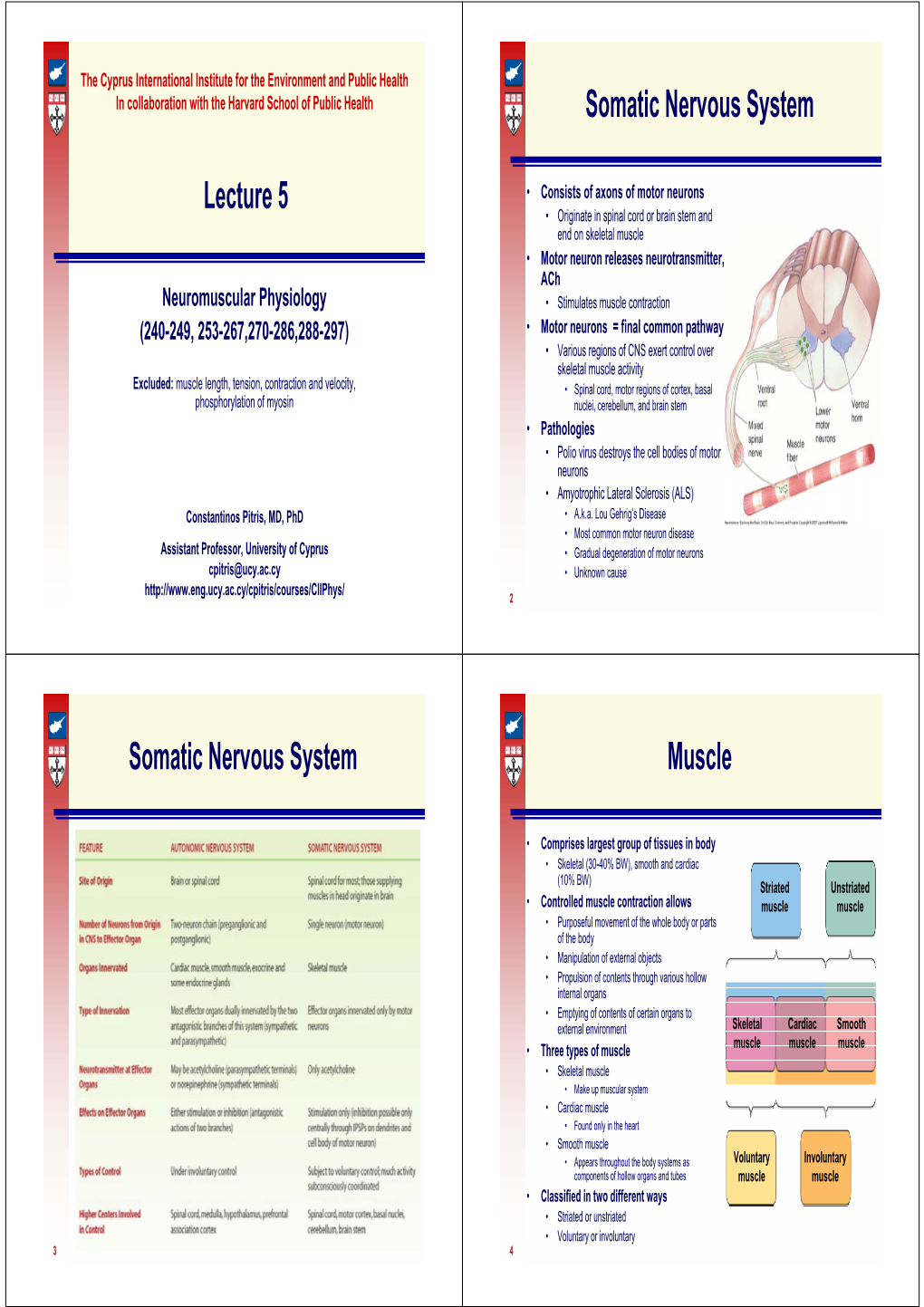
Somatic Nervous System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human Physiology/The Nervous System 1 Human Physiology/The Nervous System
Human Physiology/The Nervous System 1 Human Physiology/The Nervous System ← Integumentary System — Human Physiology — Senses → Homeostasis — Cells — Integumentary — Nervous — Senses — Muscular — Blood — Cardiovascular — Immune — Urinary — Respiratory — Gastrointestinal — Nutrition — Endocrine — Reproduction (male) — Reproduction (female) — Pregnancy — Genetics — Development — Answers The central nervous system includes the brain and spinal cord. The brain and spinal cord are protected by bony structures, membranes, and fluid. The brain is held in the cranial cavity of the skull and it consists of the cerebrum, cerebellum, and the brain stem. The nerves involved are cranial nerves and spinal nerves. Overview of the entire nervous system The nervous system has three main functions: sensory input, integration of data and motor output. Sensory input is when the body gathers information or data, by way of neurons, glia and synapses. The nervous system is composed of excitable nerve cells (neurons) and synapses that form between the neurons and connect them to centers throughout the body or to other neurons. These neurons operate on excitation or inhibition, and although nerve cells can vary in size and location, their communication with one another determines their function. These nerves conduct impulses from sensory receptors to the brain and spinal cord. The data is then processed by way of integration of data, which occurs only in the brain. After the brain has processed the information, impulses are then conducted from the brain and spinal cord to muscles and glands, which is called motor output. Glia cells are found within tissues and are not excitable but help with myelination, ionic regulation and extracellular fluid. The nervous system is comprised of two major parts, or subdivisions, the central nervous system (CNS) and the peripheral nervous system Nervous system (PNS). -
Nervous System and Eye Dissection
Nervous System and Eye Dissection Friday 14th th • Monday 10 • Finish notes • Take notes on Slides 4-10 • Write pre-reflection for dissection (write • Introduction to Nervous System separate paper) • Brain Metaphor Activity • Quiz Each other on notes • Dissection lab Safety • • th Study Word Parts and Eye Dissection Tuesday 11 Terms • Guest Speaker th • Wednesday 12 Staple following order to turn in Monday 17th • Take notes on slides 11-13 and Eye 1. Brain Metaphor Activity Dissection PowerPoint (Online) 2. Notes Neuron , CNS, PNS • Thursday 13th 3. Eye terms • Take notes on Slides 14-19 4. Senses – Mechanoreceptors and • Notes for lab on Monday Thermoreceptors • Mechanoreceptors and 5. Pre-Reflection (write separate paper) Thermoreceptors • Take the Quizizz’s once you have finished and reviewed the notes. https://join.quizizz.com • Chapter 5 and Nervous System Code: 284401 • Sheep Eye Dissection Code : 709952 • Nervous System Code: 73542 • Senses and Eyes Code: 831720 1. Draw neuron , label parts, and functions 2. Quiz Self of Nervous Cell and Functions 3. http://myclass.theinspiredinstructor.com/science/health_diagrams/ Neuron_Label.htm The Nervous System is divided into two parts: 1. Central NS a. Brain and spinal cord b. Processes info 2. Peripheral NS a. Mainly of nerves, sense organs b. Connect the CNS to every other part of the body c. Receives/sends info to and from the body 3. Nerves that transmit signals from the brain are called motor or efferent nerves 4. Nerves that transmit information from the body to the CNS are called sensory or afferent. Central Nervous System •Cerebrum •Frontal •Parietal •Occipital •Temporal •Cerebellum •Brain Stem Peripheral Nervous System Divided into three parts: 1. -

