Sickle Cell Anemia Dictionary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

AHMED H. ZEWAIL 26 February 1946 . 2 August 2016
AHMED H. ZEWAIL 26 february 1946 . 2 august 2016 PROCEEDINGS OF THE AMERICAN PHILOSOPHICAL SOCIETY VOL. 162, NO. 2, JUNE 2018 biographical memoirs t is often proclaimed that a stylist is someone who does and says things in memorable ways. From an analysis of his experimental Iprowess, his written contributions, his lectures, and even from the details of the illustrations he used in his published papers or during his lectures to scientific and other audiences, Ahmed Zewail, by this or any other definition, was a stylist par excellence. For more than a quarter of a century, I interacted with Ahmed (and members of his family) very regularly. Sometimes he and I spoke several times a week during long-distance calls. Despite our totally different backgrounds we became the strongest of friends, and we got on with one another like the proverbial house on fire. We collaborated scientifi- cally and we adjudicated one another’s work, as well as that of others. We frequently exchanged culturally interesting stories. We each relished the challenge of delivering popular lectures. In common with very many others, I deem him to be unforgettable, for a variety of different reasons. He was one of the intellectually ablest persons that I have ever met. He possessed elemental energy. He executed a succession of brilliant experiments. And, almost single-handedly, he created the subject of femtochemistry, with all its magnificent manifestations and ramifications. From the time we first began to exchange ideas, I felt a growing affinity for his personality and attitude. This was reinforced when I told him that, ever since I was a teenager, I had developed a deep interest in Egyptology and a love for modern Egypt. -

Mosher History
VI. PROFESSORS, BRIEF BIOGRAPHICAL SUMMARIES 1976-2000 These brief biographical summaries, listed in the order of their appointments to the faculty, are not intended to be complete and will of course become out of date after the year 2000. The reader is referred to contemporary volumes of American Men and Women of Science for more information and to the ACS Directory of Graduate Research for publication lists. JAMES MURRAY LUCK. Biochem. B.S. Toronto, Ph.D. Cambridge, England, 1925. Student of J.B.S. Haldane and Sir Gowland Hopkins. Demonstrator Toronto, 1925-26; Asst. Prof. to Prof., Stanford 1926-34, Prof. 1934-65; Emeritus 1965. “1856 Exhibitor Research Scholarship”. Founding editor of Annual Reviews of Biochemistry and the many subsequent Annual Reviews Series in other fields. Fellow AAAS, Fellow Calif. Acad. Sci. Born Paris, Ontario, Canada 1898. Died Stanford 8/26/1993. WILLIAM ANDREW BONNER. Org. Chem. A.B. Harvard, Ph.D. Northwestern, 1944. Student of C.D. Hurd. Instr. to Prof., Stanford 1946-59, Prof. 1959-83, Emeritus 1983. Guggenheim Fellow ETH, Zurich, Switzerland 1953. Born Chicago 1919. RICHARD HALLENBECK EASTMAN. Org. Chem. A.B. Princeton, Ph.D. Harvard, 1944. Student of R.B. Woodward. Asst. Harvard 1944-46; Instr. to Prof., Stanford 1946-59; Prof. 1959-83, Emeritus 1983. NSF Fellow, U. Marburg 1958-59. Born Erie, PA 1918. Died Stanford 6/18/2000. HARRY STONE MOSHER. Org. Chem. A.B. Willamette U., M.S. Ore. State Coll., Ph.D. Penn. State Coll. 1942. Student of F.C. Whitmore. Asst. Prof. Willamette 1939-40; Penn. State Coll.1942-47; Asst. -

Novdec2011.Pdf 2375 KB
