Pneumonia What Is Pneumonia?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Captive Orcas
Captive Orcas ‘Dying to Entertain You’ The Full Story A report for Whale and Dolphin Conservation Society (WDCS) Chippenham, UK Produced by Vanessa Williams Contents Introduction Section 1 The showbiz orca Section 2 Life in the wild FINgerprinting techniques. Community living. Social behaviour. Intelligence. Communication. Orca studies in other parts of the world. Fact file. Latest news on northern/southern residents. Section 3 The world orca trade Capture sites and methods. Legislation. Holding areas [USA/Canada /Iceland/Japan]. Effects of capture upon remaining animals. Potential future capture sites. Transport from the wild. Transport from tank to tank. “Orca laundering”. Breeding loan. Special deals. Section 4 Life in the tank Standards and regulations for captive display [USA/Canada/UK/Japan]. Conditions in captivity: Pool size. Pool design and water quality. Feeding. Acoustics and ambient noise. Social composition and companionship. Solitary confinement. Health of captive orcas: Survival rates and longevity. Causes of death. Stress. Aggressive behaviour towards other orcas. Aggression towards trainers. Section 5 Marine park myths Education. Conservation. Captive breeding. Research. Section 6 The display industry makes a killing Marketing the image. Lobbying. Dubious bedfellows. Drive fisheries. Over-capturing. Section 7 The times they are a-changing The future of marine parks. Changing climate of public opinion. Ethics. Alternatives to display. Whale watching. Cetacean-free facilities. Future of current captives. Release programmes. Section 8 Conclusions and recommendations Appendix: Location of current captives, and details of wild-caught orcas References The information contained in this report is believed to be correct at the time of last publication: 30th April 2001. Some information is inevitably date-sensitive: please notify the author with any comments or updated information. -

Allergic Bronchopulmonary Aspergillosis Masquerading As Recurrent Bacterial Pneumonia
Medical Mycology Case Reports 12 (2016) 11–13 Contents lists available at ScienceDirect Medical Mycology Case Reports journal homepage: www.elsevier.com/locate/mmcr Allergic Bronchopulmonary Aspergillosis masquerading as recurrent bacterial pneumonia Vu Le Thuong, Lam Nguyen Ho n, Ngoc Tran Van University of Medicine and Pharmacy – Ho Chi Minh city, 217 Hong Bang, Ward 11st, Dist 5, Ho Chi Minh city 70000, Vietnam article info abstract Article history: Allergic Bronchopulmonary Aspergillosis (ABPA) can be diagnosed in an asthmatic with suitable radi- Received 15 May 2016 ologic and immunological features. However ABPA is likely to be misdiagnosed with bacterial pneu- Accepted 26 June 2016 monia. Here we report a case of ABPA masquerading as recurrent bacterial pneumonia. Treatment with Available online 27 June 2016 high-dose inhaled corticosteroids was effective. To our best knowledge, this is the first reported case of Keywords: ABPA in Vietnam. Allergic bronchopulmonary aspergillosis & 2016 International Society for Human and Animal Mycology. International Society for Human and Asthma Animal Mycology Published by Elsevier B.V. All rights reserved. Inhaled corticosteroids Pneumonia Pulmonary tuberculosis 1. Introduction À120), he complained of cough and his chest X ray (CXR) showed right perihilar airspace opacities (Fig. 1A). He was diagnosed and Allergic Bronchopulmonary Aspergillosis (ABPA) is the hy- treated as a bacterial pneumonia. His cough improved and his CXR persensitive status of airway to Aspergillus which colonizes the (on day À30) came back almost normal three months later bronchial mucosa, occurring mainly in patients with asthma or (Fig. 1B). cystic fibrosis. The diagnostic criteria for ABPA articulated by Ro- Subsequently, he had a 10- day history of coughing up white- senberg, and later revised by Greenberger, has been widely used cloudy and viscous sputum before admission. -