The Somatic Nervous System Mimi Jakoi, Phd Jennifer Carbrey, Phd
Introductory Human Physiology ©copyright Jennifer Carbrey & Emma Jakoi The Somatic Nervous System Mimi Jakoi, PhD Jennifer Carbrey, PhD The underlined headings correspond to the two Somatic Nervous system videos. 1. Introduction and structure The efferent portion of the peripheral nervous system consists of the somatic nervous system and the autonomic nervous system. The autonomic nervous system controls the function of glands, smooth muscle, cardiac muscle, and the neurons of the GI tract. It is composed of two neurons in series that can either excite or inhibit the target organ. In contrast, the somatic nervous system contains single neurons that excite skeletal muscles. The movements controlled by the somatic nervous system can be voluntary or involuntary (reflexes). Motor Unit The axons of motor neurons are myelinated and have large diameters for fast conduction of action potentials. As the axon approaches a skeletal muscle fiber (muscle cell) it usually branches to form synapses with anywhere from three to one thousand muscle fibers. However, each muscle fiber is usually innervated by only a single neuron. A motor unit consists of a neuron and all of the muscle fibers it innervates. A single neuron innervates fibers from only one muscle and the innervated muscle fibers are usually spread throughout the muscle. The portion of the skeletal muscle fiber plasma membrane that synapses with the motor neuron axon is called the motor end plate. Once an action potential arrives at the axon terminal, the depolarization of the membrane opens voltage-gated calcium channels (Fig. 1). An increase in intracellular calcium at the terminal causes release of acetylcholine vesicles into the neuromuscular junction. -

Nervous System Central Nervous System Peripheral Nervous System
Peripheral Nervous System Involuntary reflexes (spinal cord); Organization of Nervous System: voluntary actions (higher brain centers) Nervous system Integration Central nervous system Peripheral nervous system (CNS) (PNS) Motor Sensory output input Brain Spinal cord Motor division Sensory division (efferent) (afferent) Autonomic nervous system Somatic nervous system (involuntary; smooth & cardiac muscle) (voluntary; skeletal muscle) Sympathetic division Parasympathetic division Peripheral Nervous System Motor Units: Motor Unit: A single motor neuron and all the muscle fibers innervated by it (motor unit = all-or-none) Motor unit size dictates control: Fine Control / Rapid Reaction: 1-10 fibers / MU (e.g., ocular muscles) Gross Control / Slow Reaction: 1000’s fibers / MU (e.g., quadriceps) Recruitment: Addition of motor units to produce smooth, steady muscle tension (multiple fiber summation) Motoneuron Pool: Set of motor neurons innervating Small large motor units activated… muscle fibers within the same muscle • Varying thresholds Motor units overlap; provides coordination Marieb & Hoehn – Figure 9.13 1 Peripheral Nervous System Types of Motor Neurons: 1) Alpha () motor neurons: • Give rise to large Type A alpha (A) motor nerve fibers (~ 14 µm diameter) • Innervate extrafusal skeletal muscle fibers (generate force) 2) Gamma () motor neurons: • Give rise to small Type A gamma (Aγ) motor nerve fibers (~ 5 µm diameter) • Innervate intrafusal muscle fibers (small, specialized fibers – muscle spindle) What is the length of the muscle? Proper -

