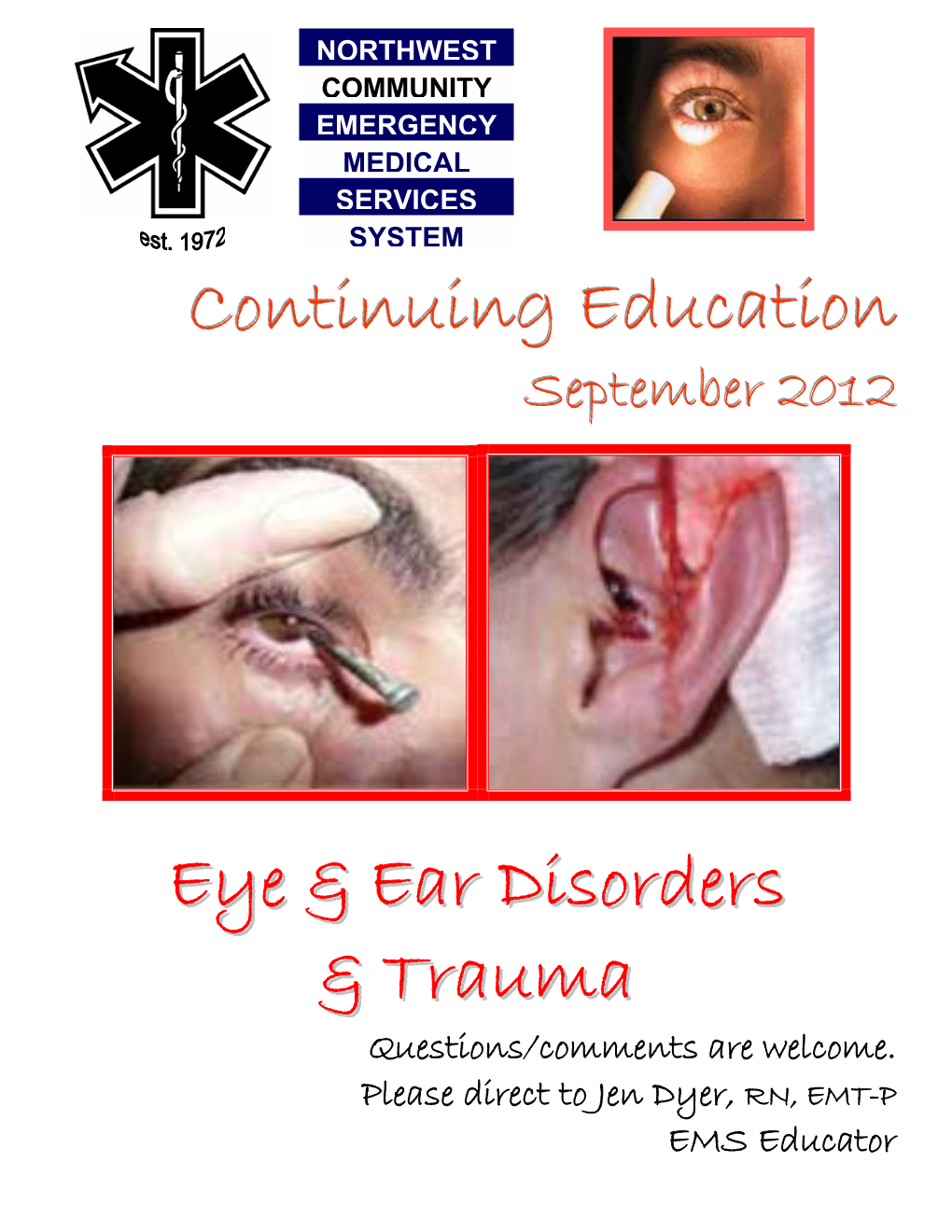
Paramedic National EMS Education Standard
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
5 Minute EMS Clinic-The First Five Minutes V2
EMS Basics: The First 5 Minutes For fire departments who offer both fire and OPQRST EMS services, approximately 75-80% of all ONSET-What was patient doing calls are medically-based. Not every fire de- when the symptoms started? partment is fortunate enough to have EMT’s or PROVOKES/PALLIATES- paramedics on their fire trucks. Regardless of Does anything make the pain your crew’s level of medical training, there are worse/better? several goals that MUST be accomplished QUALITY-Describe the pain within the first five minutes of patient contact. (sharp, dull, throbbing, etc.). Accomplishing these goals will directly im- prove patient outcomes. RADIATES-Does the pain radi- ate somewhere else? GOAL #1—-PROTECT YOURSELF: SEVERITY-On a scale from 1- Wear proper PPE (gloves, etc.) and ensure that the scene is safe prior to entry. 10 with 10 being the worst pain, rate your pain level. GOAL #2—-FOR CRITICAL PATIENTS, PERFORM IMMEDIATE INTERVENTIONS: TIME-When did the symptoms UNCONSCIOUS PATIENT = Open & protect airway start? CARDIAC ARREST = Perform CPR UNCONTROLLED BLEEDING = Direct pressure, bandage, elevate, & treat for shock SEVERE SHORTNESS OF BREATH = Administer high-flow oxygen GOAL #3—-OBTAIN THE FOLLOWING: Vital Signs = Blood Pressure, Pulse (rate/quality), Respiratory Rate, Lung Sounds, Blood Glucose, etc. OPQRST/SAMPLE History of current illness (see right column) GOAL #4—-DOCUMENT PATIENT’S DEMOGRAPHIC INFORMATION: Write down patient’s name, date of birth, social security number, phone number, etc. This information will be very helpful for the incoming ambulance crew. FOR THE OFFICER SAMPLE Make sure that your crew knows your expectations and their roles PRIOR to the alarm. -

Week of July 27, 2015 – Eye Injuries Protecting Your Eyes from Injury Is
Week of July 27, 2015 – Eye Injuries Protecting your eyes from injury is one of the most basic things you can do to keep your vision healthy throughout your life. And the most basic step a person can take to protect his/her eyes is wearing the proper protective eyewear. According to a national survey by the American Academy of Ophthalmology, only 35 percent of respondents said they always wear protective eyewear when performing home repairs or maintenance; even fewer do so while playing sports. Eye emergencies include: cuts, scratches, getting objects in the eye, burns, chemical exposures, and blunt injuries to the eye or eyelid. Certain eye infections and other medical conditions, such as blood clots or glaucoma, also represent serious conditions. Since the eye is easily damaged, any of these conditions can lead to vision loss. A black eye is a bruise and usually caused by direct trauma to the eye or face. The bruise is caused by bleeding under the skin. The tissue around the eye turns black and blue, gradually, over a few days, it changes to purple, green, and yellow. The abnormal color disappears within 2 weeks. Swelling of the eyelid and tissue around the eye may also occur. Certain types of skull fractures may also result in bruising around the eyes, even without direct injury to the eye. Sometimes, serious damage to the eye itself occurs from the pressure of a swollen eyelid or face and can result is a hyphema; which is blood in the front area of the eye. Trauma is a common cause of the condition and is often due to a direct hit to the eye from a ball. -

Diagnosing Depressed Skull Fracture in a Young Child
