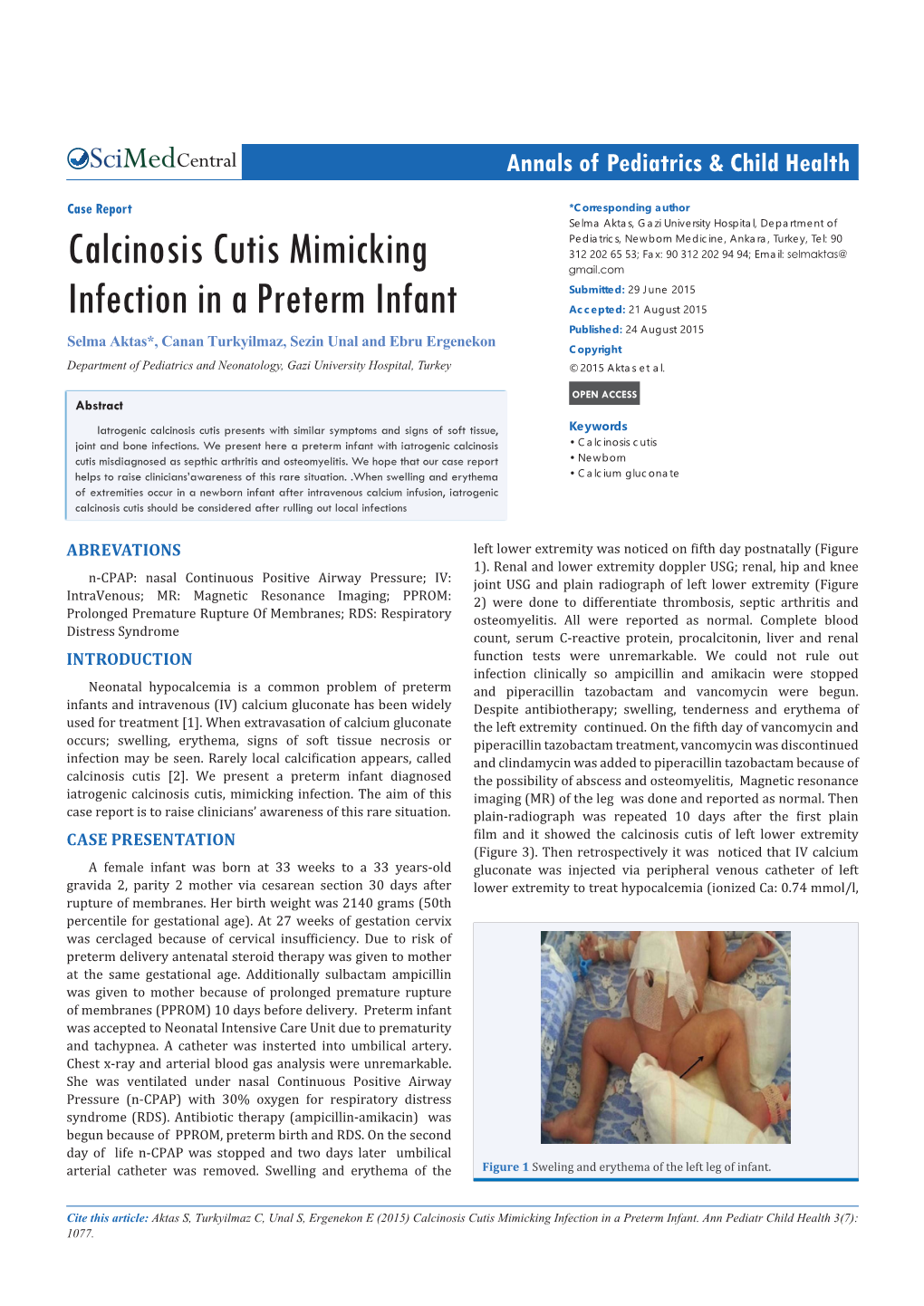
Calcinosis Cutis Mimicking Infection in a Preterm Infant
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Early Manifestation of Calcinosis Cutis in Pseudohypoparathyroidism Type
European Journal of Endocrinology (2005) 152 515–519 ISSN 0804-4643 CASE REPORT Early manifestation of calcinosis cutis in pseudohypoparathyroidism type Ia associated with a novel mutation in the GNAS gene Felix G Riepe, Wiebke Ahrens1, Nils Krone, Regina Fo¨lster-Holst2, Jochen Brasch2, Wolfgang G Sippell, Olaf Hiort1 and Carl-Joachim Partsch3 Department of Pediatrics, Division of Pediatric Endocrinology, Universita¨tsklinikum Schleswig-Holstein, Campus Kiel, Christian-Albrechts-Universita¨t, 24105 Kiel, Germany, 1Department of Pediatrics, Division of Pediatric Endocrinology and Diabetes, Universita¨tsklinikum Schleswig-Holstein, Campus Lu¨beck, Universita¨t zu Lu¨beck, 23538 Lu¨beck, Germany, 2Department of Dermatology, Universita¨tsklinikum Schleswig-Holstein, Campus Kiel, Christian-Albrechts-Universita¨t, 24105 Kiel, Germany and 3Children’s Hospital, Sta¨dtische Kliniken Esslingen, 73730 Esslingen a.N., Germany (Correspondence should be addressed to W G Sippell; Email: [email protected]) Abstract Objective: To clarify the molecular defect for the clinical finding of congenital hypothyroidism com- bined with the manifestation of calcinosis cutis in infancy. Case report: The male patient presented with moderately elevated blood thyrotropin levels at neonatal screening combined with slightly decreased plasma thyroxine and tri-iodothyronine concentrations, necessitating thyroid hormone substitution 2 weeks after birth. At the age of 7 months calcinosis cutis was seen and the patient underwent further investigation. Typical features of Albright’s heredi- tary osteodystrophy (AHO), including round face, obesity and delayed psychomotor development, were found. Methods and results: Laboratory investigation revealed a resistance to parathyroid hormone (PTH) with highly elevated PTH levels and a reduction in adenylyl cyclase-stimulating protein (Gsa) activity leading to the diagnosis of pseudohypoparathyroidism type Ia (PHP Ia). -

Tumoral Calcinosis and Calciphylaxis Treated with Subtotal Parathyroidectomy and Sodium Thiosulphate
CASE REPORT eISSN 2384-0293 Yeungnam Univ J Med 2016;33(1):68-71 http://dx.doi.org/10.12701/yujm.2016.33.1.68 Tumoral calcinosis and calciphylaxis treated with subtotal parathyroidectomy and sodium thiosulphate Hyunjeong Cho1, Yongjin Yi1, Eunjeong Kang1, Seokwoo Park1, Eun Jin Cho2, Sung Tae Cho3, Rho Won Chun3, Kyu Eun Lee4, Kook-Hwan Oh1 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul; 2Department of Internal Medicine, Hongseong Medical Center, Hongseong; 3Dr. Chun & Cho`s Medical Clinic & Dialysis Center; 4Department of Surgery, Seoul National University College of Medicine, Seoul, Korea Tumoral calcinosis (TC) is a condition resulting from extensive calcium phosphate precipitation, primarily in the periarticular tissues around major joints. Calciphylaxis is a fatal ischemic vasculopathy mainly affecting dermal blood vessels and subcutaneous fat. This syndrome is rare and predominantly occurs in patients with end-stage renal disease. Here, we report on a rare case involving a patient with TC complicated with calciphylaxis. Our patient was a 31-year-old man undergoing hemodialysis who presented with masses on both shoulders and necrotic cutaneous ulcers, which were associated with secondary hyperparathyroidism, on his lower legs. He underwent subtotal parathyroidectomy, and sodium thiosulfate (STS) was administered for 27 weeks. Twenty months after beginning the STS treatment course, he experienced dramatic relief of his TC and calciphylaxis. Keywords: Tumoral calcinosis; Calciphylaxis; Parathyroidectomy; Sodium thiosulphate INTRODUCTION reported to range from 0.5-3% [2]. The pathomechanisms of these two disorders are poorly understood, but believed to Calcinosis cutis is characterized by the deposition of in- be related to disturbances in mineral metabolism. -

