The Two Faces of Titanium Dioxide Nanoparticles Bio-Camouflage in 3D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

United States Patent (19) 11 Patent Number: 4,496,778 Myers Et Al
United States Patent (19) 11 Patent Number: 4,496,778 Myers et al. (45) Date of Patent: Jan. 29, 1985 (54) PROCESS FOR THE HYDROXYLATION OF 56 References Cited OLEFINS USING MOLECULAR OXYGEN, U.S. PATENT DOCUMENTS ANOSMIUM CONTAINING CATALYST, A COPPER CO-CATALYST, AND AN 2,773, 101 12/1956 Smith et al. ......................... 568/860 AROMATIC AMINE BASED PROMOTER 3,317,592 5/1967 Maclean et al. ... 568/860 3,337,635 8/1967 Norton et al. ....... 568/860 75 Inventors: Richard S. Myers, Fairlawn; Robert 4,390,739 6/1983 Michaelson et al. .... ..., 568/860 C. Michaelson, Waldwick; Richard FOREIGN PATENT DOCUMENTS G. Austin, Ridgewood, all of N.J. 32522 8/1974 Japan ................................... 568/860 73) Assignee: Exxon Research & Engineering Co., Primary Examiner-J. E. Evans Florham Park, N.J. Attorney, Agent, or Firm-Robert A. Maggio 21 Appl. No.: 538,190 57 ABSTRACT A process directed to the hydroxylation of olefins by 22 Filed: Oct. 3, 1983 reacting said olefins in the presence of oxygen, water, and a catalyst composition comprising (i) a catalytically 51 Int. Cl. ...................... C07C 29/04; CO7C 31/18; active osmium containing compound, (ii) a Co-catalyst C07C 31/22; CO7C 31/42 I comprising a copper containing compound such as 52 U.S.C. ................................. 568/860; 260/.397.2; CuBr2, and (iii) a Co-catalyst II capable of increasing 560/186; 562/587; 568/811; 568/821; 568/833; the rate and/or selectivity of the hydroxylation reac 568/838; 568/847 tion, such as pyridine is disclosed. 58 Field of Search .............. -
Cellular Uptake and Toxicological Effects of Differently Sized Zinc Oxide Nanoparticles in Intestinal Cells †
toxics Article Cellular Uptake and Toxicological Effects of Differently Sized Zinc Oxide Nanoparticles in Intestinal Cells † Anna Mittag 1,* , Christian Hoera 2, Alexander Kämpfe 2 , Martin Westermann 3, Jochen Kuckelkorn 4, Thomas Schneider 1 and Michael Glei 1 1 Department of Nutritional Toxicology, Institute of Nutritional Sciences, Friedrich Schiller University Jena, Dornburger Straße 24, 07743 Jena, Germany; [email protected] (T.S.); [email protected] (M.G.) 2 German Environment Agency, Swimming Pool Water, Chemical Analytics, Heinrich-Heine-Straße 12, 08645 Bad Elster, Germany; [email protected] (C.H.); [email protected] (A.K.) 3 Electron Microscopy Centre, Friedrich Schiller University Jena, Ziegelmühlenweg 1, 07743 Jena, Germany; [email protected] 4 German Environment Agency, Toxicology of Drinking Water and Swimming Pool Water, Heinrich-Heine-Straße 12, 08645 Bad Elster, Germany; [email protected] * Correspondence: [email protected] † In respectful memory of Dr. Tamara Grummt. Abstract: Due to their beneficial properties, the use of zinc oxide nanoparticles (ZnO NP) is constantly increasing, especially in consumer-related areas, such as food packaging and food additives, which is leading to an increased oral uptake of ZnO NP. Consequently, the aim of our study was to investigate the cellular uptake of two differently sized ZnO NP (<50 nm and <100 nm; 12–1229 µmol/L) using two human intestinal cell lines (Caco-2 and LT97) and to examine the possible resulting toxic effects. ZnO NP (<50 nm and <100 nm) were internalized by both cell lines and led to intracellular changes. Citation: Mittag, A.; Hoera, C.; Kämpfe, A.; Westermann, M.; Both ZnO NP caused time- and dose-dependent cytotoxic effects, especially at concentrations of Kuckelkorn, J.; Schneider, T.; Glei, M. -

