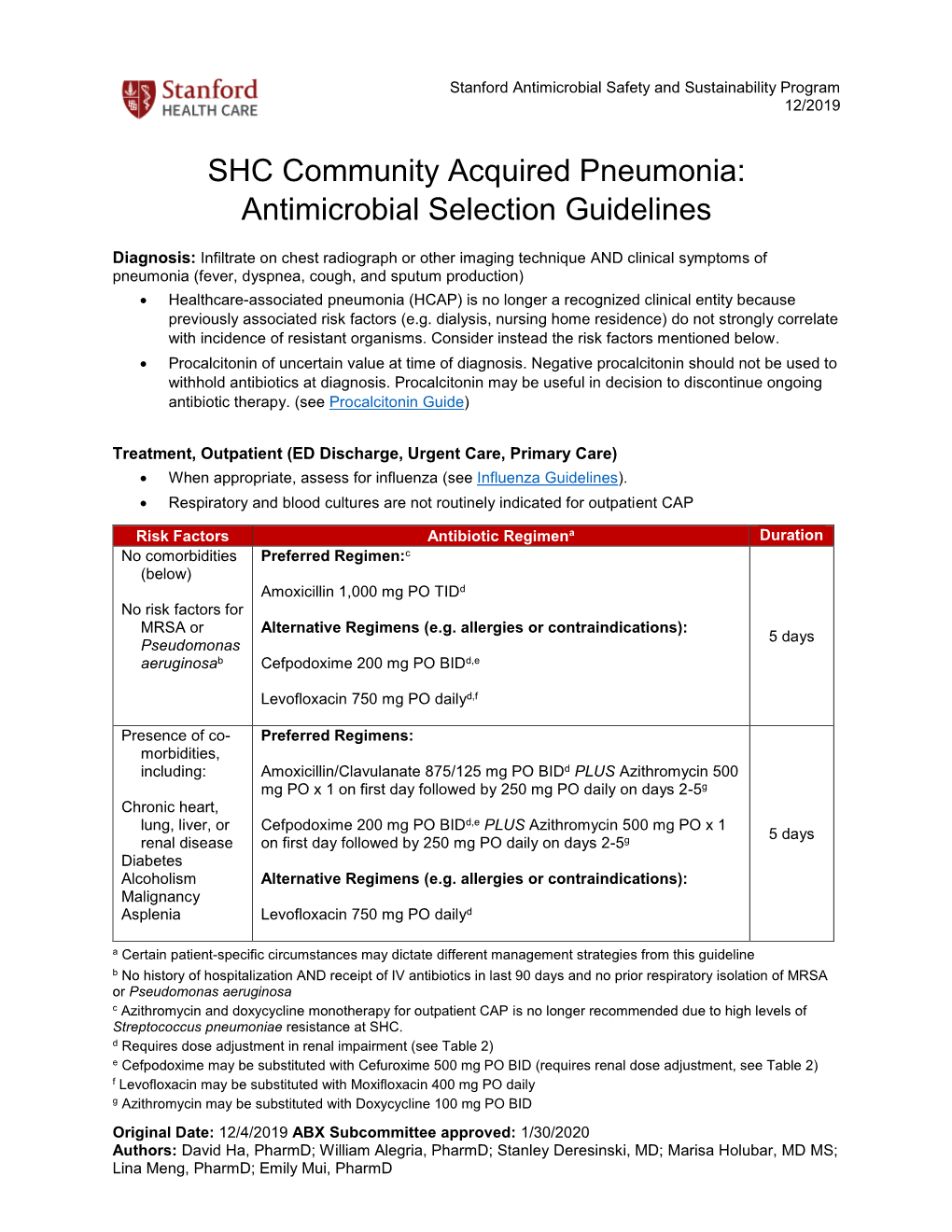
SHC Community Acquired Pneumonia: Antimicrobial Selection Guidelines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Captive Orcas
Captive Orcas ‘Dying to Entertain You’ The Full Story A report for Whale and Dolphin Conservation Society (WDCS) Chippenham, UK Produced by Vanessa Williams Contents Introduction Section 1 The showbiz orca Section 2 Life in the wild FINgerprinting techniques. Community living. Social behaviour. Intelligence. Communication. Orca studies in other parts of the world. Fact file. Latest news on northern/southern residents. Section 3 The world orca trade Capture sites and methods. Legislation. Holding areas [USA/Canada /Iceland/Japan]. Effects of capture upon remaining animals. Potential future capture sites. Transport from the wild. Transport from tank to tank. “Orca laundering”. Breeding loan. Special deals. Section 4 Life in the tank Standards and regulations for captive display [USA/Canada/UK/Japan]. Conditions in captivity: Pool size. Pool design and water quality. Feeding. Acoustics and ambient noise. Social composition and companionship. Solitary confinement. Health of captive orcas: Survival rates and longevity. Causes of death. Stress. Aggressive behaviour towards other orcas. Aggression towards trainers. Section 5 Marine park myths Education. Conservation. Captive breeding. Research. Section 6 The display industry makes a killing Marketing the image. Lobbying. Dubious bedfellows. Drive fisheries. Over-capturing. Section 7 The times they are a-changing The future of marine parks. Changing climate of public opinion. Ethics. Alternatives to display. Whale watching. Cetacean-free facilities. Future of current captives. Release programmes. Section 8 Conclusions and recommendations Appendix: Location of current captives, and details of wild-caught orcas References The information contained in this report is believed to be correct at the time of last publication: 30th April 2001. Some information is inevitably date-sensitive: please notify the author with any comments or updated information. -

