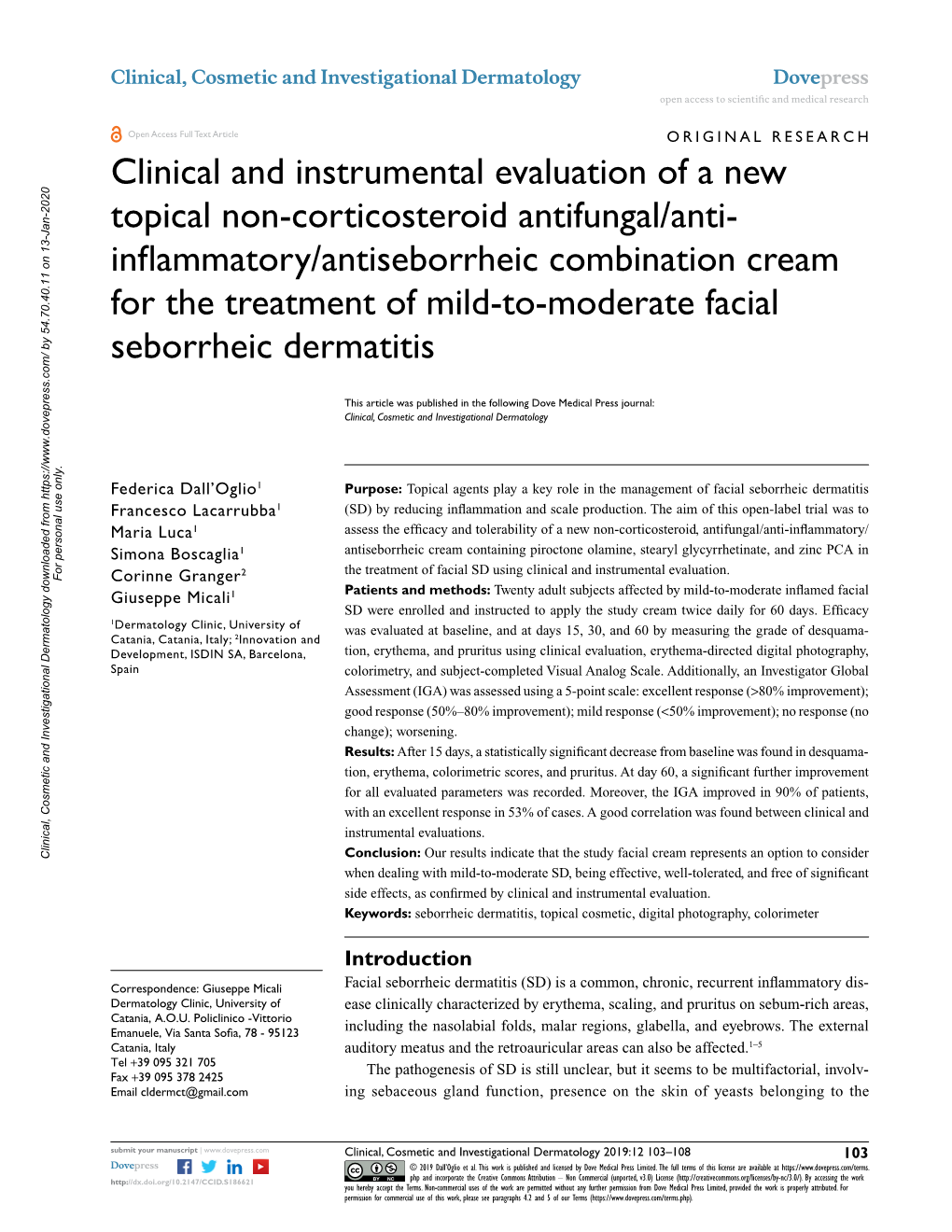
Clinical and Instrumental Evaluation of a New Topical Non-Corticosteroid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Topical Pharmaceutical Compositions
Europâisches Patentamt 0 085 579 ® ê European Patent Office @ Publication number: B1 Office européen des brevets ® EUROPEAN PATENT SPECIFICATION @ Date of publication of patent spécification: 06.05.87 ® Intel.4: A 61 K 45/06, A 61 K 31/195, A 61 K 31/20, A 61 K 31/375, (H) Application number: 83300531.7 A 61 K 31/585, A 61 K 31/19, © Date offiling: 02.02.83 A 61 K 31/61, A 61 K 31/355, A 61 K 31/715, A 61 K 33/30, A 61 K 35/78 (54) Topical pharmaceutical compositions. (§) Priority: 03.02.82 US 345204 (73) Proprietor: EFAMOL LIMITED 12th Floor Moor House London Wall London EC2Y 5HE (GB) (§) Date of publication of application: 10.08.83 Bulletin 83/32 ® Inventor: Horrobin, David Frederick P.O.Box 10 Nuns Island (§) Publication of the grant of the patent: Montréal H3E 1 J8 (CA) 06.05.87 Bulletin 87/19 Inventor: Lieb, Julian 41 Village Lane Bethany Connecticut 06525 (US) (S) Designated Contracting States: AT BE CH DE FR GB IT Ll LU NL SE (74) Représentative: Cockbain, Julian Roderick Michaelson et al - (§) Références cited: Frank B. Dehn & Co. European Patent Attorneys EP-A-0 068854 Impérial House 15-19, Kingsway US-A-3 639 625 London WC2B 6UZ (GB) US-A-4328243 CÛ O) in LO oo o o Note: Within nine months from the publication of the mention of the grant of the European patent, any person may give notice to the European Patent Office of opposition to the European patent granted. -

Alphabetical Listing of ATC Drugs & Codes
Alphabetical Listing of ATC drugs & codes. Introduction This file is an alphabetical listing of ATC codes as supplied to us in November 1999. It is supplied free as a service to those who care about good medicine use by mSupply support. To get an overview of the ATC system, use the “ATC categories.pdf” document also alvailable from www.msupply.org.nz Thanks to the WHO collaborating centre for Drug Statistics & Methodology, Norway, for supplying the raw data. I have intentionally supplied these files as PDFs so that they are not quite so easily manipulated and redistributed. I am told there is no copyright on the files, but it still seems polite to ask before using other people’s work, so please contact <[email protected]> for permission before asking us for text files. mSupply support also distributes mSupply software for inventory control, which has an inbuilt system for reporting on medicine usage using the ATC system You can download a full working version from www.msupply.org.nz Craig Drown, mSupply Support <[email protected]> April 2000 A (2-benzhydryloxyethyl)diethyl-methylammonium iodide A03AB16 0.3 g O 2-(4-chlorphenoxy)-ethanol D01AE06 4-dimethylaminophenol V03AB27 Abciximab B01AC13 25 mg P Absorbable gelatin sponge B02BC01 Acadesine C01EB13 Acamprosate V03AA03 2 g O Acarbose A10BF01 0.3 g O Acebutolol C07AB04 0.4 g O,P Acebutolol and thiazides C07BB04 Aceclidine S01EB08 Aceclidine, combinations S01EB58 Aceclofenac M01AB16 0.2 g O Acefylline piperazine R03DA09 Acemetacin M01AB11 Acenocoumarol B01AA07 5 mg O Acepromazine N05AA04 -

ACCGE 2015 Abstracts Ebook