SCALACS Website address: www.scalacs.org November/December 2011 A Joint Publication of the Southern California and San Gorgonio Sections of the American Chemical Society Southern California Section Hosts the Western Regional Meeting at the Westin in Pasadena November 10-12, 2011 100 Years of Outstanding Chemistry in Southern California! Centennial Banquet November 11, 2011 See Page 3 San Gorgonio Section 2011 SCC Undergraduate Research Conference Saturday, November 19, 2011 Mount San Antonio College See Page 15 SCALACS A Joint Publication of the Southern Cal ifornia and San Gorgonio Sections of the American Chemical Society Volume LXIV November/December 2011 Number 7 TABLE OF CONTENTS SOUTHERN CALIFORNIA SECTION 2011 OFFICERS So. Cal. Chair’s Message 2 Chair: Joe Khoury So. Cal. Meeting & WR Notice 3-6 Chair Elect: Bob de Groot Congratulations Jackie Barton! 7 Secretary: Aleksandr Pikelny Treasurer: Barbara Belmont Thank You Volunteers! 8-9 Councilors: Rita Boggs, Bob de Call for Nominations—Tolman Groot, Herb Kaesz, Tom LeBon, Eleanor Siebert, Barbara SItzman Award 10 Call for Nominations—Teacher of the SAN GORGONIO SECTION Year 11 2011 OFFICERS This Month in Chemical History 12-13 Chair: Eileen DiMauro S. G. Chair’s Message 14 Chair-Elect: Kathy Swartout S. G. Meeting Notice 15 Secretary: David Srulevitch P. O. Statement of Ownership 16 Treasurer Dennis Pederson Councilors: Jim Hammond, Ernie Index to Advertisers 17 Simpson Chemists’ Calendar bc SCALACS (ISSN) 0044-7595 is published monthly March through May, September and October; and Bi-monthly January/February and November/December along with a special ballot issue once a year. Published by the Southern California Section of the American Chemical Society at 14934 South Figueroa Street, Gardena CA 90248. -

ACS Scholars Developing Leaders by Mindy Levine by Stefan Koenig ACS Scholars
DED UN 18 O 98 F http://www.nesacs.org N Y O T R E I T H C E N O A E S S S L T A E A C R C I N S M S E E H C C TI N O CA April 2010 Vol. LXXXVIII, No. 8 N • AMERI Monthly Meeting Summer Scholar Report Esselen Award Meeting at Harvard By Elizabeth Neuhardt, Keene State College Award to Stephen L. Buchwald of MIT ACS Scholars Developing Leaders By Mindy Levine By Stefan Koenig ACS Scholars By Mindy Levine, Massachusetts Institute of Technology, Department of Chemistry, Cambridge, MA 02139 Shaymus Hudson is a self-proclaimed wise inaccessible. Merricka Living- $1,000-$5,000 per year. Students, who science nerd. Growing up, he watched stone was planning on attending the are selected either during their senior “Bill Nye the Science Guy” on televi- University of Florida. Alden Williams year of high school or during college, sion. He studied math and science at a thought she would go to Columbia major in a chemistry-related field - for Governor’s School for Science and University. Thanks in part to the ACS example, chemistry, chemical engi- Technology in rural Virginia, and did a Scholars program, both of them are neering or biochemistry. science project at a local community currently freshmen at MIT. “I really Funding Sources college during his junior year of high appreciate being here, and the opportu- The majority of the funding for the school. When it was time for him to nities I have,” Ms. -

Erick Carreira