Commercialization of Hfac Electronic Nerve Block Technology to Treat Chronic Post Surgical Pain
COMMERCIALIZATION OF HFAC ELECTRONIC NERVE BLOCK TECHNOLOGY TO TREAT CHRONIC POST SURGICAL PAIN By ANIRUDHAN NARASIMHAN Submitted in partial fulfillment of the requirements For the degree of Master of Science Department of Biology CASE WESTERN RESERVE UNIVERSITY January 2011 CASE WESTERN RESERVE UNIVERSITY SCHOOL OF GRADUATE STUDIES We hereby approve the thesis/dissertation of Anirudhan Narasimhan _____________________________________________________ Master of Science candidate for the ______________________degree *. Roy E.Ritzmann (signed)_______________________________________________ (chair of the committee) Christopher A.Cullis ________________________________________________ Hillel J. Chiel ________________________________________________ Joseph Jankowski ________________________________________________ Zi-Ping Fang ________________________________________________ ________________________________________________ 08/14/2010 (date) _______________________ *We also certify that written approval has been obtained for any proprietary material contained therein. Dedicated to Revathy Narasimhan Table of Contents TABLE OF CONTENTS ............................................................................................................................ IV LIST OF TABLES .................................................................................................................................... VI LIST OF FIGURES ................................................................................................................................ -

NERVOUS SYSTEM ANATOMY M1 - Gross and Developmental Anatomy Dr
INTRODUCTION to NERVOUS SYSTEM ANATOMY M1 - Gross and Developmental Anatomy Dr. Milton M. Sholley Professor of Anatomy and Neurobiology and Dr. Michael H. Peters Professor of Chemical and Life Science Engineering Lecture/Syllabus Outline I. Major Divisions of the Nervous System II. Cranial Nerves (structure) III. Spinal Nerves (structure) IV. Autonomic Nervous System (functional) V. Functional Components of Spinal Nerves VI. Dermatomes 2 Important Definitions I. Major divisions of the nervous system include: A. Central nervous system (CNS)-an anatomical (i.e. structural) classification 1. Brain 2. Spinal cord B. Peripheral nervous system (PNS)-an anatomical (i.e. structural) classification 1. Cranial nerves-arise from the brain 2. Spinal nerves-arise from the spinal cord C. Somatic nervous system (SNS)-a functional classification. Parts of this system begin in the CNS and enter the PNS to supply the body wall (“soma”). D. Autonomic nervous system (ANS)-a functional classification. Parts of this system begin in the CNS and enter the PNS to supply the viscera. 1. Parasympathetic division 2. Sympathetic division Cranial Nerves (all twelve pairs shown) II. Cranial nerves A. Twelve pairs of cranial nerves arise from various parts of the brain and have both I numbers designated by Roman numerals and names. I IIII 1. Most of the cranial nerves will not be IV studied until you begin the Head and Neck V portion of the course, when they will be studied in detail. VI VII B. Cranial nerve XI, the spinal accessory VII nerve, has been introduced this week in regard I IX to the trapezius muscle, which is a muscle that X it innervates. -

