Idiopathic Epilepsy in Dogs – Part One: Patient Approach
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

18 December 2020 – to Date)
(18 December 2020 – to date) MEDICINES AND RELATED SUBSTANCES ACT 101 OF 1965 (Gazette No. 1171, Notice No. 1002 dated 7 July 1965. Commencement date: 1 April 1966 [Proc. No. 94, Gazette No. 1413] SCHEDULES Government Notice 935 in Government Gazette 31387 dated 5 September 2008. Commencement date: 5 September 2008. As amended by: Government Notice R1230 in Government Gazette 32838 dated 31 December 2009. Commencement date: 31 December 2009. Government Notice R227 in Government Gazette 35149 dated 15 March 2012. Commencement date: 15 March 2012. Government Notice R674 in Government Gazette 36827 dated 13 September 2013. Commencement date: 13 September 2013. Government Notice R690 in Government Gazette 36850 dated 20 September 2013. Commencement date: 20 September 2013. Government Notice R104 in Government Gazette 37318 dated 11 February 2014. Commencement date: 11 February 2014. Government Notice R352 in Government Gazette 37622 dated 8 May 2014. Commencement date: 8 May 2014. Government Notice R234 in Government Gazette 38586 dated 20 March 2015. Commencement date: 20 March 2015. Government Notice 254 in Government Gazette 39815 dated 15 March 2016. Commencement date: 15 March 2016. Government Notice 620 in Government Gazette 40041 dated 3 June 2016. Commencement date: 3 June 2016. Prepared by: Page 2 of 199 Government Notice 748 in Government Gazette 41009 dated 28 July 2017. Commencement date: 28 July 2017. Government Notice 1261 in Government Gazette 41256 dated 17 November 2017. Commencement date: 17 November 2017. Government Notice R1098 in Government Gazette 41971 dated 12 October 2018. Commencement date: 12 October 2018. Government Notice R1262 in Government Gazette 42052 dated 23 November 2018. -

Pexion, Imepitoin
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE VETERINARY MEDICINAL PRODUCT Pexion 100 mg tablets for dogs Pexion 400 mg tablets for dogs 2. QUALITATIVE AND QUANTITATIVE COMPOSITION One tablet contains: Active substance: Imepitoin 100 mg Imepitoin 400 mg For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Tablets White, oblong, half-scored tablets with embedded logo “I 01” (100 mg) or “I 02” (400 mg) on one side. The tablet can be divided into equal halves. 4. CLINICAL PARTICULARS 4.1 Target species Dog 4.2 Indications for use, specifying the target species For the reduction of the frequency of generalised seizures due to idiopathic epilepsy in dogs for use after careful evaluation of alternative treatment options. 4.3 Contraindications Do not use in case of hypersensitivity to the active substance or to any of the excipients. Do not use in dogs with severely impaired hepatic function, severe renal or severe cardiovascular disorders (see section 4.7). 4.4 Special warnings The pharmacological response to imepitoin may vary and efficacy may not be complete. Nevertheless imepitoin is considered to be a suitable treatment option in some dogs because of its safety profile (see section 5.1). On treatment, some dogs will be free of seizures, in other dogs a reduction of the number of seizures will be observed, whilst others may be non-responders. In non-responders, an increase in seizure frequency may be observed. Should seizures not be adequately controlled, further diagnostic measures and other antiepileptic treatment should be considered. The benefit/risk assessment for the individual dog should take into account the details in the product literature. -