Meet the Editor POB3 2021 – 30.03.2021 POB3: Materiały Przyszłości Godzina Prelegent dr hab. inż. Przemysław Data, prof. PŚ 12:00 – 12:05 Rozpoczęcie e-konferencji POB3: Materiały przyszłości. Wprowadzenie Spotkanie z edytorem Journal of the American Chemical Society (Top 1) Meeting with the Journal of the American Chemical Society editor (Top 1) Writing for Impact 12:05 - 12:35 Erick Carreira JACS, Editor in Chief Dyskusja Q&A 12:35 - 13:00 Zakończenie e-konferencji. Moderator: Dr hab. inż. Przemysław Data, prof. PŚ Erick Carreira https://orcid.org/0000-0003-1472-490X https://carreira.ethz.ch/ Professor Carreira was born in Havana, Cuba in 1963. He obtained a B.S. degree in 1984 from the University of Illinois at Urbana-Champaign under the supervision of Scott E. Denmark and a Ph.D. degree in 1990 from Harvard University under the supervision of David A. Evans. After carrying out postdoctoral work with Peter Dervan at the California Institute of Technology through late 1992, he joined the faculty at the same institution as an assistant professor of chemistry and subsequently was promoted to 1 Meet the Editor POB3 2021 – 30.03.2021 POB3: Materiały Przyszłości the rank of associate professor of chemistry in the Spring of 1996, and full Professor in Spring 1997. He then moved to ETH Zürich, Switzerland as a full professor in 1998. Professor Carreira is a member of both the U.S. National Academy of Sciences and the American Academy of Arts and Sciences. He is the recipient of the Kharasch Lectureship (University of Chicago), Barluenga Lectureship (Royal Spanish Chemical Society), C. -
Phillip Sharp
Previous N. J. Leonard Lecturers 1986-1987 James P. Collman Stanford University 1987-1988 Sir Derek H. R. Barton Texas A&M University 1988-1989 Christopher T. Walsh Harvard Medical School 1989-1990 Donald J. Cram University of California, Los Angeles 1990-1991 Richard R. Ernst Eidgenossische Technische Hochschule, Zürich 1991-1992 Thomas A. Steitz Yale University 1992-1993 K. Barry Sharpless Scripps Research Institute 1993-1994 Rudolph A. Marcus California Institute of Technology GUEST 1994-1995 Phillip A. Sharp Massachusetts Institute of Technology 1995-1996 Martin Rodbell National Institute for Environmental Health Sciences SPEAKERs 1996-1997 John D. Roberts California Institute of Technology Sidney M. Hecht University of Virginia Peter G. Schultz University of California, Berkeley Thomas Carell Ludwig -Maxmilians universität Albert Eschenmoser Eidgenössische Technische Hochschule, Zürich DNA Beyond Watson and Crick 1997-1998 F. Sherwood Rowland University of California, Irvine 1998-1999 Jean-Michel Savéant Centre National de la Recherche Scientifique 1999-2000 David A. Tirrell California Institute of Technology Marvin Caruthers university of colorado 2000-2001 Alastair Ian Scott Texas A&M University Chemical and Biological Activity 2001-2002 Amos B. Smith III University of Pennsylvania of New Synthetic DNA Analogues 2002-2003 Lawrence J. Marnett Vanderbilt University 2003-2004 Robert S. Langer Massachusetts Institute of Technology Thomas Cech 2004-2005 Thomas R. Cech Howard Hughes Medical Institute, university of colorado University of Colorado at Boulder How a Chemist Thinks About RNA 2005-2006 Joseph M. DeSimone University of North Carolina-Chapel Hill 2006-2007 Rolf Thauer Max Planck Institute for Terrestrial Microbiology 2008-2009 Roger Y. -
Public Lecture Series Speakers: 1936 – 2019