Nursing Practice Keywords: Skull fracture/Children/ Neurology Case study Neurology Skull fractures associated with intracranial injury are a leading cause of traumatic death in childhood. Children with head injuries should be monitored for signs of deterioration Diagnosing depressed skull fracture in a young child respiratory rate 32/min and oxygen satura- In this article... tion 97% in air. He was drowsy but easily Risks associated with head injury and skull fracture roused by his parents. The Glasgow Coma Scale score was 12/15, which could indicate The importance of monitoring and early diagnosis an intracranial injury and raised intracra- nial pressure. A neurological examination revealed Authors Shameem Ahmed is assistant left-sided hemi-paresis indicative of raised professor in neurosurgery; Rupa Thenseen intracranial pressure. A right-sided lateral Frank is sister in charge, neurosurgical soft tissue swelling and haematoma along operation theatre; both at Gauhati Medical with a depression of the underlying bones College, Guwahati, India; Siba Prosad Paul was noted on palpation of his skull. is specialty trainee in neonates at South- He was reviewed by an anaesthetist and mead Hospital, Bristol his condition was considered to be stable. An urgent non-contrast computed tomog- ead injury is the most common raphy scan revealed a large depressed frac- cause of death and disability in ture (>5mm) involving the right fronto- people aged below 40 years parieto-occipital bone (Fig 1). The boy was H(National Institute for Health Fig 1. Large right fronto-parieto-occipital reviewed by the neurosurgical team and an and Care Excellence, 2014). It accounts for bone simple depressed fracture exploration and elevation of the depressed 1.4 million attendances at accident and fragment was carried out on the same day. -

Causes and Characteristics of Peri-Orbital Contusions and Their Relationship with Intracranial Injuries in Inward Patients in Two Tertiary Care Hospitals in Sri Lanka
Medico-Legal Journal of Sri Lanka, 2020 December Vol. 8, Issue 2 Original article Causes and Characteristics of Peri-Orbital Contusions and Their Relationship with Intracranial Injuries in Inward Patients in Two Tertiary Care Hospitals in Sri Lanka Warushahennadi J1*, Senavirathne AS2, Godakandage SSP3, Pathirana MD4, Jayarathne UGB5, Ambepitiya SGH2 1Department of Forensic Medicine, Faculty of Medicine, University of Ruhuna, Sri Lanka, 2Office of the Judicial Medical Officer, District General Hospital, Matara, Sri Lanka, 3Family Health Bureau, Sri Lanka, 4National Hospital of Sri Lanka, 5Office of the Judicial Medical Officer, Teaching Hospital, Karapitiya, Sri Lanka Abstract Introduction: The peri-orbital contusion (PC) is a common injury in day to day surgical casualties. It is a common injury observed in patients who are in an unconscious state following head injuries. The aim of the study is to describe characteristics of PC and understand its relationship with associated injuries, especially with facial injuries and intracranial injuries. Methods: This retrospective study reviewed the medico-legal examination forms (MLEF) of 67 inward patients in Teaching Hospital, Karapitiya and District General Hospital, Matara with peri-orbital contusions following trauma during a period of six months from January 2020 to June 2020. Results: A total number of 67 patients were included with 81% being male patients. The commonest soft tissue injuries around the PCs were abrasions (n=39, 71%) and 25 (38%) of the study sample had fractures of the skull. The majority (n=22, 88%) of them had fractures of facial bones followed by vault and basal skull fractures. The majority of PCs (45%) were blue in colour and only 8% were red. -

