Myths and Facts About Immunization
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-
Values, Justifications, and Perspectives Connected to the Anti-Vaccination Movement Gigi Garzio [email protected]
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Sound Ideas University of Puget Sound Sound Ideas Summer Research Summer 2018 Values, Justifications, and Perspectives Connected to the Anti-Vaccination Movement Gigi Garzio [email protected] Follow this and additional works at: https://soundideas.pugetsound.edu/summer_research Part of the Anthropology Commons, and the Medicine and Health Commons Recommended Citation Garzio, Gigi, "Values, Justifications, and Perspectives Connected to the Anti-Vaccination Movement" (2018). Summer Research. 309. https://soundideas.pugetsound.edu/summer_research/309 This Article is brought to you for free and open access by Sound Ideas. It has been accepted for inclusion in Summer Research by an authorized administrator of Sound Ideas. For more information, please contact [email protected]. Introduction Throughout the 18th and 19th centuries, when the first smallpox outbreak began and the first vaccine was introduced, there has been vaccine skepticism (Offit, 2015). Smallpox outbreaks, and the fatalities that come with it, continued to spread around the world despite the development of the vaccine. However, between the 1940s and the early 1970s, anti-vaccine sentiment declined due to “three trends: a boom in vaccine science, discovery, and manufacture; public awareness of widespread outbreaks of infectious diseases (measles, mumps, rubella, pertussis, polio, and others) and the desire to protect children from these highly prevalent ills; and a baby boom, accompanied by increasing levels of education and wealth” (Poland et al, 2011). These factors led to general public acceptance of vaccines, which resulted in significant decreases in disease outbreaks. However, with less visible outbreaks of disease and more vaccines being added to the childhood vaccination schedule, the presence of the anti-vaccination movement returned in the 1970s (Wolfe, 2002). -

Vaccines and Autism: What You Should Know | Vaccine Education
Q A Vaccines and Autism: What you should know Volume& 1 Summer 2008 Some parents of children with autism are concerned that vaccines are the cause. Their concerns center on three areas: the combination measles-mumps-rubella (MMR) vaccine; thimerosal, a mercury-containing preservative previously contained in several vaccines; and the notion that babies receive too many vaccines too soon. Q. What are the symptoms of autism? Q. Does the MMR vaccine cause autism? A. Symptoms of autism, which typically appear during the A. No. In 1998, a British researcher named Andrew Wakefi eld fi rst few years of life, include diffi culties with behavior, social raised the notion that the MMR vaccine might cause autism. skills and communication. Specifi cally, children with autism In the medical journal The Lancet, he reported the stories of may have diffi culty interacting socially with parents, siblings eight children who developed autism and intestinal problems and other people; have diffi culty with transitions and need soon after receiving the MMR vaccine. To determine whether routine; engage in repetitive behaviors such as hand fl apping Wakefi eld’s suspicion was correct, researchers performed or rocking; display a preoccupation with activities or toys; a series of studies comparing hundreds of thousands of and suffer a heightened sensitivity to noise and sounds. children who had received the MMR vaccine with hundreds Autism spectrum disorders vary in the type and severity of of thousands who had never received the vaccine. They found the symptoms they cause, so two children with autism may that the risk of autism was the same in both groups. -

Science Reporting Syllabus: Covering the Environment, Technology and Medicine
1 Science reporting syllabus: Covering the environment, technology and medicine Science reporting is in a moment of extreme transition: Popular science writing is experiencing a renaissance at precisely the moment that traditional media outlets are jettisoning specialized reporters. This creates tremendous opportunity and tremendous challenges. This course makes sure students are prepared to meet those challenges. Course objective This course is designed to acquaint reporters with all aspects of science reporting and writing. It will train participants to view new breakthroughs and discoveries with skepticism and will give students a working knowledge of many of the main areas of science coverage, including the environment, artificial intelligence, and human interaction with technology. There will be lessons on social media, online writing, news and feature writing, and writing long-form narratives. Learning objectives The syllabus is designed to strengthen students’ core competencies in several areas: Determining what sources and outlets can be trusted to discuss controversial or unproven claims. Learning which questions will elicit meaningful responses. Understanding that choosing not to cover a story can be just as important an editorial decision as deciding how to cover it. Evaluating what type of form a journalist is most comfortable with and seeking out ways to work in that form. Course design This course will focus on developing toolkits for evaluating science stories in addition to learning about some specific issues or controversies. It is designed as a workshop course for between 10 and 15 students. An integral part of the course is analyzing and critiquing other students’ work. Readings Required books Deborah Blum, Mary Knudson and Robin Marantz Henig, editors, A Field Guide for Science Writers, 2005. -