The Use of Non-Human Primates in Research in Primates Non-Human of Use The
The use of non-human primates in research The use of non-human primates in research A working group report chaired by Sir David Weatherall FRS FMedSci Report sponsored by: Academy of Medical Sciences Medical Research Council The Royal Society Wellcome Trust 10 Carlton House Terrace 20 Park Crescent 6-9 Carlton House Terrace 215 Euston Road London, SW1Y 5AH London, W1B 1AL London, SW1Y 5AG London, NW1 2BE December 2006 December Tel: +44(0)20 7969 5288 Tel: +44(0)20 7636 5422 Tel: +44(0)20 7451 2590 Tel: +44(0)20 7611 8888 Fax: +44(0)20 7969 5298 Fax: +44(0)20 7436 6179 Fax: +44(0)20 7451 2692 Fax: +44(0)20 7611 8545 Email: E-mail: E-mail: E-mail: [email protected] [email protected] [email protected] [email protected] Web: www.acmedsci.ac.uk Web: www.mrc.ac.uk Web: www.royalsoc.ac.uk Web: www.wellcome.ac.uk December 2006 The use of non-human primates in research A working group report chaired by Sir David Weatheall FRS FMedSci December 2006 Sponsors’ statement The use of non-human primates continues to be one the most contentious areas of biological and medical research. The publication of this independent report into the scientific basis for the past, current and future role of non-human primates in research is both a necessary and timely contribution to the debate. We emphasise that members of the working group have worked independently of the four sponsoring organisations. Our organisations did not provide input into the report’s content, conclusions or recommendations. -

Pneumonia: Prevention and Care at Home
FACT SHEET FOR PATIENTS AND FAMILIES Pneumonia: Prevention and Care at Home What is it? On an x-ray, pneumonia usually shows up as Pneumonia is an infection of the lungs. The infection white areas in the affected part of your lung(s). causes the small air sacs in your lungs (called alveoli) to swell and fill up with fluid or pus. This makes it harder for you to breathe, and usually causes coughing and other symptoms that sap your energy and appetite. How common and serious is it? Pneumonia is fairly common in the United States, affecting about 4 million people a year. Although for many people infection can be mild, about 1 out of every 5 people with pneumonia needs to be in the heart hospital. Pneumonia is most serious in these people: • Young children (ages 2 years and younger) • Older adults (ages 65 and older) • People with chronic illnesses such as diabetes What are the symptoms? and heart disease Pneumonia symptoms range in severity, and often • People with lung diseases such as asthma, mimic the symptoms of a bad cold or the flu: cystic fibrosis, or emphysema • Fatigue (feeling tired and weak) • People with weakened immune systems • Cough, without or without mucus • Smokers and heavy drinkers • Fever over 100ºF or 37.8ºC If you’ve been diagnosed with pneumonia, you should • Chills, sweats, or body aches take it seriously and follow your doctor’s advice. If your • Shortness of breath doctor decides you need to be in the hospital, you will receive more information on what to expect with • Chest pain or pain with breathing hospital care. -
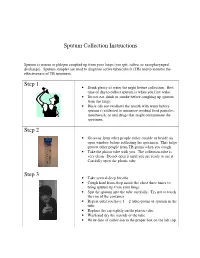
Sputum Collection Instructions Step 1 Step 2 Step 3
Sputum Collection Instructions Sputum is mucus or phlegm coughed up from your lungs (not spit, saliva, or nasopharyngeal discharge). Sputum samples are used to diagnose active tuberculosis (TB) and to monitor the effectiveness of TB treatment. Step 1 • Drink plenty of water the night before collection. Best time of day to collect sputum is when you first wake. • Do not eat, drink or smoke before coughing up sputum from the lungs. • Rinse (do not swallow) the mouth with water before sputum is collected to minimize residual food particles, mouthwash, or oral drugs that might contaminate the specimen. Step 2 • Go away from other people either outside or beside an open window before collecting the specimen. This helps protect other people from TB germs when you cough. • Take the plastic tube with you. The collection tube is very clean. Do not open it until you are ready to use it. Carefully open the plastic tube. Step 3 • Take several deep breaths. • Cough hard from deep inside the chest three times to bring sputum up from your lungs. • Spit the sputum into the tube carefully. Try not to touch the rim of the container. • Repeat until you have 1 – 2 tablespoons of sputum in the tube. • Replace the cap tightly on the plastic tube. • Wash and dry the outside of the tube. • Write date of collection in the proper box on the lab slip. Step 4 • Place the primary specimen container (usually a conical centrifuge tube) in the clear plastic baggie that has the biohazard symbol imprint. • Place the white absorbent sheet in the plastic baggie. -

