Trauma Assessment and Patient Destination TIME REQUIRED
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Paramedic National EMS Education Standard
NORTHWEST COMMUNITY EMERGENCY MEDICAL SERVICES SYSTEM CCCooonnntttiiinnnuuuiiinnnggg EEEddduuucccaaatttiiiooonnn SSSeeepppttteeemmmbbbeeerrr 222000111222 EEyyee && EEaarr DDiissoorrddeerrss && TTrraauummaa Questions/comments are welcome. Please direct to Jen Dyer, RN, EMT-P EMS Educator NWC EMSS Con-Ed Eye and Ear Disorders and Trauma September 2012 – page 1 Paramedic National EMS Education Standard Integrates assessment findings with principles of pathophysiology to formulate a field impression and implement a treatment/disposition plan for patients with eye and ear disorders/trauma. Objectives: Upon completion of the class and review of the independent study materials and post-test question bank, each participant will do the following with a degree of accuracy that meets or exceeds the standards established for their scope of practice: 1. Identify the anatomical structures of the eye and describe the corresponding physiologic function of each. (C) 2. Explain the physiology of normal vision. (C) 3. Identify the anatomic structures of the ear and describe the corresponding physiologic function of each. (C) 4. Explain the physiology of normal hearing. (C) 5. Explain the physiology of equilibrium. (C) 6. Select and discuss maneuvers for assessing eye structures and functions (C) and demonstrate a thorough EMS assessment of ocular structures, visual acuity, pupils and ocular movements. (P) 7. Distinguish abnormal assessment findings/conditions of the eye: blurred vision, diplopia, photophobia, changes in vision, flashing, pupil exam, Adie’s pupil, oculomotor nerve paralysis, Horner’s Syndrome, blindness, deviation/paralytic strabismus, orbit fracture, cataracts, conjunctivitis, color blindness, near sightedness, farsightedness, astigmatism, amblyopia, burns of the eye, corneal abrasions, foreign body, inflammation of the eyelid, glaucoma, hyphema, iritis, orbital cellulitis, macular degeneration and trauma. -

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -
5 Minute EMS Clinic-The First Five Minutes V2
EMS Basics: The First 5 Minutes For fire departments who offer both fire and OPQRST EMS services, approximately 75-80% of all ONSET-What was patient doing calls are medically-based. Not every fire de- when the symptoms started? partment is fortunate enough to have EMT’s or PROVOKES/PALLIATES- paramedics on their fire trucks. Regardless of Does anything make the pain your crew’s level of medical training, there are worse/better? several goals that MUST be accomplished QUALITY-Describe the pain within the first five minutes of patient contact. (sharp, dull, throbbing, etc.). Accomplishing these goals will directly im- prove patient outcomes. RADIATES-Does the pain radi- ate somewhere else? GOAL #1—-PROTECT YOURSELF: SEVERITY-On a scale from 1- Wear proper PPE (gloves, etc.) and ensure that the scene is safe prior to entry. 10 with 10 being the worst pain, rate your pain level. GOAL #2—-FOR CRITICAL PATIENTS, PERFORM IMMEDIATE INTERVENTIONS: TIME-When did the symptoms UNCONSCIOUS PATIENT = Open & protect airway start? CARDIAC ARREST = Perform CPR UNCONTROLLED BLEEDING = Direct pressure, bandage, elevate, & treat for shock SEVERE SHORTNESS OF BREATH = Administer high-flow oxygen GOAL #3—-OBTAIN THE FOLLOWING: Vital Signs = Blood Pressure, Pulse (rate/quality), Respiratory Rate, Lung Sounds, Blood Glucose, etc. OPQRST/SAMPLE History of current illness (see right column) GOAL #4—-DOCUMENT PATIENT’S DEMOGRAPHIC INFORMATION: Write down patient’s name, date of birth, social security number, phone number, etc. This information will be very helpful for the incoming ambulance crew. FOR THE OFFICER SAMPLE Make sure that your crew knows your expectations and their roles PRIOR to the alarm. -