Section XI Extraskeletal (Ectopic) Calcification and Ossification
Section XI Extraskeletal (Ectopic) Calcification and Ossification Michael P. Whyte Division of Bone and Mineral Diseases, Washington University School of Medicine at Barnes-Jewish Hospital and Center for Metabolic Bone Disease and Molecular Research, Shriners Hospitals for Children, St. Louis, Missouri INTRODUCTION somewhat higher value because they have greater serum phos- phate concentrations compared with adults. However, this is A significant number and variety of disorders cause extraskel- not well established.(5) etal deposition of calcium and phosphate (Table 1). In some, The material that comprises metastatic calcification may be mineral is precipitated as amorphous calcium phosphate or as amorphous calcium phosphate initially, but hydroxyapatite is crystals of hydroxyapatite; in others, osseous tissue is formed. deposited soon after.(2) The anatomic pattern of deposition The pathogenesis of ectopic mineralization is generally attrib- varies somewhat between hypercalcemia and hyperphos- uted to one of three mechanisms (Table 1). First, a supranormal phatemia, but occurs irrespective of the specific underlying “calcium-phosphate solubility product” in extracellular fluid condition or mechanism for the disturbed mineral homeostasis. can cause metastatic calcification. Second, mineral may be Additionally, there is a predilection for certain tissues. deposited as dystrophic calcification into metabolically im- Hypercalcemia is typically associated with mineral deposits paired or dead tissue despite normal serum levels of calcium in the kidneys, lungs, and fundus of the stomach. In these and phosphate. Third, ectopic ossification (or true bone forma- “acid-secreting” organs, a local alkaline milieu may account tion) occurs in a few disorders for which the pathogenesis is for the calcium deposition. In addition, the media of large becoming increasingly understood. -

Parenteral Nutrition Primer: Balance Acid-Base, Fluid and Electrolytes
Parenteral Nutrition Primer: Balancing Acid-Base, Fluids and Electrolytes Phil Ayers, PharmD, BCNSP, FASHP Todd W. Canada, PharmD, BCNSP, FASHP, FTSHP Michael Kraft, PharmD, BCNSP Gordon S. Sacks, Pharm.D., BCNSP, FCCP Disclosure . The program chair and presenters for this continuing education activity have reported no relevant financial relationships, except: . Phil Ayers - ASPEN: Board Member/Advisory Panel; B Braun: Consultant; Baxter: Consultant; Fresenius Kabi: Consultant; Janssen: Consultant; Mallinckrodt: Consultant . Todd Canada - Fresenius Kabi: Board Member/Advisory Panel, Consultant, Speaker's Bureau • Michael Kraft - Rockwell Medical: Consultant; Fresenius Kabi: Advisory Board; B. Braun: Advisory Board; Takeda Pharmaceuticals: Speaker’s Bureau (spouse) . Gordon Sacks - Grant Support: Fresenius Kabi Sodium Disorders and Fluid Balance Gordon S. Sacks, Pharm.D., BCNSP Professor and Department Head Department of Pharmacy Practice Harrison School of Pharmacy Auburn University Learning Objectives Upon completion of this session, the learner will be able to: 1. Differentiate between hypovolemic, euvolemic, and hypervolemic hyponatremia 2. Recommend appropriate changes in nutrition support formulations when hyponatremia occurs 3. Identify drug-induced causes of hypo- and hypernatremia No sodium for you! Presentation Outline . Overview