T2 R1.5 Femoral Nailing System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Federal Register/Vol. 83, No. 150/Friday, August 3, 2018/Notices
Federal Register / Vol. 83, No. 150 / Friday, August 3, 2018 / Notices 38161 Community Community map repository address Canadian County, Oklahoma and Incorporated Areas Project: 12–06–1030S Preliminary Date: February 8, 2018 City of El Reno ......................................................................................... Municipal Building, 101 North Choctaw Avenue, El Reno, OK 73036. Aransas County, Texas and Incorporated Areas Project: 15–06–0811S Preliminary Date: March 16, 2018 City of Aransas Pass ................................................................................ City Hall, 600 West Cleveland Boulevard, Aransas Pass, TX 78336. San Patricio County, Texas and Incorporated Areas Project: 15–06–0811S Preliminary Date: March 16, 2018 City of Aransas Pass ................................................................................ City Hall, 600 West Cleveland Boulevard, Aransas Pass, TX 78336. [FR Doc. 2018–16666 Filed 8–2–18; 8:45 am] 97.048, Disaster Housing Assistance to Brown Fund; 97.032, Crisis Counseling; BILLING CODE 9110–12–P Individuals and Households In Presidentially 97.033, Disaster Legal Services; 97.034, Declared Disaster Areas; 97.049, Disaster Unemployment Assistance (DUA); Presidentially Declared Disaster Assistance— 97.046, Fire Management Assistance Grant; DEPARTMENT OF HOMELAND Disaster Housing Operations for Individuals 97.048, Disaster Housing Assistance to and Households; 97.050, Presidentially Individuals and Households In Presidentially SECURITY Declared Disaster Assistance to Individuals -

An Early Turning Point in the History of the Crusades
Jonathan Phillips. The Second Crusade: Extending the Frontiers of Christendom. New Haven: Yale University Press, 2007. xxix + 364 pp. $40.00, cloth, ISBN 978-0-300-11274-0. Reviewed by Jonathan R. Lyon Published on H-German (March, 2008) As the author makes clear in the excellent in‐ cepts could be employed against a variety of Latin troduction to this work, the Second Crusade Christendom's enemies. (1145-49) has typically not attracted as much in‐ Phillips divides his work into fourteen terest from modern historians as the more fa‐ chronologically-arranged chapters, although sepa‐ mous First Crusade (1095-99) and Third Crusade rate chapters treat the Iberian and Baltic compo‐ (1188-92). A key explanation for this trend is the nents of the crusade. The frst two chapters dis‐ Second Crusade's failure to make any significant cuss the period between the First and the Second gains for the Christians of the Holy Land in the Crusade; chapter 1 focuses on the various pilgrim‐ wake of the Muslim conquest of Edessa in 1144. ages and crusading efforts of the early twelfth Nevertheless, as Phillips convincingly argues, this century, and chapter 2 provides a rich, fascinating crusade--despite its lack of success--demands discussion of the powerful legacy the First Cru‐ more attention than it has received for several sade left to Latin Christian culture in the decades reasons. It was the frst crusade to the Holy Land after 1099. Phillips persuasively argues that this to involve western European kings and thus legacy had a significant impact on recruiting for forced rulers to consider the consequences of the Second Crusade, because the generation of leaving their kingdoms for months (if not years) young nobles alive in the 1140s had grown up at a time. -

Medieval Heritage and Pilgrimage Walks
Medieval Heritage and Pilgrimage Walks Cleveland Way Trail: walk the 3 miles from Rievaulx Abbey, Yorkshire to Helmsley Castle and tread in the footsteps of medieval Pilgrims along what’s now part of the Cleveland Way Trail. Camino de Santiago/Way of St James, Spain: along with trips to the Holy Land and Rome, this is the most famous medieval pilgrimage trail of all, and the most well-travelled in medieval times, at least until the advent of Black Death. Its destination point is the spot St James is said to have been buried, in the Cathedral of Santiago de Compostela. Today Santiago is one of UNESCO’s World Heritage sites. Read more . the Cathedral of Santiago de Compostela holds a Pilgrims’ Mass every day at noon. Walk as much or as little of it as you like. Follow the famous scallop shell symbols. A popular starting point, both today and in the Middle Ages, is either Le Puy in the Massif Central, France OR the famous medieval Abbey at Cluny, near Paris. The Spanish start is from the Pyrenees, on to Roncevalles or Jaca. These routes also take in the Via Regia and/or the Camino Frances. The Portuguese way is also popular: from the Cathedrals in either Lisbon or Porto and then crossing into Falicia/Valenca. At the end of the walk you receive a stamped certifi cate, the Compostela. To achieve this you must have walked at least 100km or cycled for 200. To walk the entire route may take months. Read more . The route has inspired many TV and fi lm productions, such as Simon Reeve’s BBC2 ‘Pilgrimage’ series (2013) and The Way (2010), written and directed by Emilio Estevez, about a father completing the pilgrimage in memory of his son who died along the Way of St James. -

