Clinical Practice Guideline (Update): Earwax (Cerumen Impaction)
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-
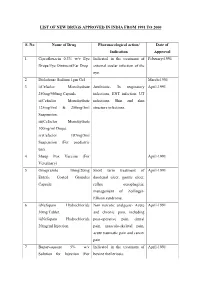
List of New Drugs Approved in India from 1991 to 2000
LIST OF NEW DRUGS APPROVED IN INDIA FROM 1991 TO 2000 S. No Name of Drug Pharmacological action/ Date of Indication Approval 1 Ciprofloxacin 0.3% w/v Eye Indicated in the treatment of February-1991 Drops/Eye Ointment/Ear Drop external ocular infection of the eye. 2 Diclofenac Sodium 1gm Gel March-1991 3 i)Cefaclor Monohydrate Antibiotic- In respiratory April-1991 250mg/500mg Capsule. infections, ENT infection, UT ii)Cefaclor Monohydrate infections, Skin and skin 125mg/5ml & 250mg/5ml structure infections. Suspension. iii)Cefaclor Monohydrate 100mg/ml Drops. iv)Cefaclor 187mg/5ml Suspension (For paediatric use). 4 Sheep Pox Vaccine (For April-1991 Veterinary) 5 Omeprazole 10mg/20mg Short term treatment of April-1991 Enteric Coated Granules duodenal ulcer, gastric ulcer, Capsule reflux oesophagitis, management of Zollinger- Ellison syndrome. 6 i)Nefopam Hydrochloride Non narcotic analgesic- Acute April-1991 30mg Tablet. and chronic pain, including ii)Nefopam Hydrochloride post-operative pain, dental 20mg/ml Injection. pain, musculo-skeletal pain, acute traumatic pain and cancer pain. 7 Buparvaquone 5% w/v Indicated in the treatment of April-1991 Solution for Injection (For bovine theileriosis. Veterinary) 8 i)Kitotifen Fumerate 1mg Anti asthmatic drug- Indicated May-1991 Tablet in prophylactic treatment of ii)Kitotifen Fumerate Syrup bronchial asthma, symptomatic iii)Ketotifen Fumerate Nasal improvement of allergic Drops conditions including rhinitis and conjunctivitis. 9 i)Pefloxacin Mesylate Antibacterial- In the treatment May-1991 Dihydrate 400mg Film Coated of severe infection in adults Tablet caused by sensitive ii)Pefloxacin Mesylate microorganism (gram -ve Dihydrate 400mg/5ml Injection pathogens and staphylococci). iii)Pefloxacin Mesylate Dihydrate 400mg I.V Bottles of 100ml/200ml 10 Ofloxacin 100mg/50ml & Indicated in RTI, UTI, May-1991 200mg/100ml vial Infusion gynaecological infection, skin/soft lesion infection. -
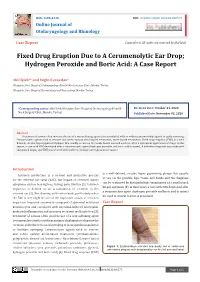
Fixed Drug Eruption Due to a Cerumenolytic Ear Drop; Hydrogen Peroxide and Boric Acid: a Case Report
ISSN: 2688-8238 DOI: 10.33552/OJOR.2020.04.000577 Online Journal of Otolaryngology and Rhinology Case Report Copyright © All rights are reserved by Akif İşlek Fixed Drug Eruption Due to A Cerumenolytic Ear Drop; Hydrogen Peroxide and Boric Acid: A Case Report Akif İşlek1* and Engin Karaaslan2 1Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey 2Nusaybin State Hospital, Dermatology and Venereology, Mardin, Turkey *Corresponding author: Received Date: October 24, 2020 Published Date: November 03, 2020 Akif İşlek, Nusaybin State Hospital, Otolaryngology-Head & Neck Surgery Clinic, Mardin, Turkey. Abstract Treatment of earwax often involves the use of a wax softening agent (cerumenolytic) with or without antimicrobial agents to easily removing. Cerumenolytic agents used to remove and soften earwax areoil-based treatments, water-based treatments. Fixed drug eruption (FDE) is a well- defined, circular, hyperpigmented plaque that usually occurs on the trunk, hands mucosal surfaces, after a systemical application of drugs. In this report, a case with FDE developed after a cerumenolytic agent (hydrogen peroxide and boric acid in water). A definitive diagnosis was made with skin punch biopsy and FDE was treated with oral levocetirizine and topical mometasone. Introduction is a well-defined, circular, hyper pigmenting plaque that usually Cerumen production is a normal and protective process occurs on the genitals, lips, trunk, and hands and the diagnosis for the external ear canal (EAC), but impact of cerumen causes can be confirmed by histopathologic examination of a small punch symptoms such as hearing loss, itching, pain, tinnitus [1]. Cerumen biopsy specimen [5]. In this report, a case with FDE developed after impaction is defined as an accumulation of cerumen in the a cerumenolytic agent (hydrogen peroxide and boric acid in water) external ear [2]. -