2012 2013 First Aid Contest Rules
2016 FIRST AID CONTEST RULES INDEX Section II Title Page Rules Governing the 2016 First Aid Contest ........................................................................ 1 Scorecard A Discounts ............................................................................................................ 8 Interpretations of Scorecard B (Artificial Ventilation/Cardiopulmonary Resuscitation). ........................................................................................................................ 12 Skill Sheets Initial Assessment .................................................................................................................. 15 Patient Assessment ................................................................................................................ 16 Automated External Defibrillator ........................................................................................ 19 One-Person CPR (Manikin Only) ........................................................................................ 18 Two-Rescuer CPR (Manikin Only) ...................................................................................... 20 Mouth-to-Mask Resuscitation .............................................................................................. 24 Airway Obstruction ............................................................................................................... 25 Sucking Chest Wound .......................................................................................................... -

Head Injury Policy
Date January 2020 Review Date January 2021 Responsibility Senior Sister HEAD INJURY POLICY The following has been developed in accordance with NICE clinical guideline 56 - Head Injury, International Rugby Board Concussion Guidelines and the RFU Guidelines for schools and colleges. Background Injuries to the head can occur in many situations in the school environment i.e. any time that pupil’s head comes into contact with a hard object such as the floor, a desk, or another pupil’s body. The potential is probably greatest during activities where collisions can occur such as in the playground, during sport and PE, and if messing around indoors during breaks. The nature of rugby means that concussion can occur during both training and in matches. Concussion is a disturbance of the normal working of the brain without causing any structural damage. It usually follows a blow directly to the head, or indirectly if the head is shaken when the body is struck. It is important to recognise that it is not necessary to lose consciousness to sustain a concussion following a blow to the head. The risk of injury is dependent upon the velocity and the force of the impact, the part of the head involved in the impact, and any pre-existing medical conditions. Symptoms may not develop for some hours, or even days, after a knock to the head, and in rare cases can develop weeks after a head injury. Whilst an initial concussion is unlikely to cause any permanent damage, a repeat injury to the head soon after a prior, unresolved concussion can have serious consequences. -

OCULAR TRAUMA Accidents and from High Velocity Missiles at the Workplace
