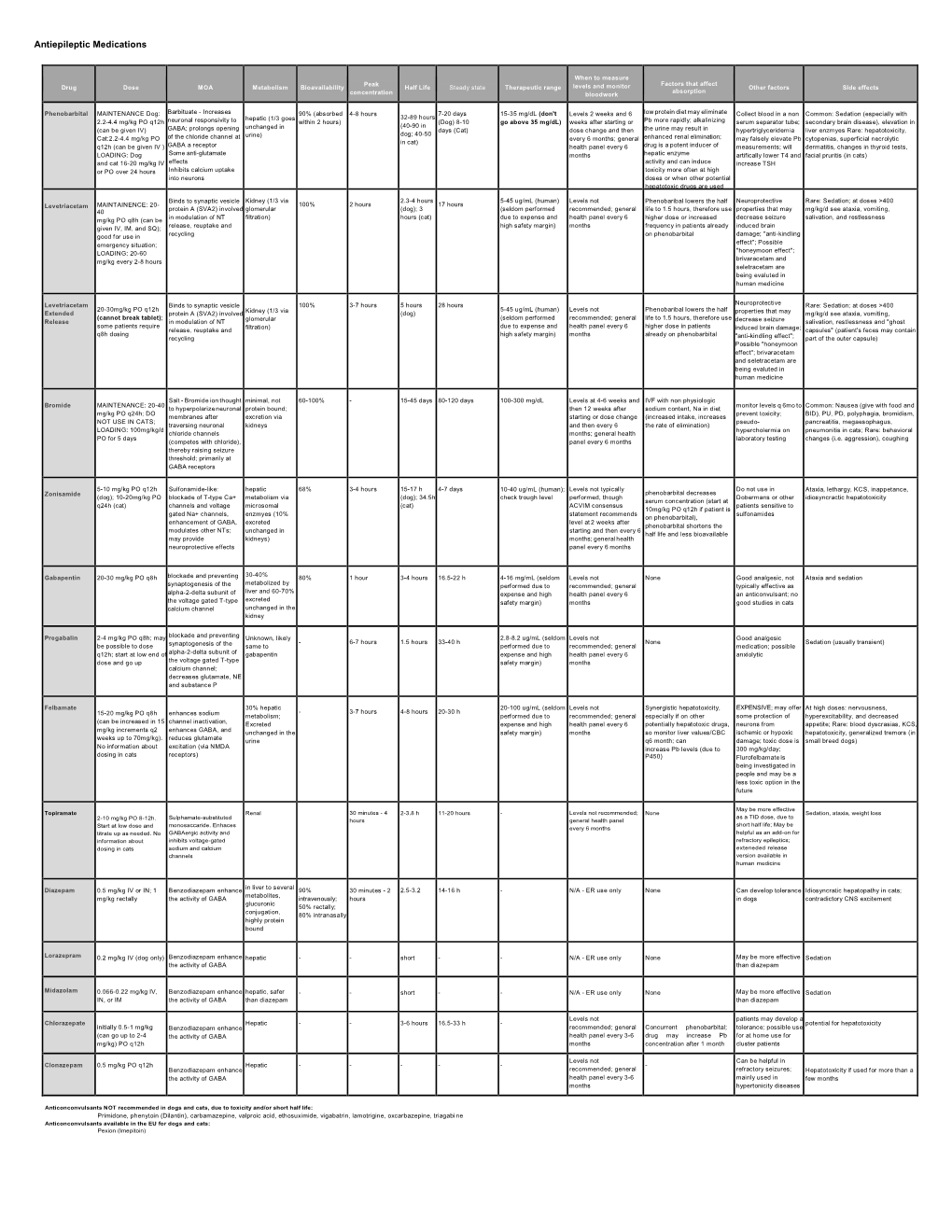
Antiepileptic Medications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