The Use of Non-Human Primates in Research in Primates Non-Human of Use The
The use of non-human primates in research The use of non-human primates in research A working group report chaired by Sir David Weatherall FRS FMedSci Report sponsored by: Academy of Medical Sciences Medical Research Council The Royal Society Wellcome Trust 10 Carlton House Terrace 20 Park Crescent 6-9 Carlton House Terrace 215 Euston Road London, SW1Y 5AH London, W1B 1AL London, SW1Y 5AG London, NW1 2BE December 2006 December Tel: +44(0)20 7969 5288 Tel: +44(0)20 7636 5422 Tel: +44(0)20 7451 2590 Tel: +44(0)20 7611 8888 Fax: +44(0)20 7969 5298 Fax: +44(0)20 7436 6179 Fax: +44(0)20 7451 2692 Fax: +44(0)20 7611 8545 Email: E-mail: E-mail: E-mail: [email protected] [email protected] [email protected] [email protected] Web: www.acmedsci.ac.uk Web: www.mrc.ac.uk Web: www.royalsoc.ac.uk Web: www.wellcome.ac.uk December 2006 The use of non-human primates in research A working group report chaired by Sir David Weatheall FRS FMedSci December 2006 Sponsors’ statement The use of non-human primates continues to be one the most contentious areas of biological and medical research. The publication of this independent report into the scientific basis for the past, current and future role of non-human primates in research is both a necessary and timely contribution to the debate. We emphasise that members of the working group have worked independently of the four sponsoring organisations. Our organisations did not provide input into the report’s content, conclusions or recommendations. -

Pneumonia: Prevention and Care at Home
FACT SHEET FOR PATIENTS AND FAMILIES Pneumonia: Prevention and Care at Home What is it? On an x-ray, pneumonia usually shows up as Pneumonia is an infection of the lungs. The infection white areas in the affected part of your lung(s). causes the small air sacs in your lungs (called alveoli) to swell and fill up with fluid or pus. This makes it harder for you to breathe, and usually causes coughing and other symptoms that sap your energy and appetite. How common and serious is it? Pneumonia is fairly common in the United States, affecting about 4 million people a year. Although for many people infection can be mild, about 1 out of every 5 people with pneumonia needs to be in the heart hospital. Pneumonia is most serious in these people: • Young children (ages 2 years and younger) • Older adults (ages 65 and older) • People with chronic illnesses such as diabetes What are the symptoms? and heart disease Pneumonia symptoms range in severity, and often • People with lung diseases such as asthma, mimic the symptoms of a bad cold or the flu: cystic fibrosis, or emphysema • Fatigue (feeling tired and weak) • People with weakened immune systems • Cough, without or without mucus • Smokers and heavy drinkers • Fever over 100ºF or 37.8ºC If you’ve been diagnosed with pneumonia, you should • Chills, sweats, or body aches take it seriously and follow your doctor’s advice. If your • Shortness of breath doctor decides you need to be in the hospital, you will receive more information on what to expect with • Chest pain or pain with breathing hospital care. -