of sodium and water . Dehydration vs. Volume Depletion . Water requirements & Equations . Hyponatremia • Hypotonic o Hypovolemic o Euvolemic o Hypervolemic . Hypernatremia • Hypovolemic • Euvolemic • Hypervolemic Sodium and Fluid Balance . Helpful hint: total body sodium determines volume status, not sodium status . Examples of this concept • Hypervolemic – too much volume • Hypovolemic – too little volume • Euvolemic – normal volume Water Distribution . Total body water content varies from 50-70% of body weight • Dependent on lean body mass: fat ratio o Fat water content is ~10% compared to ~75% for muscle mass . -

Case Report Calcinosis Cutis Associated with Chronic Sclerodermoid Graft Versus Host Disease: a Case and Review of the Literature
Hindawi Case Reports in Dermatological Medicine Volume 2020, Article ID 9250923, 4 pages https://doi.org/10.1155/2020/9250923 Case Report Calcinosis Cutis Associated with Chronic Sclerodermoid Graft versus Host Disease: A Case and Review of the Literature Jacqueline Deen , Lisa Byrom, and Ivan Robertson Department of Dermatology, Royal Brisbane and Women’s Hospital, Brisbane, Queensland, Australia Correspondence should be addressed to Jacqueline Deen; [email protected] Received 11 December 2019; Revised 23 January 2020; Accepted 5 February 2020; Published 28 February 2020 Academic Editor: Alireza Firooz Copyright © 2020 Jacqueline Deen et al. )is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. We present a rare case of calcinosis cutis associated with chronic sclerodermoid graft versus host disease in a 59-year-old male, 13 years following allogenic bone marrow transplantation. )e etiology of calcification was thought to be dystrophic. Further research is needed to understand the link between calcinosis cutis and chronic sclerodermoid graft versus host disease to assist with selecting appropriate management for these patients. 1. Introduction occurs from the deposition of calcium salts in the skin secondary to medical interventions, typically intravenous Calcinosis cutis is a descriptive term for the deposition of calcium gluconate and calcium chloride. Idiopathic calci- insoluble calcium salts in the dermis and subcutaneous fication occurs in the absence of an underlying tissue injury tissue and is associated with a number of underlying or metabolic disorder. )e final subtype, calciphylaxis, is a disorders. -

Calcinosis Cutis,Calcinosis Circumscripta,And “Mille Feuille
Calcinosis Cutis, Calcinosis Circumscripta, and “Mille Feuille” Lesions James Yi-Chien Lin, DVM MS; Han-Ju Tsai, DVM MS; Kau-Shen Hsu, DVM; Fun-In Wang, DVM PhD Skin and subcutaneous lesions of 2 cases with natural occurring Cushing’s disease and 1 case with calcinosis circumscripta were compared. Case 1 was typical of osteoma cutis, containing somewhat regularly arranged discrete ossification foci in the mid and deep dermis. Case 2 had layers of “mille feuille”, yellowish to white gritty chalky substances diffusely scattered in the sub- cutis, seen histologically as disseminatedly scattered light purple crystalloid and blue granular mineral salts. Lesions stained orange red with Alizarin Red S indicated the presence of calcium ions. Discrete ossification foci in the deep dermis and early multifocal collagenolysis with mine- ralization were also noted. Case 3 was typical of calcinosis circumscripta, seen grossly as yel- lowish chalky substance in both dermis and subcutis, and histologically as lakes of well- circumscribed light purple crystals and granular deep blue mineral salts. Case 2 had features of calcinosis cutis such as ossification foci and early multifocal collagenolysis. Case 2 also had “mille feuille” that was histologically similar to those mineral salts in case 3, but was not circum- scribed, and was not exactly calcinosis universalis. The component in case 1 was most likely hydroxyapatite Ca10(PO4)6(OH)2; the “mille feuille” of case 2 was most likely “calcium soap” after panniculitis and fat necrosis; and that in case 3 was most likely calcium phosphate CaPO4. Lo- cal factors, such as fluid exudation reflecting how well the inflammation was controlled clinically, may influence the wound healing, and thus the outcome of lesions. -