With LAMOTRIGINE IN
were independent of seizure type. Cardiac abnormalities occurring in epilepsy with GTCS may potentially facilitate sudden cardiac death (SUDEP). ETHOSUXIMIDE, VALPROIC ACID, AND LAMOTRIGINE IN CHILDHOOD ABSENCE EPILEPSY Efficacy, tolerability, and neuropsychological effects of ethosuximide, valproic acid, and lamotrigine in children with newly diagnosed childhood absence epilepsy were compared in a double-blind, randomized, controlled clinical trial performed at six centers in the US and organized as a Study Group. Drug doses were incrementally increased until freedom from seizures or highest tolerable dose was reached, Primary outcome was freedom from treatment failure after 16 weeks therapy, and secondary outcome was attentional dysfunction. In a total of 453 children, the freedom-from-failure rates after 16 weeks were similar for ethosuximide (53%) and valproic acid (58%), and higher than the rate for lamotrigine (29%) (P<0.001). Attentional dysfunction was more common with valproic acid (49%) than with ethosuximide (33%) (P=0.03). (Glauser TA, Cnaan A, Shinnar S, et al. Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy. N Engl J Med March 4 2010;362:790-799). (Reprints: Dr Tracy A Glauser, Cincinnati Children's Hospital, 3333 Burnett Ave, MLC 2015, Cincinnati, OH 45229. E- mail: [email protected]). COMMENT. "Older is better," is the conclusion of Vining EPG, in an editorial (N Engl J Med 2010;362:843-845). As generally accepted in US practice and confirmed by the above controlled trial, ethosuximide from the 1950s is the optimal initial therapy for childhood absence epilepsy without GTCS. Ethosuximide is equal to valproic acid in seizure control and superior in effects on attention. -

Phenobarbital Brand Name: Phenobarb
Generic Name: Phenobarbital Brand Name: Phenobarb What Is It Used For? Decreasing seizure activity in various types of seizures. Especially useful for controlling seizures in neonates and infants Given intravenously in the emergency department for status epilepticus. How Long Does The Oral Medicine Take to Work? 10-30 days What Are The Important Safety Concerns? When first starting the medicine, your child may be slightly drowsy and/or dizzy. Only adjust the dosage as recommended by your health care provider. They will usually increase this medication slowly to avoid side effects. Never increase the dosage more than once per week unless directed otherwise. Once you have started with one brand of the medication stay with it. Avoid switching between different brands. Check with your pharmacist before taking herbal medications and/or over-the- counter medications. They may have adverse effects if taken with anti-seizure medications. Do not stop taking this medication suddenly because this could result in seizures. It is important to keep a record of your child’s seizures and side effects to determine how well they are responding to the medication. Does My Child Need Bloodwork With This Medication? Routine blood work may be done to help determine the best dosage for your child, and also if they have side effects to the medication. If your child is required to have blood work it must be done BEFORE they get the medication. This is called a trough level. This level usually falls between 65 and 170. A blood test may be done before starting this medication to check your child’s liver function and blood counts. -

18 December 2020 – to Date)
(18 December 2020 – to date) MEDICINES AND RELATED SUBSTANCES ACT 101 OF 1965 (Gazette No. 1171, Notice No. 1002 dated 7 July 1965. Commencement date: 1 April 1966 [Proc. No. 94, Gazette No. 1413] SCHEDULES Government Notice 935 in Government Gazette 31387 dated 5 September 2008. Commencement date: 5 September 2008. As amended by: Government Notice R1230 in Government Gazette 32838 dated 31 December 2009. Commencement date: 31 December 2009. Government Notice R227 in Government Gazette 35149 dated 15 March 2012. Commencement date: 15 March 2012. Government Notice R674 in Government Gazette 36827 dated 13 September 2013. Commencement date: 13 September 2013. Government Notice R690 in Government Gazette 36850 dated 20 September 2013. Commencement date: 20 September 2013. Government Notice R104 in Government Gazette 37318 dated 11 February 2014. Commencement date: 11 February 2014. Government Notice R352 in Government Gazette 37622 dated 8 May 2014. Commencement date: 8 May 2014. Government Notice R234 in Government Gazette 38586 dated 20 March 2015. Commencement date: 20 March 2015. Government Notice 254 in Government Gazette 39815 dated 15 March 2016. Commencement date: 15 March 2016. Government Notice 620 in Government Gazette 40041 dated 3 June 2016. Commencement date: 3 June 2016. Prepared by: Page 2 of 199 Government Notice 748 in Government Gazette 41009 dated 28 July 2017. Commencement date: 28 July 2017. Government Notice 1261 in Government Gazette 41256 dated 17 November 2017. Commencement date: 17 November 2017. Government Notice R1098 in Government Gazette 41971 dated 12 October 2018. Commencement date: 12 October 2018. Government Notice R1262 in Government Gazette 42052 dated 23 November 2018. -