!!!!!!!!!!!!!! !Kr!ieg!er !Eye!Ins!tit!ute!at!Sin!ai!Ho!spi!tal ! !!!!!!!!!!!!!! !!!!!!!!!!!!!! !e!y!!e !!l!i!g!!h!!t!s ! !!!!!!!!!!!!!! Spring 2006 of injury can occur from a shattered windschield in road traffic OCULAR TRAUMA accidents and from high velocity missiles at the workplace. Foreign bodies are most frequently found on the cornea and under the eyelid where they EYE INJURY can be easily removed. We have seen a progressive increase in eye trauma resulting Eye injury occurs frequently in the United States where nearly from automobile accidents in the past seven years. Frontal air two million individuals require treatment in the hospital (60%) bag deployment was associated with a statistically significant, or doctor’s office (40%) every year. Males are four times more two-fold increased risk of eye injury, whereas seat belt use was likely than females to have ocular injuries, and eye injuries occur associated with a two-fold reduced eye injury risk. Seat belt use mostly among persons in their 20s or younger. However, as the is the most effective means of occupant protection against auto - population ages, we are seeing an increasing number of eye mobile accident-related eye injury. injuries in the elderly. Older age, being female, passenger seat position and collision Most injuries occur in the home, are sports-related or work- severity were also associated with eye injury risk. related or are the result of an assault or result from a motor vehicle accident. The most common objects EYE PROTECTION to strike the eye are fists, thrown objects Many cases of ocular injury can be prevented by wearing (e.g., stones, balls), BBs, pellets and sticks. -

When Doing TRIAGE, You MUST Protect Yourself and Your Buddy
CERT Unit 3– DMO #1 Spring 2018 Assumptions Disaster Medical Operations ● Need for CERT members to learn disaster medical operations is based on two — Part 1 assumptions: ! Number of victims could exceed local capacity for treatment ! Survivors will assist others ‒ They will do whatever they know how to do CERT Basic Training ‒ They need to know lifesaving first aid or post- Unit 3 disaster survival techniques Spring 2018 90% of disaster victims are rescued by other victims! Importance of Quick Action Unit Objectives – Learn how to: ● Phase 1: Death within minutes, result of ● Identify “killers” severe trauma ● Conduct TRIAGE under ● Phase 2: Death within several hours, simulated disaster result of excessive bleeding conditions ● Phase 3: Death in several days or weeks, ● Open airway, control result of infection bleeding, and treat for shock Rescuer Safety During Triage TRIAGE AND PPE’s ● If hazmat or terrorist event is suspected, CERT members DO NOT respond When doing TRIAGE, ! Evacuate as safely as possible ● ALWAYS wear PPE: you MUST protect ! Helmet ! Goggles yourself ! N95 mask ! Work gloves and your buddy ! Sturdy shoes or boots ! Non-latex exam gloves must do the same 1 CERT Unit 3– DMO #1 Spring 2018 Personal Protective Equipment - PPE Personal Protective Equipment - PPE ● Personal protective equipment, commonly ● How to put on and take off Non-Latex referred to as "PPE", is equipment worn to Gloves minimize exposure to serious workplace ● Practice! injuries and illnesses. ● New gloves for every victim ● Wash or sanitize hands Goggles Masks after de-gloving Gloves Personal Protective Equipment - PPE IF IT’S WET AND NOT YOURS DON’T TOUCH IT! Three “Killers” - ABS CERT Sizeup ● Emergency medicine “killers” 1. -

Emergency Drill Triage Kit Instruction Guide