Guinea Pig Care
Caring for your Guinea Pig Basic HusBandry General Information Vital Statistics Guinea Pig Body Weight: Male 900g–1,2000g; Female 700–900g Life Span: Average 4–5 years; Maximum 8 years Sexual Maturity: Male 3–4 months of age; Female 2–3 months of age Behavior and Handling • Guinea pigs should be held gently with two hands. Their hind end should always be supported. • When handling guinea pigs, try to avoid excessive noise, needless excitement, and over-handling. • Children handling the guinea pig should sit on the floor and hold the guinea pig in their lap. Children should only handle guinea pigs under adult supervision. • Guinea pigs do not adapt well to changes in their food or environment. Hair barbering (chewing of the fur) may occur in situations of stress and overcrowding. If this occurs please contact your veterinarian. Reproductive Information • It is extremely important not to let your female guinea pig breed as she reaches six months of age. At around this age, the bones of the pelvis fuse if the animal has not been bred. If a guinea pig in this condition becomes pregnant, she will most likely require high risk surgery to remove the babies. • Guinea pigs are social animals and will establish a pecking order that is frequently male-dominated. Overcrowding may incite aggression among guinea pigs, and noncastrated males may be aggressive towards other males in the presence of females. • Guinea pigs should be kept as single pets, or should be kept in separate cages. Housing • Guinea pigs should be housed separately in a cage that is a minimum of 2 ft. -

Bovine Respiratory Disease & Diagnostic Veterinary Medicine
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Range Beef Cow Symposium Animal Science Department 2009 Bovine Respiratory Disease & Diagnostic Veterinary Medicine (Managing Respiratory Diseases in the Herd) Donald Montgomery Wyoming State Veterinary Laboratory, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/rangebeefcowsymp Part of the Animal Sciences Commons Montgomery, Donald, "Bovine Respiratory Disease & Diagnostic Veterinary Medicine (Managing Respiratory Diseases in the Herd)" (2009). Range Beef Cow Symposium. 280. https://digitalcommons.unl.edu/rangebeefcowsymp/280 This Article is brought to you for free and open access by the Animal Science Department at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Range Beef Cow Symposium by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Proceedings, The Range Beef Cow Symposium XXI December 1, 2 and 3 2009, Casper, WY Bovine Respiratory Disease & Diagnostic Veterinary Medicine (Managing Respiratory Diseases in the Herd) Donald Montgomery, DVM, PhD, Dipl ACVP Pathologist and Director, Wyoming State Veterinary Laboratory Year in and year out, diseases of the respiratory system are a major cause of illness and death in cattle from 6 weeks to two years of age. Sadly, this is as true today as it was 30 years ago despite development of new and improved vaccines, new broad spectrum antibiotics, and increased fundamental knowledge as to the cause of disease. WHY? I don‟t have the answer and I doubt if anyone does. As a pathologist, I often see firsthand the devastating effects that bacteria can have in the lungs of cattle that die from respiratory disease complex or shipping fever. -

Can Animal Models Really Teach Us Anything About Pneumonia? Pro
EDITORIAL | PRO/CON DEBATE Can animal models really teach us anything about pneumonia? Pro Carlos J. Orihuela1, Ulrich A. Maus2,3 and Jeremy S. Brown4 Affiliations: 1Dept of Microbiology, University of Alabama at Birmingham, Birmingham, AL, USA. 2Dept of Experimental Pneumology, Hannover School of Medicine, Hannover, Germany. 3German Center for Lung Research, Hannover, Germany. 4UCL Respiratory, University College London, London, UK. Correspondence: Jeremy S. Brown, UCL Respiratory, University College London, Rayne Building, 5 University Street, London, UK. E-mail: [email protected] @ERSpublications Animal models can provide incredibly detailed data on pathogenesis and immunology of lung infections, and will be essential for the development of novel therapeutic/preventative strategies to reduce the morbidity and mortality caused by pneumonia http://bit.ly/2pdCzcH Cite this article as: Orihuela CJ, Maus UA, Brown JS. Can animal models really teach us anything about pneumonia? Pro. Eur Respir J 2020; 55: 1901539 [https://doi.org/10.1183/13993003.01539-2019]. Introduction Despite highly effective antibiotics and intensive care support, the mortality associated with pneumonia has not substantially decreased since the 1960s [1]. Hence, there remains a major requirement for improved treatment and preventative strategies, which will need new knowledge on the pathogenesis of pneumonia. Animal models have obvious high value when investigating the molecular mechanisms involved in pneumonia pathogenesis, but they are also directly relevant for clinically orientated research into new therapies and vaccines, complications of pneumonia, and identifying high risk groups. In this article we describe how research using animal models will be essential if we are to reduce the immense morbidity and mortality associated with pneumonia. -