Airway – Oropharyngeal: Insertion; Maintenance; Suction; Removal
Policies & Procedures Title: AIRWAY – OROPHARYNGEAL: INSERTION; MAINTENANCE; SUCTION; REMOVAL I.D. Number: 1159 Authorization Source: Nursing Date Revised: September 2014 [X] SHR Nursing Practice Committee Date Effective: October 2002 Date Reaffirmed: January 2016 Scope: SHR Acute, Parkridge Centre Any PRINTED version of this document is only accurate up to the date of printing 30-May-16. Saskatoon Health Region (SHR) cannot guarantee the currency or accuracy of any printed policy. Always refer to the Policies and Procedures site for the most current versions of documents in effect. SHR accepts no responsibility for use of this material by any person or organization not associated with SHR. No part of this document may be reproduced in any form for publication without permission of SHR. 1. PURPOSE 1.1 To safely and effectively use Oropharyngeal Airway (OPA). 2. POLICY 2.1 The Registered Nurse (RN), Registered Psychiatric Nurse (RPN), Licensed Practical Nurse (LPN), Graduate Nurse (GN), Graduate Psychiatric Nurse (GPN), Graduate Licensed Practical Nurse (GLPN) will insert, maintain, suction and remove an oropharyngeal airway (OPA). 2.2 The OPA may be inserted to establish and assist in maintaining a patent airway. 2.3 An OPA should only be used in patients with decreased level of consciousness or decreased gag reflex. 2.4 Patients with OPAs that have been inserted for airway protection should not be left unattended due to risk of aspiration if gag reflex returns unexpectedly. Page 1 of 4 Policies and Procedures: Airway – Oropharyngeal: Insertion; Maintenance; I.D. # 1159 Suction; Removal 3. PROCEDURE 3.1 Equipment: • Oropharyngeal airway of appropriate size • Tongue blade (optional) • Clean gloves • Optional: suction equipment, bag-valve-mask device 3.2 Estimate the appropriate size of airway by aligning the tube on the side of the patient’s face parallel to the teeth and choosing an airway that extends from the ear lobe to the corner of the mouth. -

Cert Disaster Medical Operations Guidelines & Treatment Protocol
WALNUT CREEK, CA COMMUNITY EMERGENCY RESPONSE TEAMS (CERT) CERT DISASTER MEDICAL OPERATIONS GUIDELINES & TREATMENT PROTOCOL TRAINING MANUAL October, 2013 Walnut Creek Community Emergency Response Teams (CERT) Disaster Medical Operations Guidelines & Treatment Protocol Training Manual CERT Disaster Medical Operations (CERT MED OPS) Mission Statement Mission: To provide the greatest good for the greatest number of people. Following a major disaster, CERT volunteers will be called upon to Triage and provide basic first aid care to members of the community that sustain injury of all types and levels of severity. Policy: CERT Medical Operations will function and provide care consistent with national CERT Training guidelines. The CERT Volunteers will function within these guidelines. Structure: CERT Medical Operations (CERT MED OPS) reports to Operations Section. CERT MED OPS Volunteer Requirements CERT MED OPS volunteers will Triage and assess each victim, as needed, according to the RPM & Simple Triage and Rapid Treatment (START) techniques that they learned during CERT training. They will treat airway obstruction, bleeding, and shock by using START techniques. They will treat the victims according to the CERT training guidelines and CERT skills limitations. CERT MED OPS volunteers will also evaluate each victim by conducting a Head-To-Toe Assessment, and perform basic first aid in a safe and sanitary manner. CERT MED OPS volunteers will ensure that victim care is documented so information can be communicated to advanced medical care when and as it becomes available. CERT MED OPS volunteers understand that CPR is not initiated in Disaster Medical Operations e.g., mass casualty disaster situations. The utmost of care and compassion will be undertaken with family members to assist them with their grieving process. -
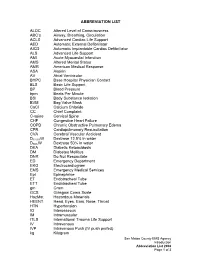
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

Best Airway and Ventilation Strategy During CPR and After Resuscitation
Best airway and ventilation strategy during CPR and after resuscitation After cardiac arrest a combination of basic and advanced airway and ventilation techniques are used during cardiopulmonary resuscitation (CPR) and after a return of spontaneous circulation (ROSC). Current guidelines are based predominantly on evidence from observational studies and expert consensus; thus, the optimal combination of airway techniques and oxygen and ventilation targets during CPR and after ROSC is uncertain, according to a review article in the journal Critical Care. Current evidence supports a stepwise approach to airway management based on patient factors, rescuer skills and the stage of resuscitation. Observational data suggest that early lay-bystander compression-only CPR can improve survival after sudden cardiac arrest. Chest compressions are easy to learn and do for most rescuers and do not require special equipment. Studies show that lay rescuer compression-only CPR is better than no CPR. During CPR, airway interventions range from compression-only CPR with or without airway opening, mouth-to-mouth ventilation, mouth-to-mask ventilation, bag-mask ventilation (with or without an oropharyngeal airway) or advanced airways (supraglottic airways [SGAs] and tracheal intubation using direct or video laryngoscopy). On arrival of trained rescuers, bag-mask ventilation with supplemental oxygen is the most common initial approach and can be aided with an oropharyngeal or nasopharyngeal airway. During CPR, the bag-mask is used to give two breaths after every 30 compressions. A pre-specified per-protocol analysis reported a significantly higher survival to discharge among those who actually received conventional CPR (30:2) compared with those who received continuous compressions. -