Role of Phosphate in Biomineralization
Henry Ford Health System Henry Ford Health System Scholarly Commons Endocrinology Articles Endocrinology and Metabolism 7-25-2020 Role of Phosphate in Biomineralization Sanjay Kumar Bhadada Sudhaker D. Rao Henry Ford Health System, [email protected] Follow this and additional works at: https://scholarlycommons.henryford.com/endocrinology_articles Recommended Citation Bhadada SK, and Rao SD. Role of Phosphate in Biomineralization. Calcif Tissue Int 2020. This Article is brought to you for free and open access by the Endocrinology and Metabolism at Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Endocrinology Articles by an authorized administrator of Henry Ford Health System Scholarly Commons. Calcifed Tissue International https://doi.org/10.1007/s00223-020-00729-9 REVIEW Role of Phosphate in Biomineralization Sanjay Kumar Bhadada1 · Sudhaker D. Rao2,3 Received: 31 March 2020 / Accepted: 14 July 2020 © Springer Science+Business Media, LLC, part of Springer Nature 2020 Abstract Inorganic phosphate is a vital constituent of cells and cell membranes, body fuids, and hard tissues. It is a major intracel- lular divalent anion, participates in many genetic, energy and intermediary metabolic pathways, and is important for bone health. Although we usually think of phosphate mostly in terms of its level in the serum, it is needed for many biological and structural functions of the body. Availability of adequate calcium and inorganic phosphate in the right proportions at the right place is essential for proper acquisition, biomineralization, and maintenance of mass and strength of the skeleton. The three specialized mineralized tissues, bones, teeth, and ossicles, difer from all other tissues in the human body because of their unique ability to mineralize, and the degree and process of mineralization in these tissues also difer to suit the specifc functions: locomotion, chewing, and hearing, respectively. -
Understanding Calcinosis and Calciphylaxis
PRACTICE DEVELOPMENT Understanding calcinosis and calciphylaxis KEY WORDS Calcinosis cutis is a rare cause of non-healing leg ulceration. There are many factors Calcinosis cutis that can delay the healing of venous leg ulceration and the deposition of calcium in Calciphylaxis the skin known as calcinosis cutis is one of these factors. There are five distinct forms: Warfarin-induced skin dystrophic calcification, metastatic calcification, idiopathic calcification, iatrogenic necrosis calcification and calciphylaxis. Warfarin skin necrosis has common clinical features with calciphylaxis and is therefore included in this article, which describes the types of calcinosis cutis, their clinical presentations and limited treatment options. The aim is to highlight these unusual causes and to assist healthcare professionals when faced with a non-healing ulcer. eg ulceration can be defined as a defect in neurotransmission and the blood coagulation the dermis located on the leg (Franks et al, pathway. At a cellular level, it is implicated in 2016). Leg ulceration is a significant clinical cell-to-cell communication (Walshe and Fairley, Lproblem with the majority attributing venous 1995). In the skin, it is specifically concerned with hypertension as the underlying disease process with keratinocyte proliferation, differentiation and venous leg ulceration affecting 1% of the population adhesion (Smith and Yamada, 2002). in the western world (Posnett et al, 2009). However, The level of serum calcium is closely there is a multitude of causative factors of leg ulcers, controlled by the parathyroid hormone. with the term leg ulcer purely signifying the clinical Regardless of this regulation, it is possible for manifestation and not the underlying aetiology. -