Table of Contents Introduction/Plenary Correlated Electron Crystals 1 Detector Materials: Scintillators and Semiconductors (ACCGE) 1 Fundamentals of Crystal Growth (ACCGE) 1 III-V Nitride, SiC, and Other Wide Bandgap Materials (Joint ACCGE/OMVPE) 1 Second Symposium on 2D Electronic Materials (Joint ACCGE/OMVPE) 1 Correlated Electron Crystals 2 Detector Materials: Scintillators and Semiconductors (ACCGE) 2 Fundamentals of Crystal Growth (ACCGE) 2 III-V Nitride, SiC, and Other Wide Bandgap Materials (Joint ACCGE/OMVPE) 2 Second Symposium on 2D Electronic Materials (Joint ACCGE/OMVPE) 2 Detector Materials: Scintillators and Semiconductors (ACCGE) 3 Fundamentals of Crystal Growth (ACCGE) 3 III-V Nitride, SiC, and Other Wide Bandgap Materials (Joint ACCGE/OMVPE) 3 Second Symposium on 2D Electronic Materials (Joint ACCGE/OMVPE) 3 Poster Session 1 III-Vs on Silicon (Joint ACCGE/OMVPE) 1 Young Author and AACG Awards Detector Materials: Scintillators and Semiconductors (ACCGE) 4 Fundamentals of Crystal Growth (ACCGE) 4 III-Vs on Silicon (Joint ACCGE/OMVPE) 2 Second Symposium on 2D Electronic Materials (Joint ACCGE/OMVPE) 4 III-V Nitride, SiC, and Other Wide Bandgap Materials (Joint ACCGE/OMVPE) 4 Nonlinear Optical and Laser Host Materials (ACCGE) 1 Thin Film Growth, Epitaxy, and Superlattices (Joint ACCGE/OMVPE) 1 Second Symposium on 2D Electronic Materials (Joint ACCGE/OMVPE) 5 III-V Nitride, SiC, and Other Wide Bandgap Materials (Joint ACCGE/OMVPE) 5 Materials for Photovoltaics and Energy Technology (Joint ACCGE/OMVPE) 1 Nonlinear Optical and -

(12) Patent Application Publication (10) Pub. No.: US 2016/0354315 A1 Li (43) Pub
US 20160354315A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2016/0354315 A1 Li (43) Pub. Date: Dec. 8, 2016 (54) DOSAGE FORMS AND USE THEREOF Publication Classification (71) Applicant: Triastek, Inc., Nanjing (CN) (51) Int. Cl. A69/20 (2006.01) (72) Inventor: Xiaoling Li, Dublin, CA (US) A6IR 9/24 (2006.01) A63L/92 (2006.01) (52) U.S. Cl. (21) Appl. No.: 15/173,596 CPC ........... A61K 9/2031 (2013.01); A61K 9/2027 (2013.01); A61K 31/192 (2013.01); A61 K 9/209 (2013.01) (22) Filed: Jun. 3, 2016 (57) ABSTRACT The present disclosure provides a stable solid pharmaceuti Related U.S. Application Data cal dosage form for oral administration. The dosage form includes a Substrate that forms at least one compartment and (60) Provisional application No. 62/170,645, filed on Jun. a drug content loaded into the compartment. The dosage 3, 2015, provisional application No. 62/313,092, filed form is so designed that the active pharmaceutical ingredient on Mar. 24, 2016. of the drug content is released in a controlled manner. Patent Application Publication Dec. 8, 2016 Sheet 1 of 20 US 2016/0354315 A1 FG. A F.G. B. Peak carcetitration, tax ise F.G. C Patent Application Publication Dec. 8, 2016 Sheet 2 of 20 US 2016/0354315 A1 F.G. 2B Patent Application Publication Dec. 8, 2016 Sheet 3 of 20 US 2016/0354315 A1 F.G. 3 Patent Application Publication Dec. 8, 2016 Sheet 4 of 20 US 2016/0354315 A1 Patent Application Publication Dec. -

CHRONIC MEDICATION COMPREHENSIVE FORMULARY Effective 1 June 2013