Evaluation of Pexion® (Imepitoin) for Treatment of Storm Anxiety in Dogs: a Randomised, Double-Blind, Placebo-Controlled Trial
Received: 20 July 2020 Revised: 7 October 2020 Accepted: 3 December 2020 DOI: 10.1002/vetr.18 ORIGINAL RESEARCH Evaluation of Pexion® (imepitoin) for treatment of storm anxiety in dogs: A randomised, double-blind, placebo-controlled trial Irina Perdew1 Carrie Emke1 Brianna Johnson1 Vaidehi Dixit2 Yukun Song2 Emily H. Griffith2 Philip Watson3 Margaret E. Gruen1 1 Department of Clinical Sciences, North Abstract Carolina State University College of Background: While often grouped with other noise aversions, fearful Veterinary Medicine, Raleigh, North Carolina, USA behaviour during storms is considered more complex than noise aversion 2 Department of Statistics, North Carolina alone. The objective here was to assess the effect of imepitoin for the treat- State University College of Sciences, Raleigh, ment of storm anxiety in dogs. North Carolina, USA Methods: In this double-blind, placebo-controlled randomised study, eligible 3 Ingelheim am Rhein, Boehringer-Ingelheim dogs completed a baseline then were randomised to receive either imepitoin Vetmedica GmbH, Ludwigshafen am Rhein, (n = 30; 30 mg/kg BID) or placebo (n = 15) for 28 days. During storms, owners Germany rated their dog’s intensity for 16 behaviours using a Likert scale. Weekly, own- Correspondence ers rated intensity and frequency of these behaviours. Summary scores were Margaret E. Gruen, Department of Clinical compared to baseline and between groups. Sciences, North Carolina State University Results and Conclusions: Imepitoin was significantly superior to placebo in College of Veterinary Medicine, 1060 William Moore Drive, Raleigh NC 27607, USA. storm logs and weekly surveys for weeks 2 and 4, and in the end-of-study sur- Email: [email protected] vey. -

WSAVA List of Essential Medicines for Cats and Dogs
The World Small Animal Veterinary Association (WSAVA) List of Essential Medicines for Cats and Dogs Version 1; January 20th, 2020 Members of the WSAVA Therapeutic Guidelines Group (TGG) Steagall PV, Pelligand L, Page SW, Bourgeois M, Weese S, Manigot G, Dublin D, Ferreira JP, Guardabassi L © 2020 WSAVA All Rights Reserved Contents Background ................................................................................................................................... 2 Definition ...................................................................................................................................... 2 Using the List of Essential Medicines ............................................................................................ 2 Criteria for selection of essential medicines ................................................................................. 3 Anaesthetic, analgesic, sedative and emergency drugs ............................................................... 4 Antimicrobial drugs ....................................................................................................................... 7 Antibacterial and antiprotozoal drugs ....................................................................................... 7 Systemic administration ........................................................................................................ 7 Topical administration ........................................................................................................... 9 Antifungal drugs ..................................................................................................................... -

Progress Report on New Antiepileptic Drugs
Epilepsy Research (2013) 103, 2—30 j ournal homepage: www.elsevier.com/locate/epilepsyres REVIEW Progress report on new antiepileptic drugs: A summary of the Eleventh Eilat Conference (EILAT XI) a,∗ b c d Meir Bialer , Svein I. Johannessen , René H. Levy , Emilio Perucca , e f Torbjörn Tomson ,H. Steve White a Institute for Drug Research, School of Pharmacy and David R. Bloom Center for Pharmacy, Faculty of Medicine, Ein Karem, The Hebrew University of Jerusalem, 91120 Jerusalem, Israel b The National Center for Epilepsy, Sandvika, and Department of Pharmacology, Oslo University Hospital, Oslo, Norway c Department of Pharmaceutics and Neurological Surgery, University of Washington, Seattle, Washington, WA, USA d Clinical Pharmacology Unit, Department of Internal Medicine and Therapeutics, University of Pavia, and National Institute of Neurology IRCCS C. Mondino Foundation, Pavia, Italy e Department of Clinical Neuroscience, Karolinska Institute, Stockholm, Sweden f Department of Pharmacology and Toxicology, University of Utah, Salt Lake City, UT, USA Received 13 September 2012; accepted 8 October 2012 Available online 4 December 2012 KEYWORDS Summary The Eleventh Eilat Conference on New Antiepileptic Drugs (AEDs)-EILAT XI, took place in Eilat, Israel from the 6th to 10th of May 2012. About 100 basic scientists, clinical phar- Antiepileptic drugs; macologists and neurologists from 20 countries attended the conference, whose main themes Drug development; Epilepsy; included ‘‘Indications overlapping with epilepsy’’ and ‘‘Securing the successful development Pharmacology; of an investigational antiepileptic drug in the current environment’’. Consistent with previ- ous formats of this conference, a large part of the program was devoted to a review of AEDs Clinical trials; Conference in development, as well as updates on AEDs introduced since 1994. -