Personal Names and Denomination of Livonians in Early Written Sources
ESUKA – JEFUL 2014, 5–1: 13–26 PERSONAL NAMES AND DENOMINATION OF LIVONIANS IN EARLY WRITTEN SOURCES Enn Ernits Estonian University of Life Sciences Abstract. This paper presents the timeline of ethnonyms denoting Livonians; specifies their chronology; and analyses the names used for this ethnos and possible personal names. If we consider the dating of the event, the earliest sources mentioning Livonians are Gesta Danorum and the Tale of Bygone Years (both 10th century), but both sources present rather dubious information: in the first the battle of Bråvalla itself or the date are dubious (6th, 8th or 10th century); in the latter we cannot be sure that the member of the Rus delegation was really a Livonian. If we consider the time of recording, the earliest sources are two rune inscriptions from Sweden (11th century), and the next is the list of neighbouring peoples of the Russians from the Tale of Bygone Years (12th century). The personal names Bicco and Ger referred in Gesta Danorum, and Либи Аръфастовъ in Tale of Bygone Years are very problematic. The first certain personal name of a Livonian is *Mustakka, *Mustukka or *Mustoikka (from Finnic *musta ‘black’) written in 1040–1050s on a strip of birch bark in Novgorod. Keywords: Livs, Finnic peoples, ethnonyms, anthroponyms, onomastics DOI: http://dx.doi.org/10.12697/jeful.2014.5.1.01 1. Introduction This paper (1) seeks to present the timeline of ethnonyms denoting Livonians; (2) to specify their chronology; (3) and to analyse the names used for this ethnos and possible personal names. It is supple- mental to the paper by Mauno Koski on words denoting Livonians (Koski 2011). -
Charters: What Survives?
Banner 4-final.qxp_Layout 1 01/11/2016 09:29 Page 1 Charters: what survives? Charters are our main source for twelh- and thirteenth-century Scotland. Most surviving charters were written for monasteries, which had many properties and privileges and gained considerable expertise in preserving their charters. However, many collections were lost when monasteries declined aer the Reformation (1560) and their lands passed to lay lords. Only 27% of Scottish charters from 1100–1250 survive as original single sheets of parchment; even fewer still have their seal attached. e remaining 73% exist only as later copies. Survival of charter collectionS (relating to 1100–1250) GEOGRAPHICAL SPREAD from inStitutionS founded by 1250 Our picture of documents in this period is geographically distorted. Some regions have no institutions with surviving charter collections, even as copies (like Galloway). Others had few if any monasteries, and so lacked large charter collections in the first place (like Caithness). Others are relatively well represented (like Fife). Survives Lost or unknown number of Surviving charterS CHRONOLOGICAL SPREAD (by earliest possible decade of creation) 400 Despite losses, the surviving documents point to a gradual increase Copies Originals in their use in the twelh century. 300 200 100 0 109 0s 110 0s 111 0s 112 0s 113 0s 114 0s 115 0s 116 0s 1170s 118 0s 119 0s 120 0s 121 0s 122 0s 123 0s 124 0s TYPES OF DONOR typeS of donor – Example of Melrose Abbey’s Charters It was common for monasteries to seek charters from those in Lay Lords Kings positions of authority in the kingdom: lay lords, kings and bishops. -

