Upregulated Connexin 43 Induced by Loss-Of-Functional S284L-Mutant 4
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
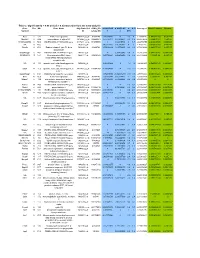
Table 2. Significant
Table 2. Significant (Q < 0.05 and |d | > 0.5) transcripts from the meta-analysis Gene Chr Mb Gene Name Affy ProbeSet cDNA_IDs d HAP/LAP d HAP/LAP d d IS Average d Ztest P values Q-value Symbol ID (study #5) 1 2 STS B2m 2 122 beta-2 microglobulin 1452428_a_at AI848245 1.75334941 4 3.2 4 3.2316485 1.07398E-09 5.69E-08 Man2b1 8 84.4 mannosidase 2, alpha B1 1416340_a_at H4049B01 3.75722111 3.87309653 2.1 1.6 2.84852656 5.32443E-07 1.58E-05 1110032A03Rik 9 50.9 RIKEN cDNA 1110032A03 gene 1417211_a_at H4035E05 4 1.66015788 4 1.7 2.82772795 2.94266E-05 0.000527 NA 9 48.5 --- 1456111_at 3.43701477 1.85785922 4 2 2.8237185 9.97969E-08 3.48E-06 Scn4b 9 45.3 Sodium channel, type IV, beta 1434008_at AI844796 3.79536664 1.63774235 3.3 2.3 2.75319499 1.48057E-08 6.21E-07 polypeptide Gadd45gip1 8 84.1 RIKEN cDNA 2310040G17 gene 1417619_at 4 3.38875643 1.4 2 2.69163229 8.84279E-06 0.0001904 BC056474 15 12.1 Mus musculus cDNA clone 1424117_at H3030A06 3.95752801 2.42838452 1.9 2.2 2.62132809 1.3344E-08 5.66E-07 MGC:67360 IMAGE:6823629, complete cds NA 4 153 guanine nucleotide binding protein, 1454696_at -3.46081884 -4 -1.3 -1.6 -2.6026947 8.58458E-05 0.0012617 beta 1 Gnb1 4 153 guanine nucleotide binding protein, 1417432_a_at H3094D02 -3.13334396 -4 -1.6 -1.7 -2.5946297 1.04542E-05 0.0002202 beta 1 Gadd45gip1 8 84.1 RAD23a homolog (S. -

Potassium Channels in Epilepsy
Downloaded from http://perspectivesinmedicine.cshlp.org/ on September 28, 2021 - Published by Cold Spring Harbor Laboratory Press Potassium Channels in Epilepsy Ru¨diger Ko¨hling and Jakob Wolfart Oscar Langendorff Institute of Physiology, University of Rostock, Rostock 18057, Germany Correspondence: [email protected] This review attempts to give a concise and up-to-date overview on the role of potassium channels in epilepsies. Their role can be defined from a genetic perspective, focusing on variants and de novo mutations identified in genetic studies or animal models with targeted, specific mutations in genes coding for a member of the large potassium channel family. In these genetic studies, a demonstrated functional link to hyperexcitability often remains elusive. However, their role can also be defined from a functional perspective, based on dy- namic, aggravating, or adaptive transcriptional and posttranslational alterations. In these cases, it often remains elusive whether the alteration is causal or merely incidental. With 80 potassium channel types, of which 10% are known to be associated with epilepsies (in humans) or a seizure phenotype (in animals), if genetically mutated, a comprehensive review is a challenging endeavor. This goal may seem all the more ambitious once the data on posttranslational alterations, found both in human tissue from epilepsy patients and in chronic or acute animal models, are included. We therefore summarize the literature, and expand only on key findings, particularly regarding functional alterations found in patient brain tissue and chronic animal models. INTRODUCTION TO POTASSIUM evolutionary appearance of voltage-gated so- CHANNELS dium (Nav)andcalcium (Cav)channels, Kchan- nels are further diversified in relation to their otassium (K) channels are related to epilepsy newer function, namely, keeping neuronal exci- Psyndromes on many different levels, ranging tation within limits (Anderson and Greenberg from direct control of neuronal excitability and 2001; Hille 2001). -

Transcriptomic Analysis of Native Versus Cultured Human and Mouse Dorsal Root Ganglia Focused on Pharmacological Targets Short