Therapeutic Class Overview Anticonvulsants
Therapeutic Class Overview Anticonvulsants INTRODUCTION Epilepsy is a disease of the brain defined by any of the following (Fisher et al 2014): ○ At least 2 unprovoked (or reflex) seizures occurring > 24 hours apart; ○ 1 unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after 2 unprovoked seizures, occurring over the next 10 years; ○ Diagnosis of an epilepsy syndrome. Types of seizures include generalized seizures, focal (partial) seizures, and status epilepticus (Centers for Disease Control and Prevention [CDC] 2018, Epilepsy Foundation 2016). ○ Generalized seizures affect both sides of the brain and include: . Tonic-clonic (grand mal): begin with stiffening of the limbs, followed by jerking of the limbs and face . Myoclonic: characterized by rapid, brief contractions of body muscles, usually on both sides of the body at the same time . Atonic: characterized by abrupt loss of muscle tone; they are also called drop attacks or akinetic seizures and can result in injury due to falls . Absence (petit mal): characterized by brief lapses of awareness, sometimes with staring, that begin and end abruptly; they are more common in children than adults and may be accompanied by brief myoclonic jerking of the eyelids or facial muscles, a loss of muscle tone, or automatisms. ○ Focal seizures are located in just 1 area of the brain and include: . Simple: affect a small part of the brain; can affect movement, sensations, and emotion, without a loss of consciousness . Complex: affect a larger area of the brain than simple focal seizures and the patient loses awareness; episodes typically begin with a blank stare, followed by chewing movements, picking at or fumbling with clothing, mumbling, and performing repeated unorganized movements or wandering; they may also be called “temporal lobe epilepsy” or “psychomotor epilepsy” . -

Pexion, Imepitoin
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE VETERINARY MEDICINAL PRODUCT Pexion 100 mg tablets for dogs Pexion 400 mg tablets for dogs 2. QUALITATIVE AND QUANTITATIVE COMPOSITION One tablet contains: Active substance: Imepitoin 100 mg Imepitoin 400 mg For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Tablets White, oblong, half-scored tablets with embedded logo “I 01” (100 mg) or “I 02” (400 mg) on one side. The tablet can be divided into equal halves. 4. CLINICAL PARTICULARS 4.1 Target species Dog 4.2 Indications for use, specifying the target species For the reduction of the frequency of generalised seizures due to idiopathic epilepsy in dogs for use after careful evaluation of alternative treatment options. 4.3 Contraindications Do not use in case of hypersensitivity to the active substance or to any of the excipients. Do not use in dogs with severely impaired hepatic function, severe renal or severe cardiovascular disorders (see section 4.7). 4.4 Special warnings The pharmacological response to imepitoin may vary and efficacy may not be complete. Nevertheless imepitoin is considered to be a suitable treatment option in some dogs because of its safety profile (see section 5.1). On treatment, some dogs will be free of seizures, in other dogs a reduction of the number of seizures will be observed, whilst others may be non-responders. In non-responders, an increase in seizure frequency may be observed. Should seizures not be adequately controlled, further diagnostic measures and other antiepileptic treatment should be considered. The benefit/risk assessment for the individual dog should take into account the details in the product literature. -