A File in the Online Version of the Kouroo Contexture (Approximately
SETTING THE SCENE FOR THOREAU’S POEM: YET AGAIN WE ATTEMPT TO LIVE AS ADAM 11th Century 1010s 1020s 1030s 1040s 1050s 1060s 1070s 1080s 1090s 12th Century 1110s 1120s 1130s 1140s 1150s 1160s 1170s 1180s 1190s 13th Century 1210s 1220s 1230s 1240s 1250s 1260s 1270s 1280s 1290s 14th Century 1310s 1320s 1330s 1340s 1350s 1360s 1370s 1380s 1390s 15th Century 1410s 1420s 1430s 1440s 1450s 1460s 1470s 1480s 1490s 16th Century 1510s 1520s 1530s 1540s 1550s 1560s 1570s 1580s 1590s 17th Century 1610s 1620s 1630s 1640s 1650s 1660s 1670s 1680s 1690s 18th Century 1710s 1720s 1730s 1740s 1750s 1760s 1770s 1780s 1790s 19th Century 1810s Alas! how little does the memory of these human inhabitants enhance the beauty of the landscape! Again, perhaps, Nature will try, with me for a first settler, and my house raised last spring to be the oldest in the hamlet. To be a Christian is to be Christ- like. VAUDÈS OF LYON 1600 William Gilbert, court physician to Queen Elizabeth, described the earth’s magnetism in DE MAGNETE. Robert Cawdrey’s A TREASURIE OR STORE-HOUSE OF SIMILES. Lord Mountjoy assumed control of Crown forces, garrisoned Ireland, and destroyed food stocks. O’Neill asked for help from Spain. HDT WHAT? INDEX 1600 1600 In about this year Robert Dudley, being interested in stories he had heard about the bottomlessness of Eldon Hole in Derbyshire, thought to test the matter. George Bradley, a serf, was lowered on the end of a lengthy rope. Dudley’s little experiment with another man’s existence did not result in the establishment of the fact that holes in the ground indeed did have bottoms; instead it became itself a source of legend as spinners would elaborate a just-so story according to which serf George was raving mad when hauled back to the surface, with hair turned white, and a few days later would succumb to the shock of it all. -

VWR Circulators and Chillers
VWR Circulators and Chillers Superior Temperature Control Equipment Clockwise from top left: 13721-200, 13721-172, 13721-138, 13721-082 Controllers Table of Contents. Page Product Features. 2-3 Precise Controllers Controllers . 4-5 Choice of four controllers. From state-of-the-art program- VWR Signature` mable designs that provide Refrigerated/Heating ultimate control, to the analog Circulating Baths. 6-10 design that is perfect for less demanding applications. How To Choose A Chiller . 11 VWR Signature Recirculating Chillers . 12-13 VWR Signature Heating Immersion Circulator. 14 Durable Design VWR` Open Bath Systems . 15 Immersed parts and reservoirs are made of corrosion-fighting VWR Signature stainless steel. The exterior Heating Circulating Baths . 16-17 surface is a tough powder coating for easy clean-up. VWR Refrigerated/Heating Circulating Baths. 18-21 VWR Immersion & Flow-Through Coolers . 22 VWR Ambient Bath Cooler. 22 Double Safety VWR Heating Recirculator . 22 Your equipment and work are protected with redundant over VWR Heating Immersion Circulators . 23 temperature and low liquid cutoff standard on all circula- VWR Heating Circulating Baths . 24-25 tors. 60Hz models are CSA approved, 50Hz models carry Accessories . 26 the CE mark. At-a-Glance Chart . 27 Environmentally Responsible VWR Refrigerated Circulators and Chillers use R-134a refrigerant, and no ozone- depleting CFC’s are used in the manufacturing process. All instruments are manufactured in an ISO 9001 accredited facility. 2 To order, call 1-800-932-5000 or visit vwr.com Controllers Time Savers Advanced refrigeration sys- tems and high wattage heaters respond quickly to temperature changes. You'll have minimum waiting time for your circulator to stabilize. -