bioRxiv preprint doi: https://doi.org/10.1101/766865; this version posted September 12, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Transcriptomic analysis of native versus cultured human and mouse dorsal root ganglia focused on pharmacological targets Short title: Comparative transcriptomics of acutely dissected versus cultured DRGs Andi Wangzhou1, Lisa A. McIlvried2, Candler Paige1, Paulino Barragan-Iglesias1, Carolyn A. Guzman1, Gregory Dussor1, Pradipta R. Ray1,#, Robert W. Gereau IV2, # and Theodore J. Price1, # 1The University of Texas at Dallas, School of Behavioral and Brain Sciences and Center for Advanced Pain Studies, 800 W Campbell Rd. Richardson, TX, 75080, USA 2Washington University Pain Center and Department of Anesthesiology, Washington University School of Medicine # corresponding authors [email protected], [email protected] and [email protected] Funding: NIH grants T32DA007261 (LM); NS065926 and NS102161 (TJP); NS106953 and NS042595 (RWG). The authors declare no conflicts of interest Author Contributions Conceived of the Project: PRR, RWG IV and TJP Performed Experiments: AW, LAM, CP, PB-I Supervised Experiments: GD, RWG IV, TJP Analyzed Data: AW, LAM, CP, CAG, PRR Supervised Bioinformatics Analysis: PRR Drew Figures: AW, PRR Wrote and Edited Manuscript: AW, LAM, CP, GD, PRR, RWG IV, TJP All authors approved the final version of the manuscript. 1 bioRxiv preprint doi: https://doi.org/10.1101/766865; this version posted September 12, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -
![(253), Re15. [DOI: 10.1126/Stke.2532004Re15] 2004](https://docslib.b-cdn.net/cover/9453/253-re15-doi-10-1126-stke-2532004re15-2004-749453.webp)
(253), Re15. [DOI: 10.1126/Stke.2532004Re15] 2004
The VGL-Chanome: A Protein Superfamily Specialized for Electrical Signaling and Ionic Homeostasis Frank H. Yu and William A. Catterall (5 October 2004) Sci. STKE 2004 (253), re15. [DOI: 10.1126/stke.2532004re15] The following resources related to this article are available online at http://stke.sciencemag.org. This information is current as of 7 July 2009. Article Tools Visit the online version of this article to access the personalization and article tools: http://stke.sciencemag.org/cgi/content/full/sigtrans;2004/253/re15 Supplemental "Supplementary Table 1" Materials http://stke.sciencemag.org/cgi/content/full/sigtrans;2004/253/re15/DC1 Related Content The editors suggest related resources on Science's sites: http://stke.sciencemag.org/cgi/content/abstract/sigtrans;2006/360/tw376 http://stke.sciencemag.org/cgi/content/abstract/sigtrans;2006/350/pe33 http://stke.sciencemag.org/cgi/content/abstract/sigtrans;2006/333/tw149 http://stke.sciencemag.org/cgi/content/abstract/sigtrans;2005/307/pe50 http://stke.sciencemag.org/cgi/content/abstract/sigtrans;2005/302/pe46 Downloaded from http://stke.sciencemag.org/cgi/content/abstract/sigtrans;2005/270/tw55 http://stke.sciencemag.org/cgi/content/abstract/sigtrans;2004/233/pe22 http://stke.sciencemag.org/cgi/content/abstract/sigtrans;2004/233/pe23 http://stke.sciencemag.org/cgi/content/abstract/sigtrans;2004/227/pe16 http://stke.sciencemag.org/cgi/content/abstract/sigtrans;2004/219/re4 http://stke.sciencemag.org/cgi/content/abstract/sigtrans;2003/194/pe32 http://stke.sciencemag.org/cgi/content/abstract/sigtrans;2003/188/re10 -

Ion Channels