Pharmacokinetic Drug–Drug Interactions Among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients
International Journal of Molecular Sciences Review Pharmacokinetic Drug–Drug Interactions among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients Marta Kara´zniewicz-Łada 1 , Anna K. Główka 2 , Aniceta A. Mikulska 1 and Franciszek K. Główka 1,* 1 Department of Physical Pharmacy and Pharmacokinetics, Poznan University of Medical Sciences, 60-781 Pozna´n,Poland; [email protected] (M.K.-Ł.); [email protected] (A.A.M.) 2 Department of Bromatology, Poznan University of Medical Sciences, 60-354 Pozna´n,Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-(0)61-854-64-37 Abstract: Anti-epileptic drugs (AEDs) are an important group of drugs of several generations, rang- ing from the oldest phenobarbital (1912) to the most recent cenobamate (2019). Cannabidiol (CBD) is increasingly used to treat epilepsy. The outbreak of the SARS-CoV-2 pandemic in 2019 created new challenges in the effective treatment of epilepsy in COVID-19 patients. The purpose of this review is to present data from the last few years on drug–drug interactions among of AEDs, as well as AEDs with other drugs, nutrients and food. Literature data was collected mainly in PubMed, as well as google base. The most important pharmacokinetic parameters of the chosen 29 AEDs, mechanism of action and clinical application, as well as their biotransformation, are presented. We pay a special attention to the new potential interactions of the applied first-generation AEDs (carba- Citation: Kara´zniewicz-Łada,M.; mazepine, oxcarbazepine, phenytoin, phenobarbital and primidone), on decreased concentration Główka, A.K.; Mikulska, A.A.; of some medications (atazanavir and remdesivir), or their compositions (darunavir/cobicistat and Główka, F.K. -
CDHO Factsheet Epilepsy
Disease/Medical Condition EPILEPSY Date of Publication: August 7, 2014 (also known as “seizure disorder”) Is the initiation of non-invasive dental hygiene procedures* contra-indicated? No Is medical consult advised? ...................................... No (assuming patient/client is already under medical care for epilepsy, which is well controlled) Is the initiation of invasive dental hygiene procedures contra-indicated?** No Is medical consult advised? ....................................... Possibly (e.g., if there is medication non-compliance) Is medical clearance required? .................................. Possibly (e.g., if there is significant risk of seizure; patient/ client should be seizure-free for several months to be considered controlled) Is antibiotic prophylaxis required? .............................. No Is postponing treatment advised? ............................... No (assuming patient/client is already under medical care for epilepsy, which is well controlled and for which there are no anticipated exacerbating factors in the office setting) Oral management implications Important considerations in the management of epileptic patients/clients are prevention of seizures in the dental chair and preparation for managing seizures if they occur. When a patient/client responds positively to questions about seizures/ epilepsy during health history taking, further information should be obtained. Based on the patient/client’s responses, the dental hygienist may choose to postpone treatment to avoid triggering a seizure in the dental chair. It is valuable for the dental hygienist to know what factors have the potential to exacerbate epileptic seizures in a particular patient/client in order that trigger stimuli can be avoided. The dental hygienist can reduce stress and anxiety by explaining procedures before starting. Bright light should be kept out of the patient/client’s eyes, and dark glasses may assist with this. -

Evaluation of Pexion® (Imepitoin) for Treatment of Storm Anxiety in Dogs: a Randomised, Double-Blind, Placebo-Controlled Trial
Received: 20 July 2020 Revised: 7 October 2020 Accepted: 3 December 2020 DOI: 10.1002/vetr.18 ORIGINAL RESEARCH Evaluation of Pexion® (imepitoin) for treatment of storm anxiety in dogs: A randomised, double-blind, placebo-controlled trial Irina Perdew1 Carrie Emke1 Brianna Johnson1 Vaidehi Dixit2 Yukun Song2 Emily H. Griffith2 Philip Watson3 Margaret E. Gruen1 1 Department of Clinical Sciences, North Abstract Carolina State University College of Background: While often grouped with other noise aversions, fearful Veterinary Medicine, Raleigh, North Carolina, USA behaviour during storms is considered more complex than noise aversion 2 Department of Statistics, North Carolina alone. The objective here was to assess the effect of imepitoin for the treat- State University College of Sciences, Raleigh, ment of storm anxiety in dogs. North Carolina, USA Methods: In this double-blind, placebo-controlled randomised study, eligible 3 Ingelheim am Rhein, Boehringer-Ingelheim dogs completed a baseline then were randomised to receive either imepitoin Vetmedica GmbH, Ludwigshafen am Rhein, (n = 30; 30 mg/kg BID) or placebo (n = 15) for 28 days. During storms, owners Germany rated their dog’s intensity for 16 behaviours using a Likert scale. Weekly, own- Correspondence ers rated intensity and frequency of these behaviours. Summary scores were Margaret E. Gruen, Department of Clinical compared to baseline and between groups. Sciences, North Carolina State University Results and Conclusions: Imepitoin was significantly superior to placebo in College of Veterinary Medicine, 1060 William Moore Drive, Raleigh NC 27607, USA. storm logs and weekly surveys for weeks 2 and 4, and in the end-of-study sur- Email: [email protected] vey. -