Perinatal/Neonatal Case Presentation
Perinatal/Neonatal Case Presentation &&&&&&&&&&&&&& Urinary Tract Infection With Trichomonas vaginalis in a Premature Newborn Infant and the Development of Chronic Lung Disease David J. Hoffman, MD vaginal bleeding with suspected abruption resulted in delivery of Gerard D. Brown, DO the infant by Cesarean section. The Apgar scores were 1, 5, and 9 Frederick H. Wirth, MD at 1, 5, and 10 minutes of life, respectively. Betsy S. Gebert, CRNP After delivery, the infant was managed with mechanical Cathy L. Bailey, MS, CRNP ventilation with pressure support and volume guarantee for Endla K. Anday, MD respiratory distress syndrome. She received exogenous surfactant We report a case of a low-birth-weight infant with an infection of the urinary tract with Trichomonas vaginalis, who later developed cystic chronic lung disease suggestive of Wilson-Mikity syndrome. Although she had mild respiratory distress syndrome at birth, the extent of the chronic lung disease was out of proportion to the initial illness. We speculate that maternal infection with this organism may have resulted in an inflammatory response that led to its development. Journal of Perinatology (2003) 23, 59 – 61 doi:10.1038/sj.jp.7210819 CASE PRESENTATION A 956-g, appropriate-for-gestational-age, African–American female was delivered by Cesarean section following 27 5/7 weeks of gestation in breech presentation after a period of advanced cervical dilatation and uterine contractions. Her mother was a 20-year-old gravida 5, para 2022 woman whose prenatal laboratory data were significant for vaginal colonization with Streptococcus agalactiae, treatment for Chlamydia trachomatis, and a history of cocaine and marijuana usage confirmed by urine toxicology. -

Guinea Pig Care
Caring for your Guinea Pig Basic HusBandry General Information Vital Statistics Guinea Pig Body Weight: Male 900g–1,2000g; Female 700–900g Life Span: Average 4–5 years; Maximum 8 years Sexual Maturity: Male 3–4 months of age; Female 2–3 months of age Behavior and Handling • Guinea pigs should be held gently with two hands. Their hind end should always be supported. • When handling guinea pigs, try to avoid excessive noise, needless excitement, and over-handling. • Children handling the guinea pig should sit on the floor and hold the guinea pig in their lap. Children should only handle guinea pigs under adult supervision. • Guinea pigs do not adapt well to changes in their food or environment. Hair barbering (chewing of the fur) may occur in situations of stress and overcrowding. If this occurs please contact your veterinarian. Reproductive Information • It is extremely important not to let your female guinea pig breed as she reaches six months of age. At around this age, the bones of the pelvis fuse if the animal has not been bred. If a guinea pig in this condition becomes pregnant, she will most likely require high risk surgery to remove the babies. • Guinea pigs are social animals and will establish a pecking order that is frequently male-dominated. Overcrowding may incite aggression among guinea pigs, and noncastrated males may be aggressive towards other males in the presence of females. • Guinea pigs should be kept as single pets, or should be kept in separate cages. Housing • Guinea pigs should be housed separately in a cage that is a minimum of 2 ft. -