Assessment of Antimicrobial Activity of Cerumen (Earwax) and Antibiotics
Microbiology Research 2020; volume 11:8565 Assessment of antimicrobial nation of fatty acid). Another gland i.e. apoc- activity of cerumen (earwax) rine sweat glands release secretion that com- Correspondence: Iffat Naz, Department of bines with the sebum to form cerumen. It Biology, Scientific Unit, Deanship of and antibiotics against picks up discarded cells, ear follicles and Educational Services, Qassim University, pathogenic bacteria isolated may contain dust or other debris, but the Buraidah, 51452, Qassim, Kingdom of Saudi from ear pus samples resulting compound forms earwax or ceru- Arabia (KSA). men.6 Tel.: +966 533897891 E-mail: [email protected] ; There are two different types of geneti- [email protected] Iffat Naz cally determined earwax such as wet type Department of Biology, Scientific Unit, and dry type. The dry type is most common Key words: Ear pus samples; Pathogenic bac- Deanship of Educational Services, in Asians and Native Americans and has a teria; Antibiotics; Cerumen; Antibacterial Qassim University, Buraidah, Qassim, grey brownish colour while the wet type can potency. Kingdom of Saudi Arabia be found in Caucasians and Africians and has a brown or dark colour.7 About 30-50% of Acknowledgements: The author would like to South Asians, Central Asians and Pacific thanks Mr. Jamil & Miss. Javeria (M. Phil islanders have the dry type of cerumen. Scholars), for assisting in collection of ear pus Abstract Cerumen type has been used by anthropolo- samples from different hospitals of Peshawar, gist to track human migratory patterns, such KP, Pakistan. She is also grateful to Dr. Abdul The present study is focused on the Rehman for providing laboratory facilities, at as those of Eskimas.8 Further, the study of assessment of the antimicrobial activity of Department of Microbiology, Abasyn cerumen and antibiotics against bacteria earwax has shown controversy, as some University Peshawar, KP, Pakistan. -