Pentobarbital Sodium
PENTobarbital Sodium Brand names Nembutal Sodium Medication error Look-alike, sound-alike drug names. Tall man letters (not FDA approved) are recommended potential to decrease confusion between PENTobarbital and PHENobarbital.(1,2) ISMP recommends the following tall man letters (not FDA approved): PENTobarbital.(30) Contraindications Contraindications: In patients with known hypersensitivity to barbiturates or any com- and warnings ponent of the formulation.(2) If an allergic or hypersensitivity reaction or a life-threatening adverse event occurs, rapid substitution of an alternative agent may be necessary. If pentobarbital is discontinued due to development of a rash, an anticonvulsant that is structurally dissimilar should be used (i.e., nonaromatic). (See Rare Adverse Effects in the Comments section.) Also contraindicated in patients with a history of manifest or latent porphyria.(2) Warnings: Rapid administration may cause respiratory depression, apnea, laryngospasm, or vasodilation with hypotension.(2) Should be withdrawn gradually if large doses have been used for prolonged periods.(2) Paradoxical excitement may occur or important symptoms could be masked when given to patients with acute or chronic pain.(2) May be habit forming. Infusion-related Respiratory depression and arrest requiring mechanical ventilation may occur. Monitor cautions oxygen saturation. If hypotension occurs, the infusion rate should be decreased and/or the patient should be treated with IV fluids and/or vasopressors. Pentobarbital is an alkaline solution (pH = 9–10.5); therefore, extravasation may cause tissue necrosis.(2) (See Appendix E for management.) Gangrene may occur following inadvertent intra-arterial injection.(2) Dosage Medically induced coma (for persistently elevated intracranial pressure (ICP) or refractory status epilepticus): Patient should be intubated and mechanically ventilated. -

Mechanisms of Action of Antiepileptic Drugs
Review Mechanisms of action of antiepileptic drugs Epilepsy affects up to 1% of the general population and causes substantial disability. The management of seizures in patients with epilepsy relies heavily on antiepileptic drugs (AEDs). Phenobarbital, phenytoin, carbamazepine and valproic acid have been the primary medications used to treat epilepsy for several decades. Since 1993 several AEDs have been approved by the US FDA for use in epilepsy. The choice of the AED is based primarily on the seizure type, spectrum of clinical activity, side effect profile and patient characteristics such as age, comorbidities and concurrent medical treatments. Those AEDs with broad- spectrum activity are often found to exert an action at more than one molecular target. This article will review the proposed mechanisms of action of marketed AEDs in the US and discuss the future of AEDs in development. 1 KEYWORDS: AEDs anticonvulsant drugs antiepileptic drugs epilepsy Aaron M Cook mechanism of action seizures & Meriem K Bensalem-Owen† The therapeutic armamentarium for the treat- patients with refractory seizures. The aim of this 1UK HealthCare, 800 Rose St. H-109, ment of seizures has broadened significantly article is to discuss the past, present and future of Lexington, KY 40536-0293, USA †Author for correspondence: over the past decade [1]. Many of the newer AED pharmacology and mechanisms of action. College of Medicine, Department of anti epileptic drugs (AEDs) have clinical advan- Neurology, University of Kentucky, 800 Rose Street, Room L-455, tages over older, so-called ‘first-generation’ First-generation AEDs Lexington, KY 40536, USA AEDs in that they are more predictable in their Broadly, the mechanisms of action of AEDs can Tel.: +1 859 323 0229 Fax: +1 859 323 5943 dose–response profile and typically are associ- be categorized by their effects on the neuronal [email protected] ated with less drug–drug interactions. -