Mucosal Immunology of Acute Bacterial Pneumonia
Mucosal Immunology of Acute Bacterial Pneumonia Alice Prince Editor Mucosal Immunology of Acute Bacterial Pneumonia Editor Alice Prince Columbia University New York , NY, USA ISBN 978-1-4614-5325-3 ISBN 978-1-4614-5326-0 (eBook) DOI 10.1007/978-1-4614-5326-0 Springer New York Heidelberg Dordrecht London Library of Congress Control Number: 2012951432 © Springer Science+Business Media New York 2013 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, speci fi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on micro fi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied speci fi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Duplication of this publication or parts thereof is permitted only under the provisions of the Copyright Law of the Publisher’s location, in its current version, and permission for use must always be obtained from Springer. Permissions for use may be obtained through RightsLink at the Copyright Clearance Center. Violations are liable to prosecution under the respective Copyright Law. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a speci fi c statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. -

Top 20 Pneumonia Facts—2019
American Thoracic Society Top 20 Pneumonia Facts—2019 1. Pneumonia is an infection of the lung. The lungs fill 12. Antibiotics can be effective for many of the bacteria with fluid and make breathing difficult. Pneumonia that cause pneumonia. For viral causes of pneumonia, disproportionately affects the young, the elderly, and antibiotics are ineffective and should not be used. There are the immunocompromised. It preys on weakness and few or no treatments for most viral causes of pneumonia. vulnerability. 13. Antibiotic resistance is growing amongst the bacteria 2. Pneumonia is the world’s leading cause of death among that cause pneumonia. This often arises from the overuse children under 5 years of age, accounting for 16% of all and misuse of antibiotics in and out of the hospital. New deaths of children under 5 years old killing approximately and more effective antibiotics are urgently needed. 2,400 children a day in 2015. There are 120 million episodes 14. Being on a ventilator raises especially high risk for of pneumonia per year in children under 5, over 10% of serious pneumonia. Ventilator-associated pneumonia is which (14 million) progress to severe episodes. There was an more likely to be caused by antibiotic-resistant microbes estimated 880,000 deaths from pneumonia in children under and can require the highest antibiotic use in the critically ill the age of five in 2016. Most were less than 2 years of age. population. 3. In the US, pneumonia is less often fatal for children, but 15. Our changing interactions with the microbial world mean it is still a big problem. -

IDSA/ATS Consensus Guidelines on The
SUPPLEMENT ARTICLE Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults Lionel A. Mandell,1,a Richard G. Wunderink,2,a Antonio Anzueto,3,4 John G. Bartlett,7 G. Douglas Campbell,8 Nathan C. Dean,9,10 Scott F. Dowell,11 Thomas M. File, Jr.12,13 Daniel M. Musher,5,6 Michael S. Niederman,14,15 Antonio Torres,16 and Cynthia G. Whitney11 1McMaster University Medical School, Hamilton, Ontario, Canada; 2Northwestern University Feinberg School of Medicine, Chicago, Illinois; 3University of Texas Health Science Center and 4South Texas Veterans Health Care System, San Antonio, and 5Michael E. DeBakey Veterans Affairs Medical Center and 6Baylor College of Medicine, Houston, Texas; 7Johns Hopkins University School of Medicine, Baltimore, Maryland; 8Division of Pulmonary, Critical Care, and Sleep Medicine, University of Mississippi School of Medicine, Jackson; 9Division of Pulmonary and Critical Care Medicine, LDS Hospital, and 10University of Utah, Salt Lake City, Utah; 11Centers for Disease Control and Prevention, Atlanta, Georgia; 12Northeastern Ohio Universities College of Medicine, Rootstown, and 13Summa Health System, Akron, Ohio; 14State University of New York at Stony Brook, Stony Brook, and 15Department of Medicine, Winthrop University Hospital, Mineola, New York; and 16Cap de Servei de Pneumologia i Alle`rgia Respirato`ria, Institut Clı´nic del To`rax, Hospital Clı´nic de Barcelona, Facultat de Medicina, Universitat de Barcelona, Institut d’Investigacions Biome`diques August Pi i Sunyer, CIBER CB06/06/0028, Barcelona, Spain. EXECUTIVE SUMMARY priate starting point for consultation by specialists. Substantial overlap exists among the patients whom Improving the care of adult patients with community- these guidelines address and those discussed in the re- acquired pneumonia (CAP) has been the focus of many cently published guidelines for health care–associated different organizations, and several have developed pneumonia (HCAP). -