(19) United States (12) Patent Application Publication (10) Pub
US 20040245547A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2004/0245547 A1 Stipe (43) Pub. Date: Dec. 9, 2004 (54) ULTRA LOW-COST SOLID-STATE MEMORY Publication Classi?cation (75) Inventor; Barry Cushing Stipe, San Jose, CA (51) Int. Cl.7 ................................................ .. H01L 31/109 (Us) (52) US. Cl. ............................................................ .. 257/200 Correspondence Address: (57) ABSTRACT JOSEPH P. CURTIN . A three-dimensional solid-state memory is formed from a plurality of bit lines, a plurality of layers, a plurality of tree ’ structures and a plurality of plate lines. Bit lines extend in a (73) A551 nee, Hitachi Global Stora e Technolo ies ?rst direction in a ?rst plane. Each layer includes an array of g ' B V AZ Amsterdam g memory cells, such as ferroelectric or hysteretic-resistor ' " memory cells. Each tree structure corresponds to a bit line, (21) APPL NO: 10/751 740 has a trunk portion and at least one branch portion. The trunk ’ portion of each tree structure extends from a corresponding (22) Filed; Jam 5, 2004 bit line, and each tree structure corresponds to a plurality of layers. Each branch portion corresponds to at least one layer Related US, Application Data and extends from the trunk portion of a tree structure. Plate lines correspond to at least one layer and overlap the branch (63) Continuation-in-part of application No. 10/453,137, portion of each tree structure in at least one roW of tree ?led on Jun. 3, 2003, noW abandoned. structures at a plurality of intersection regions. SRIIIIII DRAM HIIIJ FLASH PROBE GUM MTJ-MRAM 3D-MHAM MATRIX ITFBRIIM GT FERAM 001 size 50F? 012 512 502 502 5F? 002 5e? 512 002 502 Minimum "1" 100m 300m 100m 30 0m 311m 100m 40 nm 400m 10 nm 100m 100m MEX. -
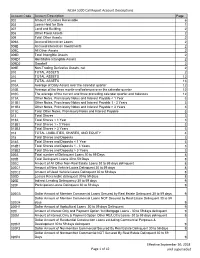
NCUA 5300 Call Report Account Descriptions Page 1 of 42 Effective
NCUA 5300 Call Report Account Descriptions Account Code Account Description Page 002 Amount of Leases Receivable 6 003 Loans Held for Sale 1 007 Land and Building 2 008 Other Fixed Assets 2 009 Total Other Assets 2 009A Accrued Interest on Loans 2 009B Accrued Interest on Investments 2 009C All Other Assets 2 009D Total Intangible Assets 2 009D1 Identifiable Intangible Assets 2 009D2 Goodwill 2 009E Non-Trading Derivative Assets, net 2 010 TOTAL ASSETS 2 010 TOTAL ASSETS 12 010 TOTAL ASSETS 13 010A Average of Daily Assets over the calendar quarter 12 010B Average of the three month-end balances over the calendar quarter 12 010C The average of the current and three preceding calendar quarter-end balances 12 011A Other Notes, Promissory Notes and Interest Payable < 1 Year 3 011B1 Other Notes, Promissory Notes and Interest Payable 1 - 3 Years 3 011B2 Other Notes, Promissory Notes and Interest Payable > 3 Years 3 011C Total Other Notes, Promissory Notes and Interest Payable 3 013 Total Shares 3 013A Total Shares < 1 Year 3 013B1 Total Shares 1 - 3 Years 3 013B2 Total Shares > 3 Years 3 014 TOTAL LIABILITIES, SHARES, AND EQUITY 4 018 Total Shares and Deposits 3 018A Total Shares and Deposits < 1 Year 3 018B1 Total Shares and Deposits 1 - 3 Years 3 018B2 Total Shares and Deposits > 3 Years 3 020A Total number of Delinquent Loans 30 to 59 Days 8 020B Total Delinquent Loans 30 to 59 Days 8 020C Amount of All Other Non-Real Estate Loans 30 to 59 days delinquent 8 020C1 Amount of New Vehicle Loans Delinquent 30 to 59 days 8 020C2 Amount of Used -

Electric Actuators Vsi-1000 Series
ELECTRIC ACTUATORS TM VSI-1000 SERIES DESCRIPTION VSI-1000 Series Electric Actuators are used on Kele KBV Series butterfly valves to provide two-position (with or without battery backup) or proportional control in a NEMA 4X housing. The VSI-1000 Series comes standard on 8" and larger non-spring return assemblies and on 5" and larger two- position spring return assemblies. They can be ordered on smaller valve assemblies as an option. Standard fea- tures include 2 SPDT fully adjustable auxiliary switches KBV-2-6-E2SO (two-position only), manual override crank, and an inter- assembly includes nal heater to prevent condensation in outdoor installa- VSI-BB1020 actuator tions. SPECIFICATIONS FEATURES Power 120 VAC standard •Lightweight, compact design Models 1005 to 1020 12/24 VDC optional • Two-position or modulating control Models 1005 to 1040 24 VAC optional • Two-position battery-backed models Torque range 347-17,359 in-lb • NEMA 4X watertight, corrosion-resistant housing Motor 120 VAC, 1 phase, 60 Hz; • Integral position indicator enclosed, non-ventilated, high • Space heater standard starting torque, reversible induc- • Two 1/2" conduit connections tion, Class E insulation • Detachable manual override crank Thermal overload Auto reset, embedded • Terminal strip wiring Travel limit switches Cam operated, adjustable SPDT • Worm gear drive, no electro-mechanical brake for open/close stop required • Mounting orientation in any direction Position indicator High-visibility graduated dial • 4-20 mA or 500Ω optional feedback signal Conduit connections -