The Nervous System Think About How Your Body Works
The nervous system Think about how your body works. Right now you are reading this page, but you are not telling your eyes to read the text; more importantly, you are not consciously reminding your heart to keep beating or your CHAPTER lungs to keep breathing. These are automatic processes that your body completes without conscious thought or instruction. But how does this 4 happen? Your body needs to coordinate communication between all of its organs, systems and muscles, and this is where your central and peripheral nervous systems are involved. When studying the roles of the central and peripheral nervous systems as communication structures between the internal and external worlds, it is easy to consider them separate entities with individual responsibilities. However, this is not how the human nervous system operates in reality. The peripheral nerves connect all of the parts of the body with the central nervous system. OBJECTIVES → Recognise the basic structure and function of the human nervous system, including the central (i.e. brain and spinal cord) and peripheral (i.e. somatic and autonomic) nervous systems → Construct a diagram of a neuron, including the axon, dendrites, the cell body and synapses → Distinguish between sensory, motor and interneurons Source: Psychology 2019 v1.3 General Senior Syllabus © Queensland Curriculum & Assessment Authority SAMPLE FIGURE 1 Digital rendering showing the brain and spinal cord (components of the central nervous system) 86 PSYCHOLOGY FOR QUEENSLAND UNITS 1 & 2 OXFORD UNIVERSITY PRESS 04_BUR_PSYCH_SB12_13296_TXT_SI.indd 86 7/12/18 11:01 am SAMPLE OXFORD UNIVERSITY PRESS CHAPTER 4 THE NERVOUS SYSTEM 87 04_BUR_PSYCH_SB12_13296_TXT_SI.indd 87 18/9/18 3:04 pm The nervous system 4.1 KEY IDEAS In this section, you will learn about: ✚ the basic structure of the human nervous system ✚ the central and peripheral nervous systems ✚ the somatic and autonomic nervous systems. -

The Basic Functions of the Nervous System
The Nervous System The Basic Functions of the Nervous System • Sensation – The ability of the nerves to detect stimuli, such as pressure, temperature changes, taste, smell or light, and send a message in the form of impulses to the brain and spinal cord. The Basic Functions of the Nervous System • Movement -The ability of the brain to send impulses to muscles to cause movement, or a change in position. The Basic Functions of the Nervous System • Coordination -The nervous system controls and coordinates functions throughout the body and responds to internal and external stimuli. The Two Divisions of the Nervous System 1. The Central Nervous System: is divided into two parts: the brain and the spinal cord. 2. The Peripheral Nervous System: is divided into two major parts: the somatic nervous system and the autonomic nervous system. The Divisions of the Nervous System The Central Nervous System: The Brain • The brain contains approximately 100 billion neurons. The brain weighs about 3 pounds. About 20% of blood leaving the heart circulates through the brain. • The brain is responsible for analyzing information, processing information and relaying messages to the rest of the body. It is the main control center of the body. • Along with the spinal cord, it forms the body’s Central Nervous System or CNS. The Central Nervous System: The Spinal Cord • Along with the brain, it is part of the Central Nervous System. • It is the major communication link between the brain and the rest of the body. • It can process many reflexes – unconscious, automatic responses to stimuli. • There are 31 pairs of spinal nerves which branch from the spinal cord to control such processes as breathing, arm movement, and leg movement. -