Idiopathic Epilepsy in Dogs – Part One: Patient Approach
Vet Times The website for the veterinary profession https://www.vettimes.co.uk Idiopathic epilepsy in dogs – part one: patient approach Author : Jacques Penderis, Holger Volk Categories : Vets Date : February 9, 2015 Dogs with recurrent epileptic seizures, and where no interictal neurological deficits or abnormalities on routine diagnostic tests are evident, have traditionally been defined as having “idiopathic epilepsy”. Rather than being a specific, single diagnosis, it is probable idiopathic epilepsy represents a complex interplay between genetic predisposition and intrinsic and extrinsic environmental factors, and the term “presumed genetic” has also been suggested to define these patients. A genetic basis for idiopathic epilepsy has been proposed in a number of breeds, including the golden retriever, Labrador retriever, Bernese mountain dog, Irish wolfhound, English springer spaniel, Keeshond, Hungarian vizsla, standard poodle, border collie and Finnish spitz (Viitmaa et al, 2013) and a possible susceptibility locus for epileptic seizures has been characterised in the Belgian shepherd dog (Seppälä et al, 2012). Reflecting its importance in veterinary medicine, idiopathic epilepsy is reported as the most common chronic neurological disease in dogs, with a prevalence of around 0.6 per cent in first opinion practice. Generalised seizures (where there is impairment of consciousness) are the most common type of epileptic seizure in dogs, while partial seizures appear to be relatively more common in cats; this, in part, represents the tendency for dogs with idiopathic epilepsy to have generalised seizures, or focal seizures with rapid secondary generalisation. The accurate description of generalised seizures in a patient with suspected idiopathic epilepsy is important, firstly to differentiate the episodes from other causes of collapse (for example, syncope) and secondly because the presence of generalised seizures is one of the criteria for making a diagnosis of idiopathic epilepsy. -

Diazepam and Kava Combination Article
Journal of Advanced Research (2014) 5, 587–594 Cairo University Journal of Advanced Research ORIGINAL ARTICLE Enhanced efficacy and reduced side effects of diazepam by kava combination Rasha A. Tawfiq a, Noha N. Nassar b,*, Wafaa I. El-Eraky c, Ezzeldein S. El-Denshary b a Egyptian Patent Office, Academy of Scientific Research and Technology, 101 Kasr El-Eini St., Cairo, Egypt b Department of Pharmacology and Toxicology, Faculty of Pharmacy, Cairo University, Kasr El-Eini St., Cairo, Egypt c Department of Pharmacology, National Research Center, El-Tahrir St., Giza, Egypt ARTICLE INFO ABSTRACT Article history: The long term use of antiepileptic drugs possesses many unwanted effects; thus, new safe com- Received 2 April 2013 binations are urgently mandated. Hence, the present study aimed to investigate the anticonvul- Received in revised form 18 July 2013 sant effect of kava alone or in combination with a synthetic anticonvulsant drug, diazepam Accepted 15 August 2013 (DZ). To this end, female Wistar rats were divided into two subsets, each comprising 6 groups Available online 22 August 2013 as follows: group (i) received 1% Tween 80 p.o. and served as control, while groups (ii) and (iii) received kava at two dose levels (100 and 200 mg/kg, p.o.). The remaining three groups received Keywords: (iv) DZ alone (10 mg/kg p.o.) or kava in combination with DZ (v) (5 mg/kg, p.o.) or (vi) (10 mg/ Kava kg, p.o.). Results of the present study revealed that kava increased the maximal electroshock Diazepam seizure threshold (MEST) and enhanced the anticonvulsant effect of diazepam following both Anticonvulsant acute and chronic treatment.