Public Lecture Series Speakers: 1936 – 2019 The Graduate School has been fortunate to host the following speakers as part of the Public Lecture Series. Lecturers on this list are not eligible for the upcoming nomination cycle. Please contact [email protected] with any questions about the nomination process. Signature Speakers Series Menhaz Afridi Maria Hinojosa Donna Shalala Morehshin Allahyari Ralina Joseph Ellen Schur Harry Belafonte Verlaine Keith-Miller Nate Silver Carl Bergstrom Marieka Klawitter Kristen Soltis Anderson Misty Copeland Anthony Leiserowitz Touré Laverne Cox Ulf Leonhardt Jose Antonio Vargas Robin DiAngelo Sharon Maeda Jevin West Junot Díaz Trinh Mai Joy Williamson-Lott Lori Dorfman Peggy McIntosh Tim Wise Adam Drewnowski Megan Ming Francis Kevin Young Ronan Farrow Kathy Najimy Sara Zewde Larry Gossett Emile Pitre Temple Grandin Rogelio Riojas Walker-Ames Scholars Alexander Nagel Kirk Johnson Louis Nirenberg John Beverley Charles Keil Rithy Panh Peter Brewer James Lawson Valerie Smith Ming Cho Lee Samuel NC Lieu Roger Strasser Deborah Dryden Helen Longino Elizabeth Wilson Carole Gassert Philip Kumar Maini Joy James Guiseppe Mazzotta Walker-Ames Lecturers Jeno Adam James Balog George Benedek Julian Agyeman Leonard Barkan Seyla Benhabib Huda Akil George Bartholemew T. Brooke Benjamin Hans Albrecht Bethe Paul Bartlett Margaret Bent Emilio Amero George Batchelor Russell Berman Alexander Archipenko Joseph Beach Howard Bern Kenneth Bailey Hugh Beales Jagdish Bhagwati Bernard Bailyn Arnold Beckett Bhabani Bhattacharya Mieke Bal Jean-Albert Bede Garrett Birkhoff Alan Bittles Alfred Chandler, Jr. Robert Dicke J. Bjerknes Li Chi Liselotte Dieckmann Felix Bloch Brock Chisholm Jean Dieudonne Bruce Blumberg Gustave Choquet Andrea (Andy) DiSessa Larry Bobo Ralph Cicerone Stuart Dodd Christoph Bode Marion Clawson Denis Donoghue Bart Bok Cornell Clayton Sterling Dow Bert Bolin William Clebsch Curt Ducasse Paul Bonifas JM Coetzee John Dunning Gabriel Bonno Philip Cohen J. -

Johnson.Speakers to 2017.17
Johnson Symposia 1986-2018 1986 ALEXANDER KLIBANOV KONRAD BLOCH STEPHEN FODOR ALBERT ESCHENMOSER GEORGE OLAH SIR DEREK BARTON CHI-HUEY WONG JOHN D. ROBERTS REINHARD HOFFMANN GILBERT STORK BRUCE AMES WILLIAM S. JOHNSON 1995 1987 DEREK BARTON DUILIO ARIGONI RON BRESLOW STEPHEN BENKOVIC ALBERT ESCHENMOSER RONALD BRESLOW ROBERT GRUBBS E. J. COREY RALPH HIRSCHMANN GILBERT STORK GEORGE OLAH PETER DERVAN RYOJI NOYORI E. THOMAS KAISER BARRY SHARPLESS JEAN-MARIE LEHN GILBERT STORK 1988 JOHN ROBERTS SAMUEL DANISHEFSKY 1996 DUDLEY WILLIAMS MARYE ANNE FOX PAUL BARTLETT JOEL HUFF KOJI NAKANISHI ERIC JACOBSEN DUILIO ARIGONI LARRY OVERMAN JEREMY KNOWLES GEORGE PETTIT K. BARRY SHARPLESS PETER SCHULTZ DONALD CRAM GREGORY VERDINE 1989 MAXINE SINGER JACK BALDWIN 1997 A. R. BATTERSBY STEPHEN BUCHWALD DAVID EVANS CHARLES CASEY ROBERT GRUBBS STEPHEN FESIK CLAYTON HEATHCOCK M. REZA GHADIRI KOJI NAKANISHI STEPHEN HANESSIAN R. NOYORI DANIEL KAHNE CHARLES SIH MARY LOWE GOOD 1990 JOANNE STUBBE ROBERT BERGMAN 1998 THOMAS CECH KEN HOUK ROALD HOFFMANN NED PORTER STUART SCHREIBER ANDREAS PFALTZ HERBERT BROWN MAURICE BROOKHART HENRY ERLICH SEAN LANCE K. C. NICOLAOU WILLIAM FENICAL E. VOGEL SIDNEY ALTMAN 1991 DUILIO ARIGONI HARRY ALLCOCK 1999 JEROME BERSON STEVEN BOXER DALE BOGER JOHN BRAUMAN WILLIAM JORGENSEN JAMES COLLMAN RALPH RAPHAEL CARL DJERASSI PETER SCHULTZ CHAITAN KHOSLA DIETER SEEBACH BARRY TROST CHRISTOPER WALSH ROBERT WAYMOUTH 1992 THOMAS WANDLESS JACQUELINE BARTON PAUL WENDER KLAUS BIEMANN 2000 RICHARD LERNER SCOTT DENMARK MANFRED REETZ JANINE COSSY ALEJANDRO ZAFFARONI DENNIS DOUGHERTY CLARK STILL JONATHAN ELLMAN J. FRASER STODDART JERROLD MEINWALD HISASHI YAMAMOTO EI-ICHI NEGISHI 1993 MASAKATSU SHIBASAKI PAUL EHRLICH BERND GIESE LOUIS HEGEDUS 2001 STEVEN LEY ROB ARMSTRONG JULIUS REBEK JON CLARDY F. -

