCATIONAL QUALIFICATIONS 1. COMPLETED MATRICULATION FROM SACRED HEART CHURCH PARK SCHOOL IN 1975 I had a complete childhood with schooling from one of the finest institutions in the country. As is well known convent education brings with it a flare to the child and close proximity with God. In any format the individual gets to think of the less fortunate and realizes the pain and anguish of our school teachers and convent nuns. I was extremely mischievous and was called out to the Principals office very often still in this developed a close camaraderie with my Principal Teacher Sister Clare. So much so that till today she remembers me fondly of tying my unruly hair in her own ribbons or admonishing me for one of my little crimes. I also happened to be the School pupil leader in the my last year occasion came on a day when I had just come back from Delhi after winning the national gold medal for swimming for 1974, and as I entered school the election had taken place in my absence, this was one of few times I saw tears (of joy) in my fathers year.