Emergency Drill Triage Kit Instruction Guide During major emergencies schools must be prepared to be self-reliant This kit does not require because it is universally understood that local first responders will advanced training or be overwhelmed. Schools will need to be ready to rescue and treat equipment. The skills injured victims using only the skills and training of the school staff. This that this kit will review Emergency Drill Triage Kit was created in collaboration with the Pediatric are the same skills Disaster Resource and Training Center at Childrens Hospital Los Angeles. taught in Basic First Aid It is intended to support school personnel as they practice identifying, and CPR classes. reporting, transporting and treating injured victims. This kit is designed to help school personnel review their Basic First Aid training and practice those skills. m num ti b ic e v r Objects fell onto patient. 9 VISUAL CUES A key component of this kit is the 40 mock victim tags. These victim Cut on Non-bleeding scalp laceration; head and right foot swollen tags were created based on historical data of earthquake-related VICTIM INFORMATION and tender. rightEmergency Triage Drillfoot injuries. Experts from Childrens Hospital Los Angeles and Los Angeles pain. City Fire reviewed the mock victim scenarios and outlined first aid and medical responses. These victim tags represent the kinds of Mock Victim Tags injuries sustained by school aged children during an earthquake and 40 cards in clip pouches they are designed to review the First Aid procedures that could be Victim Checklist used during any traumatic emergency. -

View/Download
Backcountry First Aid: Prevention,Triage and Treatment Peter Heidmann DVM MPH Specialist: Equine Internal Medicine Montana Equine Equine Medicine and Surgery Board-certified Experts 406-388-8323 Dedicated to the highest quality care of horses Preparation = Prevention • Paperwork – Health Certificate, Coggins – Contact Information – Maps • Know your country • Tack – Well-fitted, well-suited • Fitness – Fatigue promotes injury – Lameness and myopathy – Colic and lacerations Triage: Lameness • Heat? Swelling? • Flexion Tests – Arthritis – Ligament Sprain • (Connects bone to bone) – Tendon Strain • (Connects muscle to bone) • 85% of lameness originates at/below fetlock – Digital Pulses • Stone Bruises • Sole Abscess • Fractured Coffin Bone (P3) Treatment: Lameness • Thermal Therapy – Ice Early -- Heat Late • Anti-inflammatory Medications – Phenylbutazone – Surpass • Limb Wraps – Minimize Swelling – Supports Soft Tissues – Extensive Padding is CRITICAL • Other Salves? Poultices? Sweats? Triage: Wounds • Location location location • Which wound is more serious? Triage: Wounds • Infection Control – Each round removes contamination: • Dirty water is better than mud • Clean water is better than dirty water • Sterile water is better than clean water – A clean wound is considered infected after 6 hours • 2 - 4 - 16 - 256 - 65,536 - 4,294,967,296!! – Antiseptic Solutions – Vaccinations – Antibiotics • Oral, Injectable, Topical • Ask your veterinarian… Triage: Eye Trauma • Use caution with “hi-line” • Eyelid Trauma • Corneal Trauma – Signs: • Squinting • Severe Tearing • Head-shyness Treatment: - Clean any wounds w/ Saline - Opthalmic Antibiotics - NO STEROID OINTMENTS! Triage: Hemorrhage Blood Loss: How Much is TOO Much?? Blood Volume is 8 - 10 % of Body Weight Eg 1000# horse = 450 Kg = 36-45 L Total Total loss of 1/10 is typically well-tolerated = 3.6 - 4.5 Liters = More than 1GALLON! Triage: Hemorrhage Treatment • Most Wounds stop bleeding spontaneously • Arterial vs. -

International Council of Ophthalmology and Based on Their Curriculum 2009