The Evidence Behind the Treatment of Canine Idiopathic Epilepsy
The Evidence Behind the Treatment of Canine Idiopathic Epilepsy A Knowledge Summary by Marios Charalambous DVM GPCert(Neuro) RSciMRSB MRCVS1* David Brodbelt MA VetMB PhD DVA DipECVAA MRCVS2 2 Holger Volk DVM PhD DipECVN FHEA MRCVS 1 University College London 2 Royal Veterinary College * Corresponding Author ([email protected]) ISSN: 2396-9776 Published: 11 Feb 2016 in: Vol1, Issue 1 DOI: http://dx.doi.org/10.18849/ve.v1i1.9 Next Review Date: 23 Nov 2017 KNOWLEDGE SUMMARY Clinical bottom line Oral phenobarbital and imepitoin in particular, followed by potassium bromide and levetiracetam are likely to be effective for the treatment of canine idiopathic epilepsy. There is strong evidence supporting the use of oral phenobarbital and imepitoin as ‘first line’ medications. However, there remains a lack of evidence for targeted treatment for the various individual epileptic phenotypes and quite limited evidence on direct comparisons of the efficacy between various anti-epileptic drugs. Question In dogs with epilepsy, what is the best treatment to reduce seizures. Clinical scenario A 5 years old 17 kg German Shepherd intact male dog manifested generalized tonic-clonic seizures one year ago. In the last two months the dog manifested five episodes. The dog is normal between the episodes; idiopathic epilepsy is suspected. You wonder what the best treatment in a dog with presumed idiopathic epilepsy would be. Summary of the evidence Law (2015) Population: Dogs with idiopathic epilepsy (Tier II). Sample size: 21 dogs, n=21 Intervention details: Dogs were fed either ketogenic medium-chain TAG diet (MCTD) or placebo diet for 3 months followed by a subsequent respective switch of diet for a further 3 months. -

WHO Drug Information Vol. 21, No. 3, 2007
WHO DRUG INFORMATION VOLUME 21 • NUMBER 3 • 2007 RECOMMENDED INN LIST 58 INTERNATIONAL NONPROPRIETARY NAMES FOR PHARMACEUTICAL SUBSTANCES WORLD HEALTH ORGANIZATION • GENEVA WHO Drug Information Vol 21, No. 3, 2007 World Health Organization WHO Drug Information Contents Pharmacovigilance Focus Current Topics Challenges of pharmacovigilance in Global strategy to prevent transmission Ukraine 193 of Chagas disease 211 Adverse reaction reporting in Canada 197 Educational modules for health professionals reporting adverse Consultation Documents reactions 197 International Pharmacopoeia WHO pharmacovigilance capacity Amodiaquine hydrochloride tablets 212 building 202 Chloroquine sulfate oral solution 214 Paediatric artemether and lumefantrine oral suspension 216 Safety and Efficacy Issues Sulfadoxine and pyrimethamine tablets 221 Rosiglitazone: cardiac safety 203 Quinine sulfate tablets 223 Rosiglitazone: cardiac safety profile 204 Rifampicin, isoniazid and ethambutol Bevacizumab: tracheoesophageal hydrochloride tablets 226 fistula 204 Rifampicin and isoniazid dispersible NSAIDS and cardiovascular risk 205 tablets 229 Rosiglitazone and parotid gland Rifampicin, isoniazid and pyrazinamide enlargement 206 dispersible tablets 232 Cinacalcet: indication changes 206 Efavirenz capsules 236 Omalizumab and anaphylaxis 207 Nevirapine oral solution 238 Vinca alkaloids: intravenous Nevirapine tablets 241 administration 207 Pioglitazone: fractures in women 207 Recent Publications, Regulatory Action and News Information and Events Viracept®: suspension pending -