CHRONIC MEDICATION COMPREHENSIVE FORMULARY Effective 1 June 2013 This formulary represents drugs covered for chronic use for 25 Chronic Disease List (CDL) conditions and individual Diagnosis and Treatment Pairs (DTP) conditions. Reimbursement of medicines for non-CDL and non-DTP conditions is subject to Scheme Rules and the Metropolitan Health Risk Management Medicine Reimbursement Policy. Unless stipulated, all active ingredients listed in this formulary are subject to the Metropolitan Health Reference Price (MetRef). The examples below serve as a guide on the trade names available for the active ingredients listed and not for marketing a specific brand. Any product within the MetRef category may be used, however a co-payment may be attracted if the product selected is above the generic reference threshold. The dispensing pharmacist may make a generic substitution to assist members in avoiding a co-payment. Treatment designated as "Accepted treatment" indicates that this is a medicine covered as first line, according to the Metropolitan Health Risk Management Medicine Reimbursement Policy. For treatment designated as "Motivation required", certain criteria as specified in the Metropolitan Health Risk Management Medicine Reimbursement Policy should be met. For treatment designated as "Special investigation", the relevant clinical investigation reports as specified in the Metropolitan Health Risk Management Medicine Reimbursement Policy are required. Abbreviations of dosage form CAP Capsule ENE Enema OPD Eye drops CPS Capsule -
Treatments for Atopic Eczema
Health Technology Assessment 2000; Vol. 4: No. 37 Review Systematic review of treatments for atopic eczema C Hoare A Li Wan Po H Williams Health Technology Assessment NHS R&D HTA Programme HTA HTA How to obtain copies of this and other HTA Programme reports. An electronic version of this publication, in Adobe Acrobat format, is available for downloading free of charge for personal use from the HTA website (http://www.hta.ac.uk). A fully searchable CD-ROM is also available (see below). Printed copies of HTA monographs cost £20 each (post and packing free in the UK) to both public and private sector purchasers from our Despatch Agents. Non-UK purchasers will have to pay a small fee for post and packing. For European countries the cost is £2 per monograph and for the rest of the world £3 per monograph. You can order HTA monographs from our Despatch Agents: – fax (with credit card or official purchase order) – post (with credit card or official purchase order or cheque) – phone during office hours (credit card only). Additionally the HTA website allows you either to pay securely by credit card or to print out your order and then post or fax it. Contact details are as follows: HTA Despatch Email: [email protected] c/o Direct Mail Works Ltd Tel: 02392 492 000 4 Oakwood Business Centre Fax: 02392 478 555 Downley, HAVANT PO9 2NP, UK Fax from outside the UK: +44 2392 478 555 NHS libraries can subscribe free of charge. Public libraries can subscribe at a very reduced cost of £100 for each volume (normally comprising 30–40 titles). -

Medicines (Prescription Only) (Jersey) Order 1997