HANDBOOK FOR JUNIOR RESIDENTS AND MEDICAL STUDENTS LEARNING EMERGENCY OPHTHALMOLOGY Compiled by The Task Force on Undergraduate Teaching in Ophthalmology of the International Council of Ophthalmology and based on their curriculum 2009 1 In this booklet we have put together common ophthalmic emergency conditions that we think you need to know and key ophthalmic disorders we think you need to have seen. There are descriptions and colour pictures of these conditions. This pocket sized book summaries the key points in the ophthalmology curriculum complied by the Task Force of the International Council of Ophthalmology and is a format that is very portable! Sue Lightman, Do Nhu Hon and Peter McCluskey On behalf of the International Council of Ophthalmology and Vietnam National Institute of Ophthalmology, Hanoi Medical University 2010 Other Contributing Authors with thanks Anh Dinh Kim , Anh Nguyen Quoc, Chau Hoang Thi Minh, Dong Pham Ngoc, Ha Tran Minh, Hon Do Nhu, Ngoc Do Quang, Quan Bui Dao, Richard Andrews, Thang Nguyen Canh, Thanh Pham Thi Kim, Thuy Nguyen Thi Thu, Thuy Vu Thi Bich, Tung Mai Quoc, Van Pham Thi Khanh, Van Pham Trong, Yen Nguyen Thu, Simon Taylor 2 Have you seen? Tick Do you Tick Note for you: if yes know if yes Remember how it is to look it up caused and treated? Trauma Periorbital haematoma Orbital blowout Lid laceration Subconjunctival Haemorrhage Chemical burns – cornea and conjunctiva Foreign body Corneal abrasion Hyphema Iridodialysis Cataract Lens subluxation /dislocation Intraocular foreign body Scleral rupture 3 Painful Red Eye Chalazion Dacryocystitis Orbital cellulitis Conjunctivitis Scleritis Episcleritis Viral keratitis Bacterial keratitis Shingles Uveitis Acute angle-closure glaucoma Endophthalmitis Sudden Painless Loss of Vision Vitreous haemorrhage Retinal tear/detachment Central retinal artery occlusion Central retinal vein occlusion Others 4 Proptosis VII nerve palsy TRAUMA Ocular trauma is very common, especially in developing countries. -
EMR Standards and Procedures Manual
State of Wisconsin Emergency Medical Responder (EMR) Core Skills Standards & Procedures of Practical Skills Manual August 2013 This manual is intended to provide examples of tried and proven techniques of caring for patients with the various injuries or illnesses that emergency medical responder personnel will encounter in the field. It does not provide the only method or technique that may be an acceptable approach in caring for an injury or illness. However, since the certification examinations used within the state are based on the current edition of this document as well as the current edition of the National EMS Educational Standards, the State of Wisconsin Scope of Practice, and is a companion to the emergency medical responder curriculum, it is an advantage to use these skill procedures as the basis for practice. This is a consensus document, endorsed by the EMS Training Centers, the Department of Health Services, the Bureau of Communicable Diseases and Emergency Response - EMS Program, as well as the EMS Physician Advisory Committee. The Bureau of Communicable Diseases and Emergency Response - EMS Program, Wisconsin’s EMS State Medical Director, the EMS Physician Advisory Committee, as well as regional and local physician medical direction are charged with developing and promulgating these minimum standards of care for emergency medical responder personnel. This manual contains descriptions of those skills included in the scope of practice for the emergency medical responder. The scope of practice for each level of provider and local protocol shall define which of these skills may be used at the local level. State of Wisconsin – Standards & Procedures of Practical Skills Emergency Medical Responder – Core Skills TABLE OF CONTENTS SECTION 1 – BLOOD PRESSURE MEASUREMENT .........................................................................................................................