United States Patent Office Attented Oct
3,536,479 United States Patent Office attented Oct. 27, 1970 2 a hydrogen pressure of at least about 15 pounds per 3,536,479 square inch gauge (p.S.i.g.). METHOD FOR THE PRODUCTION OF HIGH PURTY (OSMUM The concentrated osmium-containing solution can ad Alexander Ellis, Clarkson, Ontario, and Alan Manson, vantageously be prepared from a dilute osmium-contain Oakville, Ontario, Canada, assignors to The Interna 5 ing solution as described hereinafter. However, most gen tional Nicke Company, Inc., New York, N.Y., a cor erally the concentrated solution will be prepared by poration of Delaware scrubbing gases containing osmium tetroxide with a Solu No Drawing. Filled Dec. 13, 1967, Ser. No. 690,083 tion containing, by weight, about 5% to 40% sodium hy Claims priority, application Canada, Feb. 21, 1967, droxide to produce a sodium perosmate solution which 983,421 10 contains about 5 grams per liter (gp.l.) to about 100 nt. C. C22b 7/00, 11/04 g.p.l. of osmium, e.g., about 60 g.p.l. of osmium. Gen U.S. C. 75-108 29 Claims erally at this stage only minor amounts of ruthenium, i.e., less than about 0.5 g.p.l. of ruthenium, accompany the osmium and can be precipitated with only minor ABSTRACT OF THE DISCLOSURE 5 amounts of osmium occluded therein from the concen Metallic osmium is recovered from a slurry of an trated osmium-containing solution by adding a Water osmium-containing material to which sufficient hydro soluble, mild organic reducing agent such as methyl al chloric acid has been added to assure a final pH value cohol and ethyl alcohol. -

Deposition of Osmium Tetroxide on Reactive Surfaces
Deposition of osmium tetroxide on reactive surfaces A. von Zweidorf1,2, R. Angert1, W. Brüchle1, E. Jäger1, J.V. Kratz2, G. Langrock2, M. Mendel2, A. Nähler2, M. Schädel1, B. Schausten1, E. Schimpf1, E. Stiel1, N. Trautmann2, G. Wirth1 1Gesellschaft für Schwerionenforschung, Darmstadt, 2Institut für Kernchemie, Johannes Gutenberg-Universität Mainz The recent study of the chemistry of element 108, hassium [1], cis-1,4-polybutadiene is more reactive than etched surfaces of leads to the conclusion, that it forms a volatile oxide, as zinc and lead, on which almost nothing is deposited. expected for a member of group 8 of the periodic table [2]. So This leads to the implication, that alternative materials for the far, no chemical reaction of this oxide is known. To learn more deposition of OsO4 are needed. about the chemical behaviour of hassium, one would like to If alkaline materials are suitable for our purposes, an alkaline investigate the chemistry of hassium oxide, the only known surface would be most efficient. Unfortunately, it is hardly compound of hassium. Presumably, it is chemically similar to possible to reproducibly prepare thin layers of an alkali OsO4 and RuO4, which have an acidic character and are able to hydroxide without a substrate. Nevertheless, is it possible to form salts with alkaline materials. coat an inert material with a smooth layer of alkali hydroxide. For that reason, a Continuously Working Arrangement For We choosed at first graphite as inert substrate and coated it with Clusterless Transport Of In-situ Produced Volatile Oxides, a thin layer of KOH, using the solubility of KOH in C2H5OH CALLISTO, was developed and successfully used to deposit the and preparing the layer from an ethanolic solution. -

Particularly Hazardous Substances
Particularly Hazardous Substances In its Laboratory Standard, OSHA requires the establishment of additional protections for persons working with "Particularly Hazardous Substances" (PHS). OSHA defines these materials as "select" carcinogens, reproductive toxins and acutely toxic materials. Should you wish to add: explosive, violently reactive, pyrophoric and water-reactve materials to this category, the information is included. Carbon nanotubes have also been added due to their suspected carcinogenic properties. This table is designed to assist the laboratory in the identification of PHS, although it is not definitively conclusive or entirely comprehensive. *Notes on the proper use of this table appear on page 12. 1 6 5 2 3 4 Substance CAS National Toxicity National Program Carcinogen Toxin Acute Regulated OSHA Carcinogen Group IARC Carcinogen Toxin Reproductive Violently Reactive/ Explosive/Peroxide Forming/Pyrophoric A-a-C(2-Amino-9H-pyrido[2,3,b]indole) 2648-68-5 2B Acetal 105-57-7 yes Acetaldehyde 75-07-0 NTP AT 2B Acrolein (2-Propenal) 107-02-8 AT Acetamide 126850-14-4 2B 2-Acetylaminofluorene 53-96-3 NTP ORC Acrylamide 79-06-6 NTP 2B Acrylyl Chloride 814-68-6 AT Acrylonitrile 107-13-1 NTP ORC 2B Adriamycin 23214-92-8 NTP 2A Aflatoxins 1402-68-2 NTP 1 Allylamine 107-11-9 AT Alkylaluminums varies AT Allyl Chloride 107-05-1 AT ortho-Aminoazotoluene 97-56-3 NTP 2B para-aminoazobenzene 60-09-3 2B 4-Aminobiphenyl 92-67-1 NTP ORC 1 1-Amino-2-Methylanthraquinone 82-28-0 NTP (2-Amino-6-methyldipyrido[1,2-a:3’,2’-d]imidazole) 67730-11-4 2B -