MEDICINES (PRESCRIPTION ONLY) (JERSEY) ORDER 1997 Revised Edition 20.625.95 Showing the law as at 1 January 2019 This is a revised edition of the law Medicines (Prescription Only) (Jersey) Order 1997 Arrangement MEDICINES (PRESCRIPTION ONLY) (JERSEY) ORDER 1997 Arrangement Article 1 Interpretation ................................................................................................... 5 2 Prescription only medicines ............................................................................ 7 3 Medicinal products that are not prescription only medicines ......................... 8 4 New medicinal products ................................................................................. 9 5 Appropriate practitioner .................................................................................. 9 6 Conditions for prescriptions relating to sale and supply ................................. 9 6A Conditions for prescriptions – administration ............................................... 11 7 Exemption for highly diluted medicinal products ........................................ 11 8 Exemptions for specified categories of persons ............................................ 11 9 Exemption for emergency sale or supply...................................................... 12 10 Exemption for sale or supply in hospitals or the prison................................ 14 11 Exemption for authorised needle supply services ......................................... 14 12 Exemption for sale or supply in cases involving another’s default -

Patient Information for Seborrheic Dermatitis in Infant/Neonate/Child/Adult
Patient Information for Seborrheic dermatitis in Infant/Neonate/Child/Adult Overview Seborrheic dermatitis, also known as seborrhea, is a common non-contagious condition of skin areas rich in oil glands (the face, scalp, and upper trunk). Seborrheic dermatitis is marked by flaking (overproduction and sloughing of skin cells) and sometimes redness and itching of the skin. It can vary in severity from mild dandruff of the scalp to scaly red patches on the skin. The normal skin yeast, Pityrosporum ovale, lives in oil-rich skin regions and plays a role in this disorder; the changes seen in the skin are due to the body's inflammatory response to the yeast found on the skin. Seborrheic dermatitis seems to worsen with stress, winter, and infrequent shampooing. Although there is no "cure" for seborrheic dermatitis, control is usually possible with medicated shampoos and topical steroid solutions, if inflammation is prominent. Who′s At Risk Dandruff occurs in 15–20% of the population, and seborrheic dermatitis (with redness and flaking) occurs in 3–5%. The problem affects all races and may be a bit worse in men. It typically starts after puberty (although babies have a version called cradle cap). Seborrheic dermatitis peaks around the age of 40 and then may improve. Severe seborrheic dermatitis is seen frequently in people with Parkinson disease, central nervous system problems, and HIV infection. Signs & Symptoms • The scalp is itchy and sheds white, oily skin flakes. • One or more of the following areas has patches of red, scaly skin: the scalp, hairline, forehead, eyebrows, eyelids, creases of the nose and ears, ear canals, beard area, breastbone, midback, groin, or armpits. -