CLINICAL TRIALS Safety and Immunogenicity of a Nicotine Conjugate Vaccine in Current Smokers
CLINICAL TRIALS Safety and immunogenicity of a nicotine conjugate vaccine in current smokers Immunotherapy is a novel potential treatment for nicotine addiction. The aim of this study was to assess the safety and immunogenicity of a nicotine conjugate vaccine, NicVAX, and its effects on smoking behavior. were recruited for a noncessation treatment study and assigned to 1 of 3 doses of the (68 ؍ Smokers (N nicotine vaccine (50, 100, or 200 g) or placebo. They were injected on days 0, 28, 56, and 182 and monitored for a period of 38 weeks. Results showed that the nicotine vaccine was safe and well tolerated. Vaccine immunogenicity was dose-related (P < .001), with the highest dose eliciting antibody concentrations within the anticipated range of efficacy. There was no evidence of compensatory smoking or precipitation of nicotine withdrawal with the nicotine vaccine. The 30-day abstinence rate was significantly different across with the highest rate of abstinence occurring with 200 g. The nicotine vaccine appears ,(02. ؍ the 4 doses (P to be a promising medication for tobacco dependence. (Clin Pharmacol Ther 2005;78:456-67.) Dorothy K. Hatsukami, PhD, Stephen Rennard, MD, Douglas Jorenby, PhD, Michael Fiore, MD, MPH, Joseph Koopmeiners, Arjen de Vos, MD, PhD, Gary Horwith, MD, and Paul R. Pentel, MD Minneapolis, Minn, Omaha, Neb, Madison, Wis, and Rockville, Md Surveys show that, although about 41% of smokers apy, is about 25% on average.2 Moreover, these per- make a quit attempt each year, less than 5% of smokers centages most likely exaggerate the efficacy of are successful at remaining abstinent for 3 months to a intervention because these trials are typically composed year.1 Smokers seeking available behavioral and phar- of subjects who are highly motivated to quit and who macologic therapies can enhance successful quit rates are free of complicating diagnoses such as depression 2 by 2- to 3-fold over control conditions. -
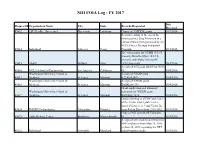
NIH FOIA Log - FY 2017
NIH FOIA Log - FY 2017 Date Request Id Organization Name City State Records Requested Received 45612 LSU Health - Shreveport Shreveport Louisiana Copies of 3 NIDDK grants. 10/3/2016 Records relating to the use of the investigational drug Fostriecin in a human clinical trial sponsored by the NCI's Cancer Therapy Evaluation 45614 Individual Lakeway Texas Program. 10/3/2016 Site visit reports for UTMB (3/1/15- present); Battelle-Ohio (10/1/15- present); and Alpha Genesis-SC 45615 SAEN Milford Ohio (4/1/14-present). 10/3/2016 A copy of NCI grant 1R43CA135915- 45616 UCLA School of Engineering Los Angeles California 01. 10/4/2016 Washington University School of A copy of NIAID grant 45617 Medicine St. Louis Missouri K22AI052407. 10/4/2016 Washington University School of A copy of NHLBI grant 45618 Medicine St. Louis Missouri R01HL081398. 10/4/2016 Grant application and summary Washington University School of statement for NIDDK grant 45619 Medicine St. Louis Missouri K01DK077878. 10/4/2016 Data pertaining to all NIH purchases of the Victor model plate reader (model Victor 1, 2, 3 and Victor X) 45620 IMGEN Technologies Alexandria Virginia from Perkin Elmer from 1999-2012. 10/3/2016 Copy of NEI grant R21EY026438- 45621 Tufts Medical Center Brookline Massachusetts 01. 10/5/2016 A copy of all emails to and from two NIH employees from May 25, 2016 to June 25, 2016 regarding the NTP 45622 Individual Greenbelt Maryland radiofrequency study. 10/5/2016 Date Request Id Organization Name City State Records Requested Received Copies of the RCDC Thesaurus from 45623 Catenion Berlin Other 2010-2014. -