The Golden Hour > How Time Shapes Airway Management > by Charlie Eisele,BS,NREMT-P
September 2008 The A supplement to JEMS (the Journal of Emergency Medical Services) Conscience of EMS JOURNAL OF EMERGENCY MEDICAL SERVICES Sponsored by Verathon Inc. ELSEVIER PUBLIC SAFETY The Perfect View How Video Laryngoscopy Is Changing the Face of Prehospital Airway Management A supplement to September 2008 JEMS, sponsored by Verathon Inc. 4 Foreword > To See or Not to See, That Is the Question > By A.J.Heightman,MPA,EMT-P 5 5 The Golden Hour > How Time Shapes Airway Management > By Charlie Eisele,BS,NREMT-P 9 The Video Laryngoscopy Movement > Can-Do Technology at Work > By John Allen Pacey,MD,FRCSc 11 ‘Grounded’ Care > Use of Video Laryngoscopy in a Ground 11 EMS System: Better for You, Better for Your Patients > By Marvin Wayne,MD,FACEP,FAAEM 14 Up in the Air > Video Laryngoscopy Holds Promise for In-Flight Intubation > By Lars P.Bjoernsen,MD,& M.Bruce Lindsay,MD 16 16 The Military Experience > The GlideScope Ranger Improves Visualization in the Combat Setting > By Michael R.Hawkins,MS,CRNA 19 Using Is Believing > Highlights from 72 Cases Involving Video Laryngoscopy at Martin County (Fla.) Fire Rescue > By David Zarker,EMT-P 21 Teaching the Airway > Designing Educational Programs for 21 Emergency Airway Management > By Michael F.Murphy,MD; Ron M.Walls,MD; & Robert C.Luten,MD COVER PHOTO KEVIN LINK Disclosure of Author Relationships: Authors have been asked to disclose any relationships they may have with commercial supporters of this supplement or with companies that may have relevance to the content of the supplement. Such disclosure at the end of each article is intended to provide readers with sufficient information to evaluate whether any material in the supplement has been influenced by the writer’s relationship(s) or financial interests with said companies. -

2012 2013 First Aid Contest Rules
2016 FIRST AID CONTEST RULES INDEX Section II Title Page Rules Governing the 2016 First Aid Contest ........................................................................ 1 Scorecard A Discounts ............................................................................................................ 8 Interpretations of Scorecard B (Artificial Ventilation/Cardiopulmonary Resuscitation). ........................................................................................................................ 12 Skill Sheets Initial Assessment .................................................................................................................. 15 Patient Assessment ................................................................................................................ 16 Automated External Defibrillator ........................................................................................ 19 One-Person CPR (Manikin Only) ........................................................................................ 18 Two-Rescuer CPR (Manikin Only) ...................................................................................... 20 Mouth-to-Mask Resuscitation .............................................................................................. 24 Airway Obstruction ............................................................................................................... 25 Sucking Chest Wound .......................................................................................................... -

Success Rate of Resuscitation After Out-Of-Hospital Cardiac Arrest
Commentary Success rate of resuscitation after out-of-hospital cardiac arrest Anthony MH Ho1, FRCPC, FCCP, Glenio B Mizubuti1 *, MSc, MD, Adrienne K Ho2, MB, BS, Song Wan3, MD, FRCS, Devin Sydor1, MD, FRCPC, David C Chung4, MD, FRCPC 1Department of Anesthesiology and Perioperative Medicine, Queen’s University, Canada 2Department of Oncology, The Christie NHS Foundation Trust, Manchester, United Kingdom 3Division of Cardiac Surgery, Department of Surgery, The Chinese University of Hong Kong, Shatin, Hong Kong 4Department of Anaesthesia and Intensive Care, The Chinese University of Hong Kong, Shatin, Hong Kong * Corresponding author: [email protected] Hong Kong Med J 2019;25:254–6 https://doi.org/10.12809/hkmj187596 A recent study in Hong Kong documented the low lack of which is linked to poor outcomes.5 However, success rate of resuscitation after adult out-of-hospital because 60% of adult and 38% of paediatric OHCAs cardiac arrest (OHCA). Survival to hospital discharge in Hong Kong are unwitnessed,1,4 these first few with good neurological outcome was 1.5%.1 A median minutes of sufficient oxygen in the blood (for sudden delay of 12 minutes for defibrillation was one factor arrest of cardiac origin) may have already elapsed. that contributed to poor outcomes.1 In ventricular This raises the question of whether a one-size-fits- fibrillation or pulseless ventricular tachycardia, every all bystander CPR with no breathing component minute without defibrillation drastically reduces is advisable. It is not surprising that the rates of the chance of successful resuscitation.2 To partially survival with good neurological outcomes are mitigate the delayed arrival of trained personnel to low. -