Toxic Manifestations of Osmium Tetroxide
Br J Ind Med: first published as 10.1136/oem.3.3.183 on 1 July 1946. Downloaded from TOXIC MANIFESTATIONS OF OSMIUM TETROXIDE BY A. I. G. McLAUGHLIN, R. MILTON and KENNETH M. A. PERRY From the University of Sheffield and Factory Department, Ministry of Labour and National Service, and the Department for Research in Industrial Medicine (Medical Research Council), the London Hospital Osmium is one of the precious metals and was the vapours of osmic acid gave rise to a capillary discovered in 1803 by Tenant. It occurs naturally bronchitis from which he died. Necropsy revealed in close association with iridium. Osmiridium is a confluent broncho-pneumonia with a tendency to an exceptionally hard alloy with a high melting- suppuration and gangrene; there was also a fatty point (2700° C.) and for this reason it is used degeneration of the epithelium of the renal tubules. extensively for tipping fountain-pen nibs. It is Bardieux (1898) showed that the subcutaneous and also used for electrical contacts, as a catalyst in the intramuscular injection of a 1 per cent. solution of preparation of synthetic ammonia, and for measur- osmic acid produced no serious effect in animals ing the rapidity of explosion of gun-cotton. Before but that small quantities injected into the lungs the introduction of tungsten, electric lamp filaments were immediately fatal. Attempts have been made were sometimes made with it. Osmium is also to make use of the solution in treating diseases such used in the taking of finger-prints, and osmic acid as tuberculosis (Walbum, 1926), syphilis (Levaditi, which is a watery solution of osmium tetroxide is 1927; and Jahnel, 1937) and cancer (Kraus, 1931) used for activating solutions of chlorate of potas- but without success, though Fischl (1933) showed it sium; hardening and colouring certain prepara- possessed some spirochaetocidal properties in tions and in histology for the fixing and staining of experimentally infected mice Coca (1908) studied nerves and fat. -

Ruthenium Tetroxide and Perruthenate Chemistry. Recent Advances and Related Transformations Mediated by Other Transition Metal Oxo-Species
Molecules 2014, 19, 6534-6582; doi:10.3390/molecules19056534 OPEN ACCESS molecules ISSN 1420-3049 www.mdpi.com/journal/molecules Review Ruthenium Tetroxide and Perruthenate Chemistry. Recent Advances and Related Transformations Mediated by Other Transition Metal Oxo-species Vincenzo Piccialli Dipartimento di Scienze Chimiche, Università degli Studi di Napoli ―Federico II‖, Via Cintia 4, 80126, Napoli, Italy; E-Mail: [email protected]; Tel.: +39-081-674111; Fax: +39-081-674393 Received: 24 February 2014; in revised form: 14 May 2014 / Accepted: 16 May 2014 / Published: 21 May 2014 Abstract: In the last years ruthenium tetroxide is increasingly being used in organic synthesis. Thanks to the fine tuning of the reaction conditions, including pH control of the medium and the use of a wider range of co-oxidants, this species has proven to be a reagent able to catalyse useful synthetic transformations which are either a valuable alternative to established methods or even, in some cases, the method of choice. Protocols for oxidation of hydrocarbons, oxidative cleavage of C–C double bonds, even stopping the process at the aldehyde stage, oxidative cleavage of terminal and internal alkynes, oxidation of alcohols to carboxylic acids, dihydroxylation of alkenes, oxidative degradation of phenyl and other heteroaromatic nuclei, oxidative cyclization of dienes, have now reached a good level of improvement and are more and more included into complex synthetic sequences. The perruthenate ion is a ruthenium (VII) oxo-species. Since its introduction in the mid-eighties, tetrapropylammonium perruthenate (TPAP) has reached a great popularity among organic chemists and it is mostly employed in catalytic amounts in conjunction with N-methylmorpholine N-oxide (NMO) for the mild oxidation of primary and secondary alcohols to carbonyl compounds. -