Bronchitis and Pneumonia
Fact Sheets for Families Bronchitis and Pneumonia Children in child care settings are often sick with upper bacteria, in which case antibiotics are the treatment of respiratory infections. The rates of these infections are choice. When pneumonia is caused by bacteria, an in- higher in the winter months, although they can occur fected child usually becomes sick relatively quickly and any time of the year. Some side effects of upper respi- experiences the sudden onset of high fever and rapid ratory infections, such as colds or flu, are bronchitis breathing When these infections are caused by a virus, and pneumonia. such as RSV, adenovirous, or influenza, antibiotics will not help and most often the infection will have to run its What is the difference between course. Bronchitis and pneumonia both require the care bronchitis and pneumonia? and supervision of a health care profes- Bronchitis is most often a bacterial or sional, as children with pneumonia viral infection that causes swelling can become sick enough to require of the tubes (bronchioles) leading hospitalization. to the lungs. Pneumonia is an acute or chronic disease marked When can children by inflammation of the lungs and return to child care? is caused by viruses, bacteria, With treatment, most types of other organisms and sometimes bacterial pneumonia can be by physical or chemical irritants. cured within 1 to 2 weeks. Viral A diagnosis of “double pneumo- pneumonia may last longer. Chil- nia” means both lungs have been dren recovering from bronchitis affected. “Walking pneumonia” or pneumonia can return to the means that the illness is not serious child care program provided enough to require hospitalization they are feeling well enough to of the child or adult; it is generally participate, are free of fever, and caused by a germ called mycoplasma. -

Pneumonia | Lung Inflammation
Pneumonia Pneumonia is an infection that causes inflammation in one or both of the lungs and may be caused by a virus, bacteria, fungi or other germs. Your doctor may conduct a physical exam and use chest x-ray, chest CT, chest ultrasound, or needle biopsy of the lung to help diagnose your condition. Your doctor may further evaluate your condition and lung function using thoracentesis, chest tube placement or image-guided abscess drainage. × Looking for information on coronavirus (COVID-19)? See the Coronavirus (COVID-19) (http://www.radiologyinfo.org/info/psa-coronavirus) page. What is pneumonia? Pneumonia is an infection that causes inflammation in one or both of the lungs. It can be caused by a virus, bacteria, fungi or other germs. The infection is usually acquired when a person breathes in air carrying germs. Patients with pneumonia could have the following symptoms: cough that produces phlegm or sometimes blood fever shortness of breath or difficulty breathing chills or shaking fatigue sweating chest or muscle pain Those most at risk for developing pneumonia are young children or people over the age of 65. People with existing health problems are also at increased risk. Risk factors and circumstances that may increase a person's chances of developing pneumonia include: having illnesses such as emphysema, HIV/AIDS or other lung diseases or conditions that affect the immune system having the flu exposure to and inhalation of various chemicals smoking or excessive drinking a prolonged stay in the hospital or intensive care recent surgery Pneumonia Page 1 of 3 Copyright© 2021, RadiologyInfo.org Reviewed Feb-8-2021 recent injury Pneumonia can sometimes lead to serious complications, such as respiratory system failure, spread of infections, fluid surrounding the lungs, abscesses or uncontrolled inflammation throughout the body (sepsis). -

Pneumonia Panel
Guidance on Use of the Pneumonia Panel for Respiratory Infections Although the number of pathogens that cause pneumonia is lengthy, establishing the microbiologic etiology of pneumonia is inherently difficult. A recent large multi-center study of community-acquired pneumonia (CAP) found that only 38% of 2259 CAP cases had a microbiologic diagnosis with 23% having viruses detected, 11% bacterial, and 3% had both viruses and bacteria detected.1 Current tools to assist in pneumonia diagnosis include respiratory tract cultures (sputum, BAL, tracheal aspirate, mini-BAL), urine antigens (pneumococcal, Legionella), serology, and PCR for viral and certain bacterial pathogens. While these tools are useful, the study noted above used all these tools and was unable to document an etiology causing pneumonia in 62% of patients. Thus, more sensitive tools for detection of respiratory pathogens are still needed. Nebraska Medicine has recently introduced a new FDA-approved multiplex PCR panel to assist in determination of the etiology of pneumonia, termed the Pneumonia Panel (PP). This test uses a nested multiplex PCR- approach to amplify nucleic acid targets directly from sputum or bronchoalveolar lavage (BAL) in patients with suspected pneumonia. The list of pathogens and resistance genes included in the panel is found in Table 1. Note that the bacterial targets are detected semi-quantitatively whereas the atypical pathogens and the viral targets are detected qualitatively. Table 1: Pneumonia Panel Pathogen Targets and Associated Resistance Genes Semi-quantitative Detection: Gram Positive Organisms: Resistance Genes (Staph aureus only): Staphylococcus aureus mecA/C and MREJ Streptococcus pneumoniae Streptococcus agalactiae Streptococcus pyogenes Gram Negative Organisms: Resistance Genes (All Gram Negatives): Acinetobacter calcoaceticus-baumannii complex CTX-M Enterobacter cloacae complex IMP E.