CNS and Anesthesia
CNS and Anesthesia Lyon Lee DVM PhD DACVA The Nervous System • Central (CNS) and Peripheral (PNS) Central nervous system (CNS) • Nerves and associated structures within the brain and spinal cord Brain • Cerebrum • Brain stem Spinal cord • Gray matter White matter • Meninges; dura mater, arachnoidea, pia mater • Epidural space • Subarachnoid space(intrathecal space) Figure 1. Anatomy of spinal cord 1 CSF • Formed at choroid plexuses in the ventricles • Cushioning effect • Normal: 10 mmHg in pressure, 1.002 – 1.009 in SG, 7.32 in pH • Increased production, decreased absorption, and/or obstruction of flow of CSF all contribute to hydrocephalus symptom Peripheral nervous system (PNS) • The nerves and ganglia which lie outside the brain and spinal cord. • Cranial nerves and spinal nerves extend from the CNS to peripheral organs such as muscles, joints and glands. • Nerves are bundles of nerve fibers, much like muscles are bundles of muscle fibers. Ganglia are collections, or small knots, of nerve cell bodies outside the CNS. • The peripheral nervous system is further subdivided into an afferent (sensory) division and an efferent (motor) division (see figure 2) • The efferent or motor division is again subdivided into the somatic nervous system and the autonomic nervous system. • Figure 3. Division of the nervous system CNS PNS Sensory division Motor division Autonomic Somatic nervous system nervous system Sympathetic Parasympathetic 2 Cranial nerves Table 1. Cranial nerves and their function Nerves in order Modality Function Olfactory (I) -

Autonomic Vs. Somatic Nervous System
Objectives z Know ANS divisionsand organization z Functional units z Principal neurotransmitters z Receptor types z Identify sensory input to ANS z Explain how it integrates function (BP) z List main physiological responses under ANS control z Distinguish SNS from PSNS mediatedresponses z Understand the consequences of ANS dysregulation Autonomic vs. Somatic Nervous System • AUTONOMIC Effectors: cardiac & smooth muscle, viscera & glands Efferent: 2‐neuron chain Neurotransmitter (NT) effects Stimulatory or inhibitory dependent on NT & receptor type SOMATIC Effectors: skeletal muscles Efferent: Heavily myelinated axons from CNS to muscle Neurotransmitter Effects: Acetylcholine excitatory effect in nicotinic (N1) receptors 1 z Autonomic Nervous System z Efferent motor neurons: innervate viscera & involuntary muscle z Afferent sensory neurons respond to: z Stretch (heart, arteries) z Glucose, PCO2, PO2 (blood) z Osmolarity & pH (blood & intestinal content) z Temperature (skin & internal organs) SNS & PSNS Functional unit 2 neuron pathway 2 Sympathetic z Preganglionic: z Preganglionic Cholinergic neuron; neurons Nicoti n ic recept(Ntor (N2) z Thoracolumbar spinal z Postganglionic: cord: T1-L3 Adrenergic neuron; z Postganglionic Adrenergic receptor neurons z α 1: vasculature z Paravertebral or z α 2: presynaptic prevertebral ganglia z β 1: heart, adipose z Distant to target organ z β 2 : bronchioles, vasculature z β 3: adipose- thermogenic Parasympathetic z Preganglionic z Preganglionic: Cholinergic neurons neuron; Nicotinic (N2) receptor -