Abc of Occupational and Environmental Medicine
ABC OF OCCUPATIONAL AND ENVIRONMENT OF OCCUPATIONAL This ABC covers all the major areas of occupational and environmental ABC medicine that the non-specialist will want to know about. It updates the OF material in ABC of W ork Related Disorders and most of the chapters have been rewritten and expanded. New information is provided on a range of environmental issues, yet the book maintains its practical approach, giving guidance on the diagnosis and day to day management of the main occupational disorders. OCCUPATIONAL AND Contents include ¥ Hazards of work ¥ Occupational health practice and investigating the workplace ENVIRONMENTAL ¥ Legal aspects and fitness for work ¥ Musculoskeletal disorders AL MEDICINE ¥ Psychological factors ¥ Human factors ¥ Physical agents MEDICINE ¥ Infectious and respiratory diseases ¥ Cancers and skin disease ¥ Genetics and reproduction Ð SECOND EDITION ¥ Global issues and pollution SECOND EDITION ¥ New occupational and environmental diseases Written by leading specialists in the field, this ABC is a valuable reference for students of occupational and environmental medicine, general practitioners, and others who want to know more about this increasingly important subject. Related titles from BMJ Books ABC of Allergies ABC of Dermatology Epidemiology of Work Related Diseases General medicine Snashall and Patel www.bmjbooks.com Edited by David Snashall and Dipti Patel SNAS-FM.qxd 6/28/03 11:38 AM Page i ABC OF OCCUPATIONAL AND ENVIRONMENTAL MEDICINE Second Edition SNAS-FM.qxd 6/28/03 11:38 AM Page ii SNAS-FM.qxd 6/28/03 11:38 AM Page iii ABC OF OCCUPATIONAL AND ENVIRONMENTAL MEDICINE Second Edition Edited by DAVID SNASHALL Head of Occupational Health Services, Guy’s and St Thomas’s Hospital NHS Trust, London Chief Medical Adviser, Health and Safety Executive, London DIPTI PATEL Consultant Occupational Physician, British Broadcasting Corporation, London SNAS-FM.qxd 6/28/03 11:38 AM Page iv © BMJ Publishing Group 1997, 2003 All rights reserved. -

When Doing TRIAGE, You MUST Protect Yourself and Your Buddy
CERT Unit 3– DMO #1 Spring 2018 Assumptions Disaster Medical Operations ● Need for CERT members to learn disaster medical operations is based on two — Part 1 assumptions: ! Number of victims could exceed local capacity for treatment ! Survivors will assist others ‒ They will do whatever they know how to do CERT Basic Training ‒ They need to know lifesaving first aid or post- Unit 3 disaster survival techniques Spring 2018 90% of disaster victims are rescued by other victims! Importance of Quick Action Unit Objectives – Learn how to: ● Phase 1: Death within minutes, result of ● Identify “killers” severe trauma ● Conduct TRIAGE under ● Phase 2: Death within several hours, simulated disaster result of excessive bleeding conditions ● Phase 3: Death in several days or weeks, ● Open airway, control result of infection bleeding, and treat for shock Rescuer Safety During Triage TRIAGE AND PPE’s ● If hazmat or terrorist event is suspected, CERT members DO NOT respond When doing TRIAGE, ! Evacuate as safely as possible ● ALWAYS wear PPE: you MUST protect ! Helmet ! Goggles yourself ! N95 mask ! Work gloves and your buddy ! Sturdy shoes or boots ! Non-latex exam gloves must do the same 1 CERT Unit 3– DMO #1 Spring 2018 Personal Protective Equipment - PPE Personal Protective Equipment - PPE ● Personal protective equipment, commonly ● How to put on and take off Non-Latex referred to as "PPE", is equipment worn to Gloves minimize exposure to serious workplace ● Practice! injuries and illnesses. ● New gloves for every victim ● Wash or sanitize hands Goggles Masks after de-gloving Gloves Personal Protective Equipment - PPE IF IT’S WET AND NOT YOURS DON’T TOUCH IT! Three “Killers” - ABS CERT Sizeup ● Emergency medicine “killers” 1.