UC Davis UC Davis Previously Published Works Title THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Ion channels. Permalink https://escholarship.org/uc/item/1442g5hg Journal British journal of pharmacology, 176 Suppl 1(S1) ISSN 0007-1188 Authors Alexander, Stephen PH Mathie, Alistair Peters, John A et al. Publication Date 2019-12-01 DOI 10.1111/bph.14749 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2019/20: Ion channels. British Journal of Pharmacology (2019) 176, S142–S228 THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Ion channels Stephen PH Alexander1 , Alistair Mathie2 ,JohnAPeters3 , Emma L Veale2 , Jörg Striessnig4 , Eamonn Kelly5, Jane F Armstrong6 , Elena Faccenda6 ,SimonDHarding6 ,AdamJPawson6 , Joanna L Sharman6 , Christopher Southan6 , Jamie A Davies6 and CGTP Collaborators 1School of Life Sciences, University of Nottingham Medical School, Nottingham, NG7 2UH, UK 2Medway School of Pharmacy, The Universities of Greenwich and Kent at Medway, Anson Building, Central Avenue, Chatham Maritime, Chatham, Kent, ME4 4TB, UK 3Neuroscience Division, Medical Education Institute, Ninewells Hospital and Medical School, University of Dundee, Dundee, DD1 9SY, UK 4Pharmacology and Toxicology, Institute of Pharmacy, University of Innsbruck, A-6020 Innsbruck, Austria 5School of Physiology, Pharmacology and Neuroscience, University of Bristol, Bristol, BS8 1TD, UK 6Centre for Discovery Brain Science, University of Edinburgh, Edinburgh, EH8 9XD, UK Abstract The Concise Guide to PHARMACOLOGY 2019/20 is the fourth in this series of biennial publications. The Concise Guide provides concise overviews of the key properties of nearly 1800 human drug targets with an emphasis on selective pharmacology (where available), plus links to the open access knowledgebase source of drug targets and their ligands (www.guidetopharmacology.org), which provides more detailed views of target and ligand properties. -
Identification of Key Pathways and Genes in Dementia Via Integrated Bioinformatics Analysis
bioRxiv preprint doi: https://doi.org/10.1101/2021.04.18.440371; this version posted July 19, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Identification of Key Pathways and Genes in Dementia via Integrated Bioinformatics Analysis Basavaraj Vastrad1, Chanabasayya Vastrad*2 1. Department of Biochemistry, Basaveshwar College of Pharmacy, Gadag, Karnataka 582103, India. 2. Biostatistics and Bioinformatics, Chanabasava Nilaya, Bharthinagar, Dharwad 580001, Karnataka, India. * Chanabasayya Vastrad [email protected] Ph: +919480073398 Chanabasava Nilaya, Bharthinagar, Dharwad 580001 , Karanataka, India bioRxiv preprint doi: https://doi.org/10.1101/2021.04.18.440371; this version posted July 19, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract To provide a better understanding of dementia at the molecular level, this study aimed to identify the genes and key pathways associated with dementia by using integrated bioinformatics analysis. Based on the expression profiling by high throughput sequencing dataset GSE153960 derived from the Gene Expression Omnibus (GEO), the differentially expressed genes (DEGs) between patients with dementia and healthy controls were identified. With DEGs, we performed a series of functional enrichment analyses. Then, a protein–protein interaction (PPI) network, modules, miRNA-hub gene regulatory network and TF-hub gene regulatory network was constructed, analyzed and visualized, with which the hub genes miRNAs and TFs nodes were screened out. Finally, validation of hub genes was performed by using receiver operating characteristic curve (ROC) analysis. -

Therapeutic Approaches to Genetic Ion Channelopathies and Perspectives in Drug Discovery