Material Safety Data Sheet Product No. 18466 Osmium Tetroxide, 2% Aqueous Issue Date (06-05-12) Review Date (06-05-12)
Material Safety Data Sheet Product No. 18466 Osmium Tetroxide, 2% Aqueous Issue Date (06-05-12) Review Date (06-05-12) Section 1: Product and Company Identification Product Name: Osmium Tetroxide, 2% Aqueous Synonym: Osmium Tetroxide, Osmic Acid Solution, Osmium (VIII) Oxide Chemical Family: Platinum Group Metal Salts Company Name Ted Pella, Inc. P.O. Box 492477, Redding, CA 96049-2477 Domestic Phone (800) 237-3526 (Mon-Thu. 6:00AM to 4:30PM PST; Fri 6:00AM to 4:00PM PST) International Phone (01) (530) 243-2200 (Mon-Thu. 6:00AM to 4:30PM PST; Fri 6:00AM to 4:00PM PST) Chemtrec Emergency Number 1-800-424-9300 24 hrs a day. Section 2: Composition / Information on Ingredients % Principle Hazardous OSHA ACGIH ACGIH OSHA Component(s) PEL TLV TLV- NTP IARC (chemical and common name(s)) regulated (Cas. No) mg/m3 mg/m3 STEL ppm Osmium Tetroxide/Osmium 2 0.002 0.0006 0.002 No No No Oxide (20816-12-0) Water (7732-18-5) 98 NE NE NE No No No Section 3: Hazard Identification Emergency overview Appearance: Colorless to pale yellow solution. Immediate effects: This substance can be absorbed into the body by inhalation of its vapors, by inhalation of its aerosol and by ingestion. May cause sensitization by inhalation and skin contact. Target Organs: Eyes and Central Nervous System. Potential health effects Primary Routes of entry: Eyes: Likely; Inhalation: Highly; Skin: Likely; Ingestion: Likely Signs and Symptoms of Overexposure: ND Eyes: Irritation, lacrimation, visual disturbance, conjunctivitis, headache, potential damage to cornea. If eyes are exposed to vapor over a short period of time, night vision will be affected for about one evening. -
Osmium Tetroxide [CAS No
LABORATORY SAFETY GUIDELINE Osmium Tetroxide [CAS No. 20816-12-0] All users of Osmium Tetroxide must review this document before use. Osmium tetroxide (OsO4) is a highly poisonous, pale yellow solid that is volatile. It is a corrosive oxidizer that produces an acrid chlorine like odor. Osmium tetroxide is most commonly used in oxidation reactions and as a fixative for biological staining. Users should contact their EHS Laboratory Safety Advisor and department safety officer if they have questions before beginning work. HAZARDS The acute toxicity is high, and it is a severe irritant of the eyes and respiratory tract. Vapors can damage the cornea of the eye and even lead to blindness. Concentrations of vapor that do not cause immediate irritation can have a dangerous cumulative effect; symptoms may not be noted until several hours after exposure. Inhalation can cause chemical burns to the respiratory tract, headache, coughing, dizziness, lung damage, and difficult breathing, and may potentially be fatal. Chronic exposure can result in accumulation of osmium compounds in the liver and kidney, and damage to these organs. Exposure via inhalation, skin contact, or ingestion can lead to systemic toxic effects involving liver and kidney damage. Repeated exposure may cause sensitization by inhalation or skin contact. Corrosive to skin and eyes, exposure may cause blindness. Contact of the vapor with skin can cause dermatitis, and direct contact with the solid can lead to severe irritation and burns. PRECAUTIONS • Osmium tetroxide is a strong oxidizer that will sublime (pass directly from solid to vapor and back to solid) readily at room temperature and significantly when refrigerated. -
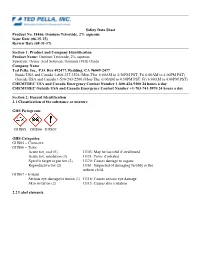
Safety Data Sheet Product No. 18466, Osmium Tetroxide, 2% Aqueous Issue Date (06-15-15) Review Date (08-31-17)
Safety Data Sheet Product No. 18466, Osmium Tetroxide, 2% aqueous Issue Date (06-15-15) Review Date (08-31-17) Section 1: Product and Company Identification Product Name: Osmium Tetroxide, 2% aqueous Synonym: Osmic Acid Solution, Osmium (VIII) Oxide Company Name Ted Pella, Inc., P.O. Box 492477, Redding, CA 96049-2477 Inside USA and Canada 1-800-237-3526 (Mon-Thu. 6:00AM to 4:30PM PST; Fri 6:00AM to 4:00PM PST) Outside USA and Canada 1-530-243-2200 (Mon-Thu. 6:00AM to 4:30PM PST; Fri 6:00AM to 4:00PM PST) CHEMTREC USA and Canada Emergency Contact Number 1-800-424-9300 24 hours a day CHEMTREC Outside USA and Canada Emergency Contact Number +1-703-741-5970 24 hours a day Section 2: Hazard Identification 2.1 Classification of the substance or mixture GHS Pictograms GHS05 GHS06 GHS07 GHS Categories GHS05 – Corrosive GHS06 – Toxic Acute tox, oral (5) H303: May be harmful if swallowed Acute tox, inhalation (3) H331: Toxic if inhaled Specific target organ tox (2) H370: Causes damage to organs Reproductive tox (2) H361: Suspected of damaging fertility or the unborn child. GHS07 – Irritant Serious eye damage/irritation (1) H318: Causes serious eye damage Skin irritation (2) H315: Causes skin irritation 2.2 Label elements Hazard pictograms GHS06 GHS05 GHS07 Signal Word: DANGER Hazard statements H303: May be harmful if swallowed H315: Causes skin irritation H318: Causes serious eye damage H331: Toxic if inhaled H370: Causes damage to organs H361: Suspected of damaging fertility or the unborn child Precautionary statements P202: Do not handle until all safety precautions have been read and understood P210: Keep away from heat/sparks/open flames/hot surfaces – No smoking P264: Wash thoroughly after handling P280: Wear protective gloves/protective clothing/eye protection/face protection P308+313: IF exposed or concerned: Get medical advice/attention. -