1:1 Motif for Dna Recognition by Β-Alanine-Linked Polyamides
1:1 MOTIF FOR DNA RECOGNITION BY β-ALANINE-LINKED POLYAMIDES Thesis by Adam Robert Urbach In Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy California Institute of Technology Pasadena, California 2002 (Submitted May 17, 2002) ii © 2002 Adam Robert Urbach All Rights Reserved iii To my Father iv Acknowledgements I would like to thank my Ph. D. advisor, Professor Peter Dervan, for giving me just the right mixture of freedom and guidance in order to pursue my interests and yet to turn my energy into useful science. The training I've received has far exceeded anything I could have imagined just a few years ago. I am particularly grateful to Professor Dervan for supporting my decision to leave Caltech during my second year and then taking me back into his group with enthusiasm and compassion. My thesis committee has taught me, among other things, the important lesson of how to better approach the writing and defending of research proposals. I am grateful to Professors Robert H. Grubbs, John D. Roberts, Richard W. Roberts, and Stephen L. Mayo for these lessons as well as helpful conversations over the years. Special thanks goes to Professor John D. Roberts for the privilege of his discerning attention during this past year. The work of Professor Uli Laemmli provided much inspiration for the theses presented here. I look to Professor Laemmli with great admiration and respect as a scientist, and I am grateful to him for advocating my work during his visit to Caltech. Much appreciation goes to Professor John Love and Dr Scott Ross for teaching me macromolecular NMR and being supportive throughout our fruitful collaboration. -
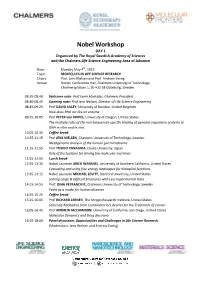
Nobel Workshop DAY 1 Organized by the Royal Swedish Academy of Sciences and the Chalmers Life Science Engineering Area of Advance
Nobel Workshop DAY 1 Organized by The Royal Swedish Academy of Sciences and the Chalmers Life Science Engineering Area of Advance Date: Monday May 4th, 2015 Topic: MOLECULES IN LIFE SCIENCE RESEARCH Chairs: Prof. Jens Nielsen and Prof. Andrew Ewing Venue: RunAn Conference Hall, Chalmers University of Technology, Chalmersplatsen 1, SE-412 58 Göteborg, Sweden 08:35-08:40 Welcome note: Prof Karin Markides, Chalmers President 08:40-08:45 Opening note: Prof Jens Nielsen, Director of Life Science Engineering 08:45-09:25 Prof DAVID LILLEY, University of Dundee, United Kingdom How does RNA act like an enzyme 09:25-10:05 Prof PETER von HIPPEL, University of Oregon, United States The multiple roles of the non-(sequence)-specific binding of genome-regulatory proteins to DNA in vitro and in vivo. 10.05-10:35 Coffee break 10:35-11:15 Prof JENS NIELSEN, Chalmers University of Technology, Sweden Metagenome analysis of the human gut microbiome 11:15-11:55 Prof TOSHIO YANAGIDA, Osaka University, Japan Role of fluctuations for driving bio-molecular machines 11:55-12:55 Lunch break 12:55-13:35 Nobel Laureate ARIEH WARSHEL, University of Southern California, United States Evaluating and using free energy landscapes for biological functions 13:35-14:15 Nobel Laureate MICHAEL LEVITT, Stanford University, United States Solving Large & Difficult Structures with Less Experimental Data 14:15-14:55 Prof. DINA PETRANOVIC, Chalmers University of Technology, Sweden Yeast as a model for human diseases 14:55-15:25 Coffee break 15:25-16:05 Prof RICHARD LERNER, The Scripps -

Interview with John D. Baldeschwieler