fphar-07-00121 May 7, 2016 Time: 11:45 # 1 REVIEW published: 10 May 2016 doi: 10.3389/fphar.2016.00121 Therapeutic Approaches to Genetic Ion Channelopathies and Perspectives in Drug Discovery Paola Imbrici1*, Antonella Liantonio1, Giulia M. Camerino1, Michela De Bellis1, Claudia Camerino2, Antonietta Mele1, Arcangela Giustino3, Sabata Pierno1, Annamaria De Luca1, Domenico Tricarico1, Jean-Francois Desaphy3 and Diana Conte1 1 Department of Pharmacy – Drug Sciences, University of Bari “Aldo Moro”, Bari, Italy, 2 Department of Basic Medical Sciences, Neurosciences and Sense Organs, University of Bari “Aldo Moro”, Bari, Italy, 3 Department of Biomedical Sciences and Human Oncology, University of Bari “Aldo Moro”, Bari, Italy In the human genome more than 400 genes encode ion channels, which are transmembrane proteins mediating ion fluxes across membranes. Being expressed in all cell types, they are involved in almost all physiological processes, including sense perception, neurotransmission, muscle contraction, secretion, immune response, cell proliferation, and differentiation. Due to the widespread tissue distribution of ion channels and their physiological functions, mutations in genes encoding ion channel subunits, or their interacting proteins, are responsible for inherited ion channelopathies. These diseases can range from common to very rare disorders and their severity can be mild, Edited by: disabling, or life-threatening. In spite of this, ion channels are the primary target of only Maria Cristina D’Adamo, University of Perugia, Italy about 5% of the marketed drugs suggesting their potential in drug discovery. The current Reviewed by: review summarizes the therapeutic management of the principal ion channelopathies Mirko Baruscotti, of central and peripheral nervous system, heart, kidney, bone, skeletal muscle and University of Milano, Italy Adrien Moreau, pancreas, resulting from mutations in calcium, sodium, potassium, and chloride ion Institut Neuromyogene – École channels. -
Relevance of Electrolytic Balance in Channelopathies
SCUOLA DI DOTTORATO UNIVERSITÀ DEGLI STUDI DI MILANO-BICOCCA University of Milano-Bicocca School of Medicine and Surgery PhD Program in Translational and Molecular Medicine XXIX PhD course Relevance of electrolytic balance in channelopathies. Dr. Anna BINDA Matr. 708721 Tutor: Dr.ssa Ilaria RIVOLTA Coordinator: prof. Andrea BIONDI Academic year 2015-2016 2 Table of contents Chapter 1: introduction Channelopathies…………………………..…………………….….p. 7 Skeletal muscle channelopathies………………………….….…...p. 10 Neuromuscular junction channelopathies………………….……..p. 16 Neurological channelopathies……………………………….……p. 17 Cardiac channelopathies………………………………………..…p. 26 Channelopathies of non-excitable tissue………………………….p. 35 Scope of the thesis…………………………………………..…….p. 44 References………………………………………………….……..p. 45 Chapter 2: SCN4A mutation as modifying factor of Myotonic Dystrophy Type 2 phenotype…………………………..………..p. 51 Chapter 3: Functional characterization of a novel KCNJ2 mutation identified in an Autistic proband.…………………....p. 79 Chapter 4: A Novel Copy Number Variant of GSTM3 in Patients with Brugada Syndrome……………………………...………..p. 105 Chapter 5: Functional characterization of a mutation in KCNT1 gene related to non-familial Brugada Syndrome…………….p. 143 Chapter 6: summary, conclusions and future perspectives….p.175 3 4 Chapter 1: introduction 5 6 Channelopathies. The term “electrolyte” defines every substance that dissociates into ions in an aqueous solution and acquires the capacity to conduct electricity. Electrolytes have a central role in cellular physiology, in particular their correct balance between the intracellular compartment and the extracellular environment regulates physiological functions of both excitable and non-excitable cells, acting on cellular excitability, muscle contraction, neurotransmission and hormone release, signal transduction, ion and water homeostasis [1]. The most important electrolytes in the human organism are sodium, potassium, magnesium, phosphate, calcium and chloride. -

1 1 2 3 Cell Type-Specific Transcriptomics of Hypothalamic