Lääkealan Turvallisuus- Ja Kehittämiskeskuksen Päätös
Lääkealan turvallisuus- ja kehittämiskeskuksen päätös N:o xxxx lääkeluettelosta Annettu Helsingissä xx päivänä maaliskuuta 2016 ————— Lääkealan turvallisuus- ja kehittämiskeskus on 10 päivänä huhtikuuta 1987 annetun lääke- lain (395/1987) 83 §:n nojalla päättänyt vahvistaa seuraavan lääkeluettelon: 1 § Lääkeaineet ovat valmisteessa suolamuodossa Luettelon tarkoitus teknisen käsiteltävyyden vuoksi. Lääkeaine ja sen suolamuoto ovat biologisesti samanarvoisia. Tämä päätös sisältää luettelon Suomessa lääk- Liitteen 1 A aineet ovat lääkeaineanalogeja ja keellisessä käytössä olevista aineista ja rohdoksis- prohormoneja. Kaikki liitteen 1 A aineet rinnaste- ta. Lääkeluettelo laaditaan ottaen huomioon lää- taan aina vaikutuksen perusteella ainoastaan lää- kelain 3 ja 5 §:n säännökset. kemääräyksellä toimitettaviin lääkkeisiin. Lääkkeellä tarkoitetaan valmistetta tai ainetta, jonka tarkoituksena on sisäisesti tai ulkoisesti 2 § käytettynä parantaa, lievittää tai ehkäistä sairautta Lääkkeitä ovat tai sen oireita ihmisessä tai eläimessä. Lääkkeeksi 1) tämän päätöksen liitteessä 1 luetellut aineet, katsotaan myös sisäisesti tai ulkoisesti käytettävä niiden suolat ja esterit; aine tai aineiden yhdistelmä, jota voidaan käyttää 2) rikoslain 44 luvun 16 §:n 1 momentissa tar- ihmisen tai eläimen elintoimintojen palauttami- koitetuista dopingaineista annetussa valtioneuvos- seksi, korjaamiseksi tai muuttamiseksi farmako- ton asetuksessa kulloinkin luetellut dopingaineet; logisen, immunologisen tai metabolisen vaikutuk- ja sen avulla taikka terveydentilan -

7 Antiepileptic Therapy in Dogs
8/13/19 Disclosures è FINANCIAL DISCLOSURE: • Grant/Research Support – Purina, Boehringer Ingelheim, BBSRC, Wellcome Trust, AKC Canine Health Foundation Department of Small Animal Diseases • Consulting and Speaker Engagement – Purina, Boehringer Ingelheim. è UNLABELED/ UNAPPROVED USES DISCLOSURE: Antiepileptic Therapy in Dogs - Fundamentals • I will discuss results of clinical trials in which antiepileptic drugs were used which are either not licensed for the specie or are only licensed in certain countries. Please and Cases check local authorities before use. Prof. Holger A. Volk DipECVN, PhD, PGCAP, FHEA, MRCVS Head of Department, Tierärztliche Hochschule Hannover RCVS & EBVS® European Specialist in Veterinary Neurology Past-President of the European College of Veterinary Neurology Treasurer of the European Board of Veterinary Specialisation Honorary Senior Lecturer -UCL Institute of Neurology Honorary Professor of Veterinary Neurology and Neurosurgery -Royal Veterinary College Outcome in individual patients: impact on seizures How does success look like? Therapeutic success Outcome in individual patients: impact on seizures Thank you Marios Charalambous Evaluate short-term & long-term success. Term drug-resistant combined witH drug information. (e.g. PHB resistant) 1 8/13/19 International Veterinary Epilepsy Task Force 1. International Veterinary Epilepsy Task Force consensus report on epilepsy definition, classification and terminology in companion animals (chaired by Prof. Mette Berendt) 2. International Veterinary Epilepsy Task Force Consensus Proposal: Diagnostic approach to epilepsy in dogs (Chaired by Drs. Luisa De Risio and Sofie Bhatti) 3. International Veterinary Epilepsy Task Force current understanding of idiopathic epilepsy of genetic or suspected genetic origin in purebred dogs (Chaired by Dr. Velia-Isabel Hülsmeyer) 4. International Veterinary Epilepsy Task Force consensus proposal: Medical treatment of canine epilepsy in Europe (Chaired by Drs. -
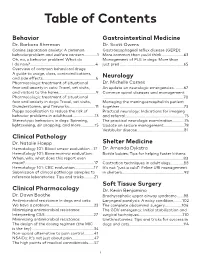
Table of Contents
Table of Contents Behavior Gastrointestinal Medicine Dr. Barbara Sherman Dr. Scott Owens Canine separation anxiety: A common Gastroesophageal reflux disease (GERD): behaviorproblem and welfare concern.............1 More common than you’d think .....................63 Oh, no, a behavior problem! What do Management of PLE in dogs: More than I do now?................................................................4 just pred ..............................................................65 Overview of common behavioral drugs: A guide to usage, class, contraindications, and side effects....................................................6 Neurology Pharmacologic treatment of situational Dr. Michelle Carnes fear and anxiety in cats: Travel, vet visits, An update on neurologic emergencies..........67 and visitors to the home.....................................9 Common spinal diseases and management Pharmacologic treatment of situational ...............................................................................70 fear and anxiety in dogs: Travel, vet visits, Managing the meningoencephalitis patient thunderstorms, and fireworks..........................11 together ..............................................................73 Puppy socialization to reduce the risk of Practical neurology: Indications for imaging behavior problems in adulthood......................13 and referral..........................................................75 Stereotypic behaviors in dogs: Spinning, The practical neurologic examination............76 lightseeking, -
Cambridge University Press 978-0-521-27971-0 — Common Epilepsy Pitfalls Dieter Schmidt , Steven Schachter Index More Information
Cambridge University Press 978-0-521-27971-0 — Common Epilepsy Pitfalls Dieter Schmidt , Steven Schachter Index More Information Index A AEDs newer, 113, 115, 128–9, AAN, 109, 118, 189, 197 adverse efects, 101, 113–14, 132–4, 137, 141–2, 146, abdominal pain, 168–9 132–4, 137, 144–6, 165, 148, 151–2 abnormal EEG, 98, 102–4, 168, 174, 177, 184–5, 187, nonenzyme-inducing, 153 179, 181 190, 195, 199–200, 202 noninducing, 132 abnormalities, 17, 18, 19, 27, carbonic anhydrase- noninteracting, 129 30, 35, 38, 45, 47, 51, inhibiting, 168 old, 104, 113, 115, 132–4, 57, 61, 62, 92, 102, 152, appropriate, 106, 159–60, 224 173, 211 169 average doses, 141 optimal, 111 neurological, 103, 105 baseline, 173 past, 145 pathological, 91, 163 classic, 109, 115, 128–9, plasma concentrations, absence seizures, 13, 59, 68, 132–3, 141 148–9 70–1, 80, 82, 89–90, 105, combinations, 144, 174 preferred, 109 110, 114, 116, 119, 122, comedication of, 130–1 restarting, 183, 186 158, 179 common doses, 140, 147 risk-beneit proile, 110 abuse, 14, 26, 56 compliance, 220, 226 second-generation, 111–12, accommodations, 235 concentration, 148 136 acetazolamide, 112, 120, 122, current, 99, 106, 134, 160, second-line, 117, 224 168, 193 198, 225 second, 143, 145, 173 acidosis, 119, 168, 221, 225 daily dose, 141–4, 195 side efects, 171 metabolic, 167–8 discontinuation of, 90, 117, single, 172 ACTH, 117, 121 133, 151–2, 160, 164, 168, starting, 97–8, 100, 104–5 activating procedures, 18 175, 178–81, 183–7, 206 stopping, 97, 172, 175–9, acupuncture, 154 dose increments, 140–2, 183–6 -