JOHN D. BALDESCHWIELER (Born 1933) INTERVIEWED BY SHIRLEY K. COHEN January – February, 2001 ARCHIVES CALIFORNIA INSTITUTE OF TECHNOLOGY Pasadena, California Subject area Chemistry, chemical engineering Abstract Interview in six sessions in January and February 2001 with John D. Baldeschwieler, J. Stanley Johnson Professor and professor of chemistry, emeritus, in the Division of Chemistry and Chemical Engineering. Dr. Baldeschwieler received his bachelor’s in chemical engineering from Cornell in 1956 and his PhD in 1959 from UC Berkeley. He begins by recalling his childhood and early education in Cranford, N.J. His father, an analytical chemist, emigrated from Switzerland and his mother from Manitoba. He matriculated at Cornell in 1951 and enrolled in ROTC during the Korean War. Recalls summer work at Los Alamos and graduate school at Berkeley 1956-1959; his thesis on infrared spectroscopy, with George Pimentel; interest in instrument building. After six months’ active duty at Aberdeen Proving Ground, Md., joins the Harvard faculty; becomes a consultant for Aberdeen. Early work with nuclear magnetic resonance (NMR). Invited to Stanford as associate professor in 1965, where he works on electron cyclotron resonance, in connection with Varian Associates. Joins Army Scientific Advisory Panel; works on “people sensors” during the Vietnam War. Appointed to PSAC (President’s Science Advisory Committee); discussion of defoliant Agent Orange. Becomes deputy director of http://resolver.caltech.edu/CaltechOH:OH_Baldeschwieler_J the Office of Science and Technology in 1970, during first Nixon administration; takes a leave from Stanford and moves to Washington, D.C. Recalls the debates on biological warfare and on whether or not to build the SST (supersonic transport). -
Badger Chemist
Est. 1953. NO. 49 2005 Badger Chemist THE NEWSLETTER OF THE UNIVERSITY OF WISCONSIN - MADISON CHEMISTRY DEPARTMENT THE NEWSLETTER OF THE UNIVERSITY OF WISCONSIN –MADISON C H E M I S T R Y DEPARTMENT CONTENTS From the Chair . 1 Current Chemistry News . 2 Our Awards . 9 New Badger Chemists. 11 Other Notable News. 13 Institute for Chemical Education . 16 The ACS Chemluminary Celebration. 18 Wisconsin Initiative for Science Literacy. 20 Journal of Chemical Education. 23 This ‘n’ That . 25 Chemistry Department Support . 27 Donors to Department Funds. 31 In Memoriam. 34 2005 BADGER CHEMIST Matthew Sanders Editor Est. 1953 NO. 49 Designed by the Instructional Media Development Center School of Education, University of Wisconsin–Madison Linda Endlich 2005 Art Direction Katie Drapp & Candice Heberer Production Assistance From the Chair January 2006 Dear Badger Chemists, I am now well into my second year as Chair of the Chemistry Department. I am grateful for the strong support the Department has received from the College of Letters and Science, and for the support I have received from my colleagues in the Department. As a result my eighteen months as Chair have been rewarding (and stimulating and busy!). The Badger Chemist, under the exceptional editorship of our Executive Director, Matt Sanders, is a wonderful vehicle for communicating our activities to alumni and friends. This issue of the Badger Chemist highlights our activities of the 2004-05 academic year, and indeed, there were many! On the teaching front, we continue to make significant efforts to excel. These efforts include training TAs in the fall, mentoring new faculty, and securing federal funding for research in education.