1 2 3 4 Cell type-specific transcriptomics of hypothalamic energy-sensing neuron responses to 5 weight-loss 6 7 Fredrick E. Henry1,†, Ken Sugino1,†, Adam Tozer2, Tiago Branco2, Scott M. Sternson1,* 8 9 1Janelia Research Campus, Howard Hughes Medical Institute, 19700 Helix Drive, Ashburn, VA 10 20147, USA. 11 2Division of Neurobiology, Medical Research Council Laboratory of Molecular Biology, 12 Cambridge CB2 0QH, UK 13 14 †Co-first author 15 *Correspondence to: [email protected] 16 Phone: 571-209-4103 17 18 Authors have no competing interests 19 1 20 Abstract 21 Molecular and cellular processes in neurons are critical for sensing and responding to energy 22 deficit states, such as during weight-loss. AGRP neurons are a key hypothalamic population 23 that is activated during energy deficit and increases appetite and weight-gain. Cell type-specific 24 transcriptomics can be used to identify pathways that counteract weight-loss, and here we 25 report high-quality gene expression profiles of AGRP neurons from well-fed and food-deprived 26 young adult mice. For comparison, we also analyzed POMC neurons, an intermingled 27 population that suppresses appetite and body weight. We find that AGRP neurons are 28 considerably more sensitive to energy deficit than POMC neurons. Furthermore, we identify cell 29 type-specific pathways involving endoplasmic reticulum-stress, circadian signaling, ion 30 channels, neuropeptides, and receptors. Combined with methods to validate and manipulate 31 these pathways, this resource greatly expands molecular insight into neuronal regulation of 32 body weight, and may be useful for devising therapeutic strategies for obesity and eating 33 disorders. -

Novel Voltage Dependent Ion Channel Fusions and Method of Use Thereof
(19) TZZ¥ZZ _T (11) EP 3 056 902 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 17.08.2016 Bulletin 2016/33 G01N 33/542 (2006.01) C07K 14/705 (2006.01) (21) Application number: 15155202.3 (22) Date of filing: 16.02.2015 (84) Designated Contracting States: (72) Inventors: AL AT BE BG CH CY CZ DE DK EE ES FI FR GB • Ruigrok, Hermanus GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO 33200 Bordeaux (FR) PL PT RO RS SE SI SK SM TR • Percherancier, Yann Designated Extension States: 33140 Villenave d’Ornon (FR) BA ME •Veyret,Bernard 33600 PESSAC (FR) (71) Applicants: • UNIVERSITE DE BORDEAUX (74) Representative: Lecca, Patricia S. 33000 Bordeaux (FR) Cabinet Lecca • CENTRE NATIONAL DE LA RECHERCHE 21, rue de Fécamp SCIENTIFIQUE 75012 Paris (FR) 75794 Paris Cedex 16 (FR) • Institut Polytechnique de Bordeaux 33402 Talence Cedex (FR) (54) Novel voltage dependent ion channel fusions and method of use thereof (57) The present invention relates to novel volt- izing candidate molecules or physical parameters for age-dependent ion channel fusion subunits, and to a their ability to activate or inhibit voltage-dependent ion functional bioluminescence resonance energy transfer channels. (BRET) assay for screening in real time and character- EP 3 056 902 A1 Printed by Jouve, 75001 PARIS (FR) EP 3 056 902 A1 Description FIELD OF THE INVENTION 5 [0001] The present invention relates to novel voltage-dependent ion channel fusion subunits, and to a functional bioluminescence resonance energy transfer (BRET) assay for screening in real time and characterizing candidate mol- ecules or physical parameters for their ability to activate or inhibit voltage-dependent ion channels. -

Genetic Variations Associated with Pharmacoresistant Epilepsy (Review)