Bovine Respiratory Disease & Diagnostic Veterinary Medicine
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Range Beef Cow Symposium Animal Science Department 2009 Bovine Respiratory Disease & Diagnostic Veterinary Medicine (Managing Respiratory Diseases in the Herd) Donald Montgomery Wyoming State Veterinary Laboratory, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/rangebeefcowsymp Part of the Animal Sciences Commons Montgomery, Donald, "Bovine Respiratory Disease & Diagnostic Veterinary Medicine (Managing Respiratory Diseases in the Herd)" (2009). Range Beef Cow Symposium. 280. https://digitalcommons.unl.edu/rangebeefcowsymp/280 This Article is brought to you for free and open access by the Animal Science Department at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Range Beef Cow Symposium by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Proceedings, The Range Beef Cow Symposium XXI December 1, 2 and 3 2009, Casper, WY Bovine Respiratory Disease & Diagnostic Veterinary Medicine (Managing Respiratory Diseases in the Herd) Donald Montgomery, DVM, PhD, Dipl ACVP Pathologist and Director, Wyoming State Veterinary Laboratory Year in and year out, diseases of the respiratory system are a major cause of illness and death in cattle from 6 weeks to two years of age. Sadly, this is as true today as it was 30 years ago despite development of new and improved vaccines, new broad spectrum antibiotics, and increased fundamental knowledge as to the cause of disease. WHY? I don‟t have the answer and I doubt if anyone does. As a pathologist, I often see firsthand the devastating effects that bacteria can have in the lungs of cattle that die from respiratory disease complex or shipping fever. -

Chest Pain in Pediatrics
PEDIATRIC CARDIOLOGY 0031-3955/99 $8.00 + .OO CHEST PAIN IN PEDIATRICS Keith C. Kocis, MD, MS Chest pain is an alarming complaint in children, leading an often frightened and concerned family to a pediatrician or emergency room and commonly to a subsequent referral to a pediatric cardiologist. Because of the well-known associ- ation of chest pain with significant cardiovascular disease and sudden death in adult patients, medical personnel commonly share heightened concerns over pediatric patients presenting with chest pain. Although the differential diagnosis of chest pain is exhaustive, chest pain in children is least likely to be cardiac in origin. Organ systems responsible for causing chest pain in children include*: Idiopathic (12%-85%) Musculoskeletal (15%-31%) Pulmonary (12%-21%) Other (4%-21%) Psychiatric (5%-17%) Gastrointestinal (4'/0-7%) Cardiac (4%4%) Furthermore, chest pain in the pediatric population is rareZy associated with life-threatening disease; however, when present, prompt recognition, diagnostic evaluation, and intervention are necessary to prevent an adverse outcome. This article presents a comprehensive list of differential diagnostic possibilities of chest pain in pediatric patients, discusses the common causes in further detail, and outlines a rational diagnostic evaluation and treatment plan. Chest pain, a common complaint of pediatric patients, is often idiopathic in etiology and commonly chronic in nature. In one study,67 chest pain accounted for 6 in 1000 visits to an urban pediatric emergency room. In addition, chest pain is the second most common reason for referral to pediatric cardiologist^.^, 23, 78 Chest pain is found equally in male and female patients, with an average *References 13, 17, 23, 27, 32, 35, 44, 48, 49, 63-67, 74, and 78. -

Can Animal Models Really Teach Us Anything About Pneumonia? Pro
EDITORIAL | PRO/CON DEBATE Can animal models really teach us anything about pneumonia? Pro Carlos J. Orihuela1, Ulrich A. Maus2,3 and Jeremy S. Brown4 Affiliations: 1Dept of Microbiology, University of Alabama at Birmingham, Birmingham, AL, USA. 2Dept of Experimental Pneumology, Hannover School of Medicine, Hannover, Germany. 3German Center for Lung Research, Hannover, Germany. 4UCL Respiratory, University College London, London, UK. Correspondence: Jeremy S. Brown, UCL Respiratory, University College London, Rayne Building, 5 University Street, London, UK. E-mail: [email protected] @ERSpublications Animal models can provide incredibly detailed data on pathogenesis and immunology of lung infections, and will be essential for the development of novel therapeutic/preventative strategies to reduce the morbidity and mortality caused by pneumonia http://bit.ly/2pdCzcH Cite this article as: Orihuela CJ, Maus UA, Brown JS. Can animal models really teach us anything about pneumonia? Pro. Eur Respir J 2020; 55: 1901539 [https://doi.org/10.1183/13993003.01539-2019]. Introduction Despite highly effective antibiotics and intensive care support, the mortality associated with pneumonia has not substantially decreased since the 1960s [1]. Hence, there remains a major requirement for improved treatment and preventative strategies, which will need new knowledge on the pathogenesis of pneumonia. Animal models have obvious high value when investigating the molecular mechanisms involved in pneumonia pathogenesis, but they are also directly relevant for clinically orientated research into new therapies and vaccines, complications of pneumonia, and identifying high risk groups. In this article we describe how research using animal models will be essential if we are to reduce the immense morbidity and mortality associated with pneumonia. -