(Imepitoin) for Idiopathic Epilepsy?
Does your dog receive Pexion (Imepitoin) for idiopathic epilepsy? New RVC and AHT study investigates the effects of Pexion (Imepitoin) on the behaviour and welfare of dogs with idiopathic epilepsy Idiopathic epilepsy is the most common neurological disorder affecting dogs. A wide variety of diagnostic tests and medical treatment options are available and are well investigated; however, not much is known about the impact of epilepsy and the anti-epileptic drugs your dog receives on his or her behaviour and welfare. As such, we are carrying out a questionnaire study focussing on the impact of your dog’s epilepsy and its treatment on your dog’s day to day behaviour and welfare. We hope this information will further our understanding of epilepsy and the treatments vets prescribe for it, and aid vets in giving advice to owners such as yourself in the future. How can you get involved? We are interested in dogs that: 1. Have been diagnosed with idiopathic epilepsy, EITHER By a neurology specialist with the aid of blood examination and MRI OR By your regular vet due to recurrent seizures for more than one year, and the first seizure your dog had was when they were between 6 months and 6 years. AND 2. Are currently being treated with Imepitoin ('Pexion'), or this was the last anti-epileptic treatment reported (if your dog passed away whilst being treated for epilepsy) (N.B. This can be in combination with any other anti-epileptic drug e.g. Phenobarbital (e.g. 'Epiphen', 'Phenoleptil'), Potassium Bromide (e.g. 'Epilease', 'Libromide') etc.