Hildegard Transfigured – Programme Copy 2021(1)
Hildegard Transfigured: a medieval trance for the 21st century Hildegard Transfigured is a collaborative piece of concert-theatre by vocal trio Voice, visual artist Innerstrings, and composer Laura Moody that celebrates St. Hildegard of Bingen through song, psychedelic lights, and live visuals. The performance at SJE includes the world premiere of Moody’s Hildegard Portraits. St Hildegard of Bingen (1098 - 1179) joined the monastery in Disibodenberg (in German Rhineland) when she was just eight years old and would stay there for nearly forty years, eventually becoming abbess in 1136. She founded her own abbey at Rupertsberg near Bingen in 1147 and a second monastery in nearby Eibingen in 1165. Throughout her life, Hildegard was a great spiritual leader, theologian, mystic, scientist, and composer. Revered as a saint for centuries, Pope Benedict XVI canonised Hildegard of Bingen on 10 May 2012. Hildegard experienced intense visions, recorded in her major work Scivias (Know the Way), (1141-51), and it is this aspect of her life that the collaboration with visual artist, Innerstrings, will bring to life in Hildegard Transfigured, transfiguring her beautiful music into a new sensory experience. Laura Moody’s research for the show brought her to The Personal Correspondence of Hildegard of Bingen, translated by Joseph L Baird and Radd K Ehrman (OUP 2006). She has set extracts and fragments of Hildegard’s letters in her composition Hildegard Portraits, written especially for this programme. You will hear Moody's music interspersed throughout in the form of miniatures, culminating in the finale The Living Light. “It is some kind of miracle to have the kind of access to a female creator of the twelfth century that we have with Hildegard, her output only having been permissible during her lifetime because of her sacred status. -

Attempts at Geopolitical Restauration
Chapter 4 Attempts at Geopolitical Restauration Apart from aspects of the empire’s internal politics (imperial ideology, divi- sions within the Constantinopolitan court elite, problematic imperial- Venetian relations) our astrological corpus also contains information regarding Baldwin ii’s foreign politics, especially on relations with the Castilian court. The estab- lished view on the Latin empire’s geopolitical position within the Byzantine region (Balkan, Aegean, Asia Minor) under Baldwin ii is that Constantinople and its dependencies were waiting to fall into the hands of the Nicaean em- peror comme un fruit mûr, as Jean Longnon has so eloquently put it: a pas- sive existence with an inevitable outcome.1 This, however, negates the fact that on the diplomatic level the emperor and his entourage in the 1240s and 1250s continued developing one project after another with a range of international partners with the aim at maintaining and ultimately restoring his empire: the 1237–1240 crusade (with papal support), the alliance with Konya in the early 1240s, the Cuman alliance in the 1240s, the diplomatic relations with the Mon- gols in the 1240s and 1250s (which appear to have inaugurated a “Black Sea policy,” as John Giebfried has suggested, although this presumably was pre- dominantly a Venetian attempt to dominate trade in the region), the project involving the Order of Santiago in 1245–1246 (again with papal support), the 1248 campaign in the Constantinopolitan region, the re-establishment of a more active imperial policy vis-à-vis the Latin Orient (Cyprus and Syria- Palestine) in the context of the Seventh Crusade (1248–1254), a possible mar- riage alliance with Trebizond in the 1250s (with the French king Louis ix mediating), and the “grand alliance” between Achaia, Epiros, Sicily, and Con- stantinople in 1257/58–1259.2 This dynamic diplomacy—although not always 1 Longnon, L’empire latin de Constantinople, 186.