The Preparation and Characterization of Some Alkanethiolatoosmium Compounds Harold Harris Schobert Iowa State University
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 1970 The preparation and characterization of some alkanethiolatoosmium compounds Harold Harris Schobert Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Inorganic Chemistry Commons Recommended Citation Schobert, Harold Harris, "The preparation and characterization of some alkanethiolatoosmium compounds " (1970). Retrospective Theses and Dissertations. 4357. https://lib.dr.iastate.edu/rtd/4357 This Dissertation is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. 71-14,258 SCHOBERT, Harold Harris, 1943- THE PREPARATION AND CHARACTERIZATION OF SOME ALKANETHIOLATOOSMIUM COMPOUNDS. Iowa State University, Ph.D., 1970 Chemistry, inorganic University Microfilms, A XEROX Company, Ann Arbor, Michigan THIS DISSERTATION HAS BEEH MICROFILMED EXACTLY AS RECEIVED THE PREPARATION AND CHARACTERIZATION OF SOME ALKANETHIOLATOOSMIUM COMPOUNDS by Harold Harris Schobert A Dissertation Submitted to the Graduate Faculty in Partial Fulfillment of The Requirements for the Degree of DOCTOR OF PHILOSOPHY Major Subject: Inorganic Chemistry Approved: Signature was redacted for privacy. Signature was redacted for -

Osmium Catalyzed Dihydroxylation and Oxidative Cleavage of Vinyl
Purdue University Purdue e-Pubs Open Access Dissertations Theses and Dissertations Fall 2013 Osmium Catalyzed Dihydroxylation And Oxidative Cleavage Of Vinyl Sulfone And Elucidation Of The inV ylsulfone Polypropionate Methodology For The yS nthesis Of The C32 esD - Methyl C28-C34 Actin Binding Tail Of Aplyronine A Thomas Paul Bobinski Purdue University Follow this and additional works at: https://docs.lib.purdue.edu/open_access_dissertations Part of the Organic Chemistry Commons Recommended Citation Bobinski, Thomas Paul, "Osmium Catalyzed Dihydroxylation And Oxidative Cleavage Of Vinyl Sulfone And Elucidation Of The Vinylsulfone Polypropionate Methodology For The yS nthesis Of The C32 eD s-Methyl C28-C34 Actin Binding Tail Of Aplyronine A" (2013). Open Access Dissertations. 199. https://docs.lib.purdue.edu/open_access_dissertations/199 This document has been made available through Purdue e-Pubs, a service of the Purdue University Libraries. Please contact [email protected] for additional information. Graduate School ETD Form 9 (Revised 12/07) PURDUE UNIVERSITY GRADUATE SCHOOL Thesis/Dissertation Acceptance This is to certify that the thesis/dissertation prepared By Thomas Paul Bobinski Entitled For the degree of Doctor of Philosophy Is approved by the final examining committee: Philip L. Fuchs Chair Paul Wenthold Mark Lipton Mahdi abu-Omar To the best of my knowledge and as understood by the student in the Research Integrity and Copyright Disclaimer (Graduate School Form 20), this thesis/dissertation adheres to the provisions of Purdue