Common Ear, Nose & Throat Problems
Common Ear, Nose & Throat Problems The information provided in this presentation is not intended to guide treatment or aid in making a diagnosis. Always consult a physician or nurse practitioner. Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Normal Larynx Normal larynx in a 44 yr old non-smoker Go to http://www.entusa.com/normal_larynx.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Acute Laryngitis This video shows the function of the larynx in a 24 yr old patient with acute laryngitis. Talking was painful and she only talked in a faint whisper. Go to http://www.entusa.com/laryngitis.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Vocal Cord Paralysis This video shows the function of a larynx with a paralyzed left true vocal cord. The patient has lung cancer. She has a poorly compensated breathy voice which is difficult to understand. This patient had a 55 pack year history of smoking. Go to http://www.entusa.com/vocal_cord_paralysis_2.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Vocal Cord Polyp This video shows the function of a larynx with a vocal cord polyp on the right true vocal cord. This patient smoked one pack a day for 30 years. Go to http://www.entusa.com/larynx_polyp-9.htm to View Video Copyright 2002, 2014, Kevin T. Kavanagh All Rights Reserved www.entusa.com Laryngeal Cancer This video shows the function of a larynx with a large T1b Cancer on both true vocal cords and anterior commissure in 72 yr old male with a 150 pack year history of smoking. -
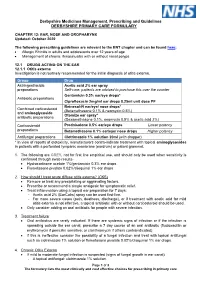
EAR, NOSE and OROPHARYNX Updated: October 2020
Derbyshire Medicines Management, Prescribing and Guidelines DERBYSHIRE PRIMARY CARE FORMULARY CHAPTER 12: EAR, NOSE AND OROPHARYNX Updated: October 2020 The following prescribing guidelines are relevant to the ENT chapter and can be found here: • Allergic Rhinitis in adults and adolescents over 12 years of age • Management of chronic rhinosinusitis with or without nasal polyps 12.1 DRUGS ACTING ON THE EAR 12.1.1 Otitis externa Investigation is not routinely recommended for the initial diagnosis of otitis externa. Group Drug Astringent/acidic Acetic acid 2% ear spray preparations Self-care: patients are advised to purchase this over the counter Gentamicin 0.3% ear/eye drops* Antibiotic preparations Ciprofloxacin 2mg/ml ear drops 0.25ml unit dose PF Betnesol-N ear/eye/ nose drops* Combined corticosteroid (Betamethasone 0.1% & neomycin 0.5%) and aminoglycoside Otomize ear spray* antibiotic preparations (Dexamethasone 0.1%, neomycin 0.5% & acetic acid 2%) Corticosteroid Prednisolone 0.5% ear/eye drops Lower potency preparations Betamethasone 0.1% ear/eye/ nose drops Higher potency Antifungal preparations Clotrimazole 1% solution 20ml (with dropper) * In view of reports of ototoxicity, manufacturers contra-indicate treatment with topical aminoglycosides in patients with a perforated tympanic membrane (eardrum) or patent grommet. 1. The following are GREY, not for first line empirical use, and should only be used when sensitivity is confirmed through swab results- • Hydrocortisone acetate 1%/gentamicin 0.3% ear drops • Flumetasone pivalate 0.02%/clioquinol 1% ear drops 2. How should I treat acute diffuse otitis externa? (CKS) • Remove or treat any precipitating or aggravating factors. • Prescribe or recommend a simple analgesic for symptomatic relief. -

10/15-Hour Medication Test Answers
Appendix 10/15-Hour Medication Test Answers Name _________________________________ Facility _________________________________ Part 1: Match the term or phrase on the right with the abbreviation or term on the left by placing the correct letter on the appropriate line. _____ 1. PRN (p) a. milligram _____ 2. ac (e) b. at bedtime _____ 3. stat (j) c. Medication Administration Record _____ 4. SL (k) d. over the counter _____ 5. MAR (c) e. before meals _____ 6. mg (a) f. tablespoonful _____ 7. pc (m) g. placed and affixed to the skin _____ 8. OTC (d) h. teaspoonful _____ 9. Subcutaneous (r) i. milliliter _____ 10. po (n) j. immediately _____ 11. qhs (b) k. sublingual _____ 12. tbsp (f) l. placed under the tongue _____ 13. transdermal (g) m. after meals _____ 14. ml (i) n. by mouth _____ 15. gm (o) o. gram _____ 16. QOD (q) p. as needed _____ 17. tsp (h) q. every other day _____ 18. sublingual (l) r. inject into the fat with a syringe Medication Administration – March 2021 10/15-Hour Training Course for Adult Care Homes 4 Appendix 10/15-Hour Medication Test Answers – Continued Part 2: Fill in the blank with the appropriate word or term. You may choose to use the word bank below. 19. A heart tablet taken by mouth and swallowed is an example of a medication taken by the oral route. 20. A medication that is inserted into the rectum is given using the rectal route. 21. A topical medication is applied directly to the skin surface. -

What Causes Swimmer's Ear?
Swimmer’s Ear Affecting the outer ear, swimmer’s ear is a painful condition resulting from inflammation, irritation, or infection. These symptoms often occur after water gets trapped in your ear, with subsequent spread of bacteria or fungal organisms. Because this condition commonly affects swimmers, it is known as swimmer’s ear. Swimmer’s ear (also called acute otitis externa) often affects children and teenagers, but can also affect those with eczema (a condition that causes the skin to itch), or excess earwax. Your doctor will prescribe treatment to reduce your pain and to treat the infection. What causes swimmer’s ear? A common source of the infection is increased moisture trapped in the ear canal, from baths, showers, swimming, or moist environments. When water is trapped in the ear canal, bacteria that normally inhabit the skin and ear canal multiply, causing infection of the ear canal. Swimmer’s ear needs to be treated to reduce pain and eliminate any effect it may have on your hearing, as well as to prevent the spread of infection. Other factors that may contribute to swimmer’s ear include: ● Contact with excessive bacteria that may be present in hot tubs or polluted water ● Excessive cleaning of the ear canal with cotton swabs ● Contact with certain chemicals such as hair spray or hair dye (Avoid this by placing cotton balls in your ears when using these products.) ● Damage to the skin of the ear canal following water irrigation to remove wax ● A cut in the skin of the ear canal ● Other skin conditions affecting the ear canal, such as eczema or seborrhea What are the signs and symptoms? The most common symptoms of swimmer’s ear are itching inside the ear and pain that gets worse when you tug on the auricle (outer ear). -