Calciphylaxis
Postgrad Med J 2001;77:557–561 557 Postgrad Med J: first published as 10.1136/pmj.77.911.557 on 1 September 2001. Downloaded from REVIEWS Calciphylaxis R V Mathur, J R Shortland, A M El Nahas Abstract phosphate diet act as sensitising agents result- The phenomenon of calciphylaxis is rare, ing in a high calcium-phosphate product (Ca × but potentially fatal. It has been recog- P; normal range 4.2–5.6 mmol2/l2) with result- nised for a long time in patients with ant precipitation of Ca-P crystals.14 This results chronic renal failure with secondary hy- in diVuse calcification of the media and perparathyroidism. Disturbed calcium internal elastic lamina of small to medium and phosphate metabolism can result in sized arteries and arterioles with intimal prolif- painful necrosis of skin, subcutaneous tis- eration and rarely arterial occlusion causing sue and acral gangrene. Appearance of the tissue necrosis. This entity was given the term lesions is distinctive but the pathogenesis calcinosis cutis to signify vascular calcification remains uncertain. The beneficial eVects with ischaemic epidermolysis as seen in of parathyroidectomy are controversial. patients with chronic renal failure on However, correction of hyperphosphatae- haemodialysis.15–17 Other triggering events in- mia or occasionally hypercalcaemia is clude intravenous iron dextran and albumin imperative. Fulminant sepsis as a conse- infusion, low serum albumin, corticosteroids, quence of secondary infection of necrotic immunosuppression, trauma, subcutaneous in- and gangrenous tissue is a frequent cause jections in obese patients, and protein C and S of patient morbidity and mortality. deficiencies causing hypercoagulability and 8 12 16 18–25 (Postgrad Med J 2001;77:557–561) subsequent thrombosis. -

CALCIUM DEPOSITS in the SKIN (Calcinosis)
CALCIUM DEPOSITS IN THE SKIN (Calcinosis) What is this problem? Calcium deposits in the skin have a variety of causes, usually of minor significance in the young but indicating serious disease in some older animals. Calcinosis circumscripta is deposits of calcium at bony prominences or in the footpads and mouth. It is usually a disease of large dog breeds and occurs before two years of age. Calcinosis cutis is induced by local damage in susceptible animals. The cause may be either dystrophic (local factors only causing damage leading to calcification) or metastatic (too high a concentration of calcium in the blood leading to deposits of calcium in the locally damaged tissues). In the latter case, there may be multiple calcium deposits. What do we know about the cause? The reason why a particular pet may develop this, or any Image courtesy of Jan Hall, BVM&S, MS, MRCVS, DipACVD, cancer, is not straightforward. Cancer is often seemingly the Clinical Dermatology, culmination of a series of circumstances that come together for Ontario Veterinary College the unfortunate individual. The cause of calcinosis circumscripta is unknown but there is often a genetic component. The most probable immediate cause is an increase in the blood enzyme lipase leading to degeneration of the subcutaneous adipose tissue followed by calcification. Dystrophic causes of calcinosis cutis include idiosyncratic reactions to injections and other foreign materials. The most common cause of metastatic calcinosis cutis in dogs is overproduction of adrenal hormones (corticosteroids or “steroids”). This may be due to overgrowth or cancer of the adrenal glands, or of the pituitary, the gland that controls the adrenals. -