MOLECULAR MEDICINE REPORTS 21: 1685-1701, 2020 Genetic variations associated with pharmacoresistant epilepsy (Review) NOEMÍ CÁRDENAS-RODRÍGUEZ1*, LILIANA CARMONA-APARICIO1*, DIANA L. PÉREZ-LOZANO1,2, DANIEL ORTEGA-CUELLAR3, SAÚL GÓMEZ-MANZO4 and IVÁN IGNACIO-MEJÍA5,6 1Laboratory of Neuroscience, National Institute of Pediatrics, Ministry of Health, Coyoacán, Mexico City 04530; 2Department of Postgraduate of Medical, Dental and Health Sciences, Clinical Experimental Health Research, National Autonomous University of Mexico, Mexico City 04510; Laboratories of 3Experimental Nutrition and 4Genetic Biochemistry, National Institute of Pediatrics, Ministry of Health, Coyoacán, Mexico City 04530; 5Laboratory of Translational Medicine, Military School of Health Graduates, Lomas de Sotelo, Militar, Mexico City 11200; 6Section of Research and Graduate Studies, Superior School of Medicine, National Polytechnic Institute, Mexico City 11340, Mexico Received August 28, 2019; Accepted January 16, 2020 DOI: 10.3892/mmr.2020.10999 Abstract. Epilepsy is a common, serious neurological disorder the pathophysiological processes that underlie this common worldwide. Although this disease can be successfully treated human neurological disease. in most cases, not all patients respond favorably to medical treatments, which can lead to pharmacoresistant epilepsy. Drug-resistant epilepsy can be caused by a number of mecha- Contents nisms that may involve environmental and genetic factors, as well as disease- and drug-related factors. In recent years, 1. Introduction numerous studies have demonstrated that genetic variation is 2. Pharmacoresistant epilepsy involved in the drug resistance of epilepsy, especially genetic 3. Genetic variations associated with pharmacoresistant variations found in drug resistance-related genes, including epilepsy the voltage-dependent sodium and potassium channels genes, 4. The role of genetic variants in the diagnosis and treatment and the metabolizer of endogenous and xenobiotic substances of pharmacoresistant epilepsy genes. -

Graded Co-Expression of Ion Channel, Neurofilament, and Synaptic Genes in Fast- Spiking Vestibular Nucleus Neurons
Research Articles: Cellular/Molecular Graded co-expression of ion channel, neurofilament, and synaptic genes in fast- spiking vestibular nucleus neurons https://doi.org/10.1523/JNEUROSCI.1500-19.2019 Cite as: J. Neurosci 2019; 10.1523/JNEUROSCI.1500-19.2019 Received: 26 June 2019 Revised: 11 October 2019 Accepted: 25 October 2019 This Early Release article has been peer-reviewed and accepted, but has not been through the composition and copyediting processes. The final version may differ slightly in style or formatting and will contain links to any extended data. Alerts: Sign up at www.jneurosci.org/alerts to receive customized email alerts when the fully formatted version of this article is published. Copyright © 2019 the authors 1 Graded co-expression of ion channel, neurofilament, and synaptic genes in fast-spiking 2 vestibular nucleus neurons 3 4 Abbreviated title: A fast-spiking gene module 5 6 Takashi Kodama1, 2, 3, Aryn Gittis, 3, 4, 5, Minyoung Shin2, Keith Kelleher2, 3, Kristine Kolkman3, 4, 7 Lauren McElvain3, 4, Minh Lam1, and Sascha du Lac1, 2, 3 8 9 1 Johns Hopkins University School of Medicine, Baltimore MD, 21205 10 2 Howard Hughes Medical Institute, La Jolla, CA, 92037 11 3 Salk Institute for Biological Studies, La Jolla, CA, 92037 12 4 Neurosciences Graduate Program, University of California San Diego, La Jolla, CA, 92037 13 5 Carnegie Mellon University, Pittsburgh, PA, 15213 14 15 Corresponding Authors: 16 Takashi Kodama ([email protected]) 17 Sascha du Lac ([email protected]) 18 Department of Otolaryngology-Head and Neck Surgery 19 The Johns Hopkins University School of Medicine 20 Ross Research Building 420, 720 Rutland Avenue, Baltimore, Maryland, 21205 21 22 23 Conflict of Interest 24 The authors declare no competing financial interests.