The Brain, Cranial Nerves, and Sensory and Motor Pathways
13 The Brain, Cranial Nerves, and Sensory and Motor Pathways Lecture Presentation by Lori Garrett © 2018 Pearson Education, Inc. Note to the Instructor: For the third edition of Visual Anatomy & Physiology, we have updated our PowerPoints to fully integrate text and art. The pedagogy now more closely matches that of the textbook. The goal of this revised formatting is to help your students learn from the art more effectively. However, you will notice that the labels on the embedded PowerPoint art are not editable. You can easily import editable art by doing the following: Copying slides from one slide set into another You can easily copy the Label Edit art into the Lecture Presentations by using either the PowerPoint Slide Finder dialog box or Slide Sorter view. Using the Slide Finder dialog box allows you to explicitly retain the source formatting of the slides you insert. Using the Slide Finder dialog box in PowerPoint: 1. Open the original slide set in PowerPoint. 2. On the Slides tab in Normal view, click the slide thumbnail that you want the copied slides to follow. 3. On the toolbar at the top of the window, click the drop down arrow on the New Slide tab. Select Reuse Slides. 4. Click Browse to look for the file; in the Browse dialog box, select the file, and then click Open. 5. If you want the new slides to keep their current formatting, in the Slide Finder dialog box, select the Keep source formatting checkbox. When this checkbox is cleared, the copied slides assume the formatting of the slide they are inserted after. -

Nervous System Organization of Nervous System
Nervous system Organization of nervous system Brain Central nervous system Spinal cord Special senses Sensory division Somatic Somatic /Voluntary Nervous system General senses nervous system Motor division Visceral Peripheral nervous Sensory division system Autonomic nervous Sympathetic system Motor division Enteric nervous Parasympathetic system Nervous system • The system which regulate the body responses to internal and external stimuli • Nervous system has two divisions ❑ Central Nervous System • Present in the midline performs the integratory role • It has anatomic components • Brain: Part of the CNS contained in skull and made up of over 100 billion neurons • Spinal Cord: Part of CNS contained in vertebral column, made up of about 100 million neurons Peripheral Nervous system • All nervous tissue outside CNS is called PNS • It is made up of nerves, ganglia, enteric plexus and sensory receptors • It has three divisions: • Somatic nervous system • Autonomic nervous system • Enteric nervous system Histology of nervous system Nervous tissue comprises two types of cell: • Neurons • Neuroglia . • Combine in different ways in the brain, spinal cord and periphery to generate different functions Neurons / Nerve cells • Structural and functional unit of nervous system • Structurally neuron has two parts: • The cell body • The neuronal processes • The cell body is the control center of neuron and is responsible for receiving, integrating, and sending nerve impulses • The cell body is enclosed by a plasma membrane and contains cytoplasm surrounding a nucleus with its nucleolus • The cytoplasm of the cell body is called perikaryon • Cell bodies also contain free ribosomes and prominent clusters of rough endoplasmic reticulum, termed Nissl bodies • The cytoskeleton includes both microtubules and neurofibrils.