Supplementary Methods Earwax Sample Extraction a Clinical Research Assistant Was Specifically Trained in the Use of the Reiner-A
Supplementary Methods Earwax Sample Extraction A clinical research assistant was specifically trained in the use of the Reiner-Alexander syringe by one ear-nose-throat specialist doctor. Before cleaning both ears, the external auditory canal was examined using an otoscope to rule out the presence of any external ear pathology, such as impacted earwax or perforated eardrum. Briefly, the Reiner-Alexander syringe slowly injects water at 37°C inside the external ear canal. The process of syringing creates a sensation of mild pressure in the ear as the warm water from the syringe flushes the wax out. The expelled water and the extracted earwax secretion were collected in a kidney basin. During the follow-up visit, participants self-clean their right ears using the earwax self-sampling device, according to the manufacturer instructions (www.trears.com). The four labelled earwax samples were stored at 4 °C until they were analysed. Earwax Analysis using the Reiner-Alexander Syringe The extracted solution of water plus earwax secretion was stored in a 50 ml cryovial. Earwax samples were then resuspended with 500 µl Phosphate-Buffered Saline (PBS) to homogenise the sample. Then, 500 µl of diethyl ether was added to each sample and wobbled for one minute using a vortex. The resulting solution was stored at -20°C for 2 hours. Glucose levels were then analysed from the hydrophilic fraction. The earwax solution was dried using the displacement method of N2 at 25 degree Celsius. Following this, 125 µl of PPBS was added to resuspend each solution. The resulting solution containing earwax samples was stored at 4 degrees Celsius until analysed. -

A Functional ABCC11 Allele Is Essential in the Biochemical
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector See related commentary on pg 344 ORIGINAL ARTICLE A Functional ABCC11 Allele Is Essential in the Biochemical Formation of Human Axillary Odor Annette Martin1,3, Matthias Saathoff1,3, Fabian Kuhn2, Heiner Max1, Lara Terstegen1 and Andreas Natsch2 The characteristic human axillary odor is formed by bacterial action on odor precursors that originate from apocrine sweat glands. Caucasians and Africans possess a strong axillary odor ,whereas many Asians have only a faint acidic odor. In this study, we provide evidence that the gene ABCC11 (MRP8), which encodes an apical efflux pump, is crucial for the formation of the characteristic axillary odor and that a single-nucleotide polymorphism (SNP) 538G-A, which is prominent among Asian people, leads to a nearly complete loss of the typical odor components in axillary sweat. The secretion of amino-acid conjugates of human-specific odorants is abolished in homozygotic carriers of the SNP, and steroidal odorants and their putative precursors are significantly reduced. Moreover, we show that ABCC11 is expressed and localized in apocrine sweat glands. These data point to a key function of ABCC11 in the secretion of odorants and their precursors from apocrine sweat glands. SNP 538G-A, which also determines human earwax type, is present on an extended haplotype, which has reached 495% frequency in certain populations in recent human evolution. A strong positive selection in mate choice for low-odorant partners with a dysfunctional ABCC11 gene seems a plausible explanation for this striking frequency of a loss-of-function allele. -

Earwax Problems N
n Earwax Problems n Can earwax problems Earwax, also called cerumen, is a normal sub- stance that helps protect the ear canal. If too be prevented? much earwax builds up, it can block the ear canal, If your child has a lot of earwax build-up, using special causing ear discomfort, reduced hearing, and eardrops on a regular basis may help to prevent prob- other symptoms. Excessive earwax can usually lems. be removed by using special drops. If necessary, it can be done by a doctor. Don’t try to remove Follow the doctor’s instructions on removing earwax. wax from your child’s ear by inserting anything in Especially in babies, never insert cotton swabs or any- the ear, including cotton swabs. thing else in the ear to attempt to remove earwax. How are earwax problems treated? What kinds of problems are caused by earwax? Earwax removal kits are available at drugstores. Tilt your child’s head sideways and then place drops in the ear. Let The build-up of too much earwax can block the your the drops remain in the ear for several minutes; they will child’s ear canal. This is sometimes called “impaction.” help dissolve the wax. This procedure can be repeated for Removing the excessive earwax promptly relieves symp- a few days, if needed. If excessive earwax is still present, toms such as feeling “clogged-up,” reduced hearing, and call our office. discomfort or pain. Earwax can be removed by using ear- ’ drops available at the drugstore or, if necessary, in the In the doctor s office, earwax may be removed using spe- doctor’s office. -