PNEUMONIAS Pneumonia Is Defined As Acute Inflammation of the Lung
PNEUMONIAS Pneumonia is defined as acute inflammation of the lung parenchyma distal to the terminal bronchioles which consist of the respiratory bronchiole, alveolar ducts, alveolar sacs and alveoli. The terms 'pneumonia' and 'pneumonitis' are often used synonymously for in- flammation of the lungs, while 'consolidation' (meaning solidification) is the term used for macroscopic and radiologic appearance of the lungs in pneumonia. PATHOGENESIS. The microorganisms gain entry into the lungs by one of the following four routes: 1. Inhalation of the microbes. 2. Aspiration of organisms. 3. Haematogenous spread from a distant focus. 4. Direct spread from an adjoining site of infection. Failure of defense me- chanisms and presence of certain predisposing factors result in pneumonias. These condi- tions are as under: 1. Altered consciousness. 2. Depressed cough and glottic reflexes. 3. Impaired mucociliary transport. 4. Impaired alveolar macrophage function. 5. Endo- bronchial obstruction. 6. Leucocyte dysfunctions. CLASSIFICATION. On the basis of the anatomic part of the lung parenchyma involved, pneumonias are traditionally classified into 3 main types: 1. Lobar pneumonia. 2. Bronchopneumonia (or Lobular pneumonia). 3. Interstitial pneumonia. A. BACTERIAL PNEUMONIA Bacterial infection of the lung parenchyma is the most common cause of pneumonia or consolidation of one or both the lungs. Two types of acute bacterial pneumonias are dis- tinguished—lobar pneumonia and broncho-lobular pneumonia, each with distinct etiologic agent and morphologic changes. 1. Lobar Pneumonia Lobar pneumonia is an acute bacterial infection of a part of a lobe, the entire lobe, or even two lobes of one or both the lungs. ETIOLOGY. Following types are described: 1. -

Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT
University of Nebraska Medical Center DigitalCommons@UNMC Theses & Dissertations Graduate Studies Fall 12-18-2015 Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT Christopher C. Schultz University of Nebraska Medical Center Follow this and additional works at: https://digitalcommons.unmc.edu/etd Part of the Other Medical Specialties Commons Recommended Citation Schultz, Christopher C., "Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT" (2015). Theses & Dissertations. 54. https://digitalcommons.unmc.edu/etd/54 This Thesis is brought to you for free and open access by the Graduate Studies at DigitalCommons@UNMC. It has been accepted for inclusion in Theses & Dissertations by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. EVALUATION OF UPPER AIRWAY CHANGES FOLLOWING SURGICAL REMOVAL OF THE ADENOIDS USING 3-D CONE BEAM CT By Christopher C. Schultz, D.D.S A THESIS Presented to the Faculty of The Graduate College in the University of Nebraska In Partial Fulfillment of Requirements For the Degree of Master of Science Medical Sciences Interdepartmental Area Oral Biology University of Nebraska Medical Center Omaha, Nebraska December, 2015 Advisory Committee: Sundaralingam Premaraj, BDS, MS, PhD, FRCD(C) Sheela Premaraj, BDS, PhD Peter J. Giannini, DDS, MS Stanton D. Harn, PhD i ACKNOWLEDGEMENTS I would like to express my thanks and gratitude to the members of my thesis committee: Dr. Sundaralingam Premaraj, Dr. Sheela Premaraj, Dr. Peter Giannini, and Dr. Stanton Harn. Your advice and assistance has been vital for the completion of the project.