Dermatology Grand Rounds 2019 Skin Signs of Internal Disease
Dermatology Grand Rounds 2019 skin signs of internal disease John Strasswimmer, MD, PhD Affiliate Clinical Professor (Dermatology), FAU College of Medicine Research Professor of Biochemistry, FAU College of Science Associate Clinical Professor, U. Miami Miller School of Medicine Dermatologist and Internal Medicine “Normal” abnormal skin findings in internal disease • Thyroid • Renal insufficiency • Diabetes “Abnormal” skin findings as clue to internal disease • Markers of infectious disease • Markers of internal malignancy risk “Consultation Cases” • Very large dermatology finding • A very tiny dermatology finding Dermatologist and Internal Medicine The "Red and Scaly” patient “Big and Small” red rashes not to miss The "Red and Scaly” patient • 29 Year old man with two year pruritic eruption • PMHx: • seasonal allergies • childhood eczema • no medications Erythroderma Erythroderma • Also called “exfoliative dermatitis” • Not stevens-Johnson / toxic epidermal necrosis ( More sudden onset, associated with target lesions, mucosal) • Generalized erythema and scale >80-90% of body surface • May be associated with telogen effluvium It is not a diagnosis per se Erythroderma Erythroderma Work up 1) Exam for pertinent positives and negatives: • lymphadenopathy • primary skin lesions (i.e. nail pits of psoriasis) • mucosal involvement • Hepatosplenomagaly 2) laboratory • Chem 7, LFT, CBC • HIV • Multiple biopsies over time 3) review of medications 4) age-appropriate malignancy screening 5) evaluate hemodynamic stability Erythroderma Management 1) -

Chapter 73 1009
C h a p t e r 73 Fluid and Electrolyte Issues in Pediatric Critical Illness Robert Lynch, Ellen Glenn Wood, and Tara M. Neumayr intraoperative fluids influence acid-base and electrolyte status, PEARLS particularly of vulnerable patients.4 The choice of Na+ content • Hypotonic maintenance IV fluids are associated with mild to and balancing ions of IVF for postoperative or critical care moderate hyponatremia in postoperative patients. maintenance may be important for some patients thus justify- Anesthesia, stress, and inflammatory mediators probably ing additional expense. Clearly 0.18 and 0.225 mM saline is 5,6 contribute. Electrolyte monitoring in patients at risk is associated with a higher incidence of mild hyponatremia, essential for detection and management of the occasional although controlled trials do not show this effect for 0.46 mM 7,8 patient who develops severe hyponatremia. This critical saline. Severe hyponatremia has been associated with pul- effect of the syndrome of inappropriate antidiuretic hormone monary or CNS illness in pediatrics and is infrequent even may occur even in patients on isotonic IV fluids. within those categories, with the exception of children with • Medical patients with high levels of inflammatory mediators traumatic brain injury (TBI). Among patients with those and appear to be at increased risk of significant hyponatremia. other illnesses, the evolving study of the influence of inflam- Interleukin effects on antidiuretic hormone release may matory mediators directly on the hypothalamus and indirectly contribute. on vasopressin secretion may further clarify which patients are 9,10 • Albumin infusions have been generally safe but may at most risk of clinically significant hyponatremia.