Earwax, Clinical Practice Il Tappo Di Cerume: Pratica Clinica F
Volume 29 – Supplement 1 – Number 4 – August 2009 Otorhinolaryngologica Italica Official Journal of the Italian Society of Otorhinolaryngology - Head and Neck Surgery Organo Ufficiale della Società Italiana di Otorinolaringologia e Chirurgia Cervico-Facciale Editorial Board Italian Scientific Board © Copyright 2009 by Editor-in-Chief: F. Chiesa L. Bellussi, G. Danesi, C. Grandi, Società Italiana di Otorinolaringologia e President of S.I.O.: A. Rinaldi Ceroni A. Martini, L. Pignataro, F. Raso, Chirurgia Cervico-Facciale Former Presidents of S.I.O.: R. Speciale, I. Tasca Via Luigi Pigorini, 6/3 G. Borasi, E. Pirodda (†), 00162 Roma, Italy I. De Vincentiis, D. Felisati, L. Coppo, International Scientific Board G. Zaoli, P. Miani, G. Motta, J. Betka, P. Clement, A. De La Cruz, Publisher L. Marcucci, A. Ottaviani, G. Perfumo, M. Halmagyi, L.P. Kowalski, Pacini Editore SpA P. Puxeddu, I. Serafini, M. Maurizi, M. Pais Clemente, J. Shah, Via Gherardesca,1 G. Sperati, D. Passali, E. de Campora, H. Stammberger 56121 Ospedaletto (Pisa), Italy A. Sartoris, P. Laudadio, E. Mora, Tel. +39 050 313011 M. De Benedetto, S. Conticello, D. Casolino Treasurer Fax +39 050 313000 Former Editors-in-Chief: C. Miani [email protected] C. Calearo (†), E. de Campora, www.pacinimedicina.it A. Staffieri, M. Piemonte Editorial Office Editor-in-Chief: F. Chiesa Cited in Index Medicus/MEDLINE, Editorial Staff Divisione di Chirurgia Cervico-Facciale Science Citation Index Expanded, Scopus Editor-in-Chief: F. Chiesa Istituto Europeo di Oncologia Deputy Editor: C. Vicini Via Ripamonti, 435 Associate Editors: 20141 Milano, Italy C. Viti, F. Scasso Tel. +39 02 57489490 Editorial Coordinators: Fax +39 02 57489491 M.G. -

GENTAMICIN Eye/Ear Drops 0.3% W/V Gentamicin Sulphate Please
GENTAMICIN Eye/Ear Drops 0.3% w/v Gentamicin Sulphate Please read this leaflet carefully before you start using this medicine. Keep this leaflet. You may need to read it again. If you have further questions, please ask your doctor or pharmacist. This medicine has been prescribed for you personally and you should not pass it on to others. It may harm them, even if their symptoms are the same as yours. If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist. The medicine will be called Gentamicin in this leaflet. In this leaflet: 1. What Gentamicin is and what it is used for 2. Before you use Gentamicin 3. How to use Gentamicin 4. Possible side effects 5. How to store Gentamicin 6. Further information 1. WHAT GENTAMICIN IS AND WHAT IT IS USED FOR Gentamicin eye/ear Drops are a sterile, preserved, aqueous solution used as eye/ear drops. The active ingredient Gentamicin is an antibiotic used to kill bacteria which cause infection. It is used for the management of eye & ear infection. 2. BEFORE YOU USE GENTAMICIN Do not use if you are allergic to Gentamicin, any of the ingredients, or any other aminoglycoside antibiotics if you have a perforated ear drum if you suffer from myasthenia gravis and related conditions Before you use Gentamicin: Take special care with Gentamicin Avoid prolonged use The drops must not be used in the ear if the ear drum is damaged in any way.