(12) Patent Application Publication (10) Pub. No.: US 2016/0022579 A1 Siegfried (43) Pub
US 20160022579A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2016/0022579 A1 Siegfried (43) Pub. Date: Jan. 28, 2016 (54) LIQUID COMPOSITIONS CAPABLE OF A619/00 (2006.01) FOAMING AND INCLUDING ACTIVE A63L/96 (2006.01) AGENTS, AND METHODS FOR MAKING OR A613 L/474 (2006.01) DEVELOPNG SAME A613 L/7048 (2006.01) A63L/92 (2006.01) (71) Applicant: MIKA Pharma GmbH A 6LX3/573 (2006.01) (52) U.S. Cl. (72) Inventor: Bernd G. Siegfried, Limburgerhof (DE) CPC ............... A61K 9/122 (2013.01); A61 K31/192 (2013.01); A61 K3I/I67 (2013.01); A61 K (21) Appl. No.: 14/633,929 31/573 (2013.01); A61K 31/196 (2013.01); A61K 31/4174 (2013.01); A61 K3I/7048 (22) Filed: Feb. 27, 2015 (2013.01); A61 K9/0014 (2013.01) Related U.S. Application Data (57) ABSTRACT (63) Continuation of application No. 12/838.737, filed on A liquid composition Suitable for topical use comprising is Jul. 19, 2010, now Pat. No. 9,005,626. provided that includes a phospholipid foaming agent and at least one solvent; and a pharmaceutically acceptable active (30) Foreign Application Priority Data agent; wherein the liquid composition is capable of mechani cally foaming without an additional propellant; and wherein Jul. 24, 2009 (DE) ..................... 10-2009-034-603.1 upon mechanical foaming of 250 ml of the liquid composition results in a foam with a foam Volume of at least about 400 ml Publication Classification and a foam stability wherein at least about 50% of the foam volume is still present after about 5 minutes at 25° C., as (51) Int. -
PDF (Guidelines for ATC Classification and DDD Assignment)
Guidelines for ATC classification and DDD assignment 2018 ISSN 1726-4898 ISBN 978-82-8082-896-5 Suggested citation: WHO Collaborating Centre for Drug Statistics Methodology, Guidelines for ATC classification and DDD assignment 2018. Oslo, Norway, 2017. © Copyright WHO Collaborating Centre for Drug Statistics Methodology, Oslo, Norway. Use of all or parts of the material requires reference to the WHO Collaborating Centre for Drug Statistics Methodology. Copying and distribution for commercial purposes is not allowed. Changing or manipulating the material is not allowed. Guidelines for ATC classification and DDD assignment 21st edition WHO Collaborating Centre for Drug Statistics Methodology Norwegian Institute of Public Health P.O.Box 4404 Nydalen N-0403 Oslo Norway Telephone: (47) 21078160 E-mail: [email protected] Website: www.whocc.no Previous editions: 1990: Guidelines for ATC classification1) 1991: Guidelines for DDD1) 1993: Guidelines for ATC classification 1993: Guidelines for DDD 1996: Guidelines for ATC classification and DDD assignment 1998: Guidelines for ATC classification and DDD assignment 2000: Guidelines for ATC classification and DDD assignment 2001: Guidelines for ATC classification and DDD assignment 2002: Guidelines for ATC classification and DDD assignment 2003: Guidelines for ATC classification and DDD assignment 2004: Guidelines for ATC classification and DDD assignment 2005: Guidelines for ATC classification and DDD assignment 2006: Guidelines for ATC classification and DDD assignment 2007: Guidelines for ATC classification