Hearing Before the Committee on Government Reform
DOCUMENT RESUME ED 466 915 EC 309 063 TITLE Autism: Present Challenges, Future Needs--Why the Increased Rates? Hearing before the Committee on Government Reform. House of Representatives, One Hundred Sixth Congress, Second Session (April 6,2000). INSTITUTION Congress of the U.S., Washington, DC. House Committee on Government Reform. REPORT NO House-Hrg-106-180 PUB DATE 2001-00-00 NOTE 483p. AVAILABLE FROM Government Printing Office, Superintendent of Documents, Congressional Sales Office, Washington, DC 20402-9328. Tel: 202-512-1800. For full text: http://www.house.gov/reform. PUB TYPE Legal/Legislative/Regulatory Materials (090) EDRS PRICE EDRS Price MF02/PC20 Plus Postage. DESCRIPTORS *Autism; *Child Health; Children; *Disease Control; *Etiology; Family Problems; Hearings; *Immunization Programs; Incidence; Influences; Parent Attitudes; *Preventive Medicine; Research Needs; Symptoms (Individual Disorders) IDENTIFIERS Congress 106th; Vaccination ABSTRACT This document contains the proceedings of a hearing on April 6, 2000, before the U.S. House of Representatives Committee on Government Reform. The hearing addressed the increasing rate of children diagnosed with autism, possible links between autism and childhood vaccinations, and future needs of these children. After opening statements by congressmen on the Committee, the statements and testimony of Kenneth Curtis, James Smythe, Shelley Reynolds, Jeana Smith, Scott Bono, and Dr. Wayne M. Danker, all parents of children with autism, are included. Their statements discuss symptoms of autism, vaccination concerns, family problems, financial concerns, and how parents can be helped. The statements and testimony of the second panel are then provided, including that of Andrew Wakefield, John O'Leary, Vijendra K. Singh, Coleen A. Boyle, Ben Schwartz, Paul A. -
Solving the Autism Puzzle
Contents Foreword .............................. 4 Saturday (Schedule) .................... 18 Acknowledgments by Sertoma . 5 Poster Session 1: Friday 9:30 am . 20 Purpose of Autism07 .................... 6 Poster Session 2: Friday 3:00 pm . 21 Continuing Education Credit . 9 Poster Session 3: Saturday 9:30 am . 22 Thursday (Schedule).................... 11 Exhibitors............................. 25 Downstairs Floor Plan of the Cajundome Partners............................... 25 Convention Center .................. 11 Advertisers............................ 25 Upstairs floor plan for the Cajundome Planning & Organizing Committee . 25 Convention Center .................. 12 Index of Names & Companies . 26 Friday (Schedule) ..................... 13 Copyright © of this Program for Autism07 by the Sertoma Club of Lafayette 2007 Foreword The autism puzzle is about it? This conference addresses that critical question among the most troubling along with questions about the diagnosis and treatment of of today’s world. Severe autism and related disorders. Autism07 has received the autism robs parent and highest possible rating for continuing education from the child of a normal relation American Medical Association. Qualified participants can with each other. Jon receive up to 13.25 AMA PRA Category 1 CreditsTM . Shestack, the producer of Continuing education is also available to dentists, nurses, Father of the Bride and behavior analysts, psychologists, hygienists, social other Hollywood motion workers, occupational therapists, teachers, and -

Interpersonal Communication for Immunization Training for Front Line Workers
1 Participant manual Interpersonal Communication for Immunization Training for Front Line Workers UNICEF Europe and Central Asia Region 2 Interpersonal Communication for Immunization. Participant manual Participant manual Interpersonal Communication for Immunization Training for Front Line Workers UNICEF Europe and Central Asia Region 4 Interpersonal Communication for Immunization. Participant manual Acknowledgements This training package was developed by the Johns Hopkins Center for Communication Programs, the UNICEF Europe and Central Asia Regional Office, and UNICEF Country Office staff in Bosnia and Herzegovina and Serbia. We would like to thank Sergiu Tomsa, UNICEF Regional Communication for Development Specialist, Mario Mosquera, UNICEF Regional Communication for Development Adviser and Svetlana Stefanet, UNICEF Regional Immunization Specialist, for their significant contributions to its conceptualization and development. We also thank Fatima Cengic, Health and Nutrition Specialist, UNICEF Bosnia and Herzegovina and Jelena Zajeganovic-Jakovljevic, Early Childhood Development Specialist, UNICEF Serbia, as well as Dragoslav Popovic, consultant, the representatives of Institutes of Public Health, academia, health workers, Roma community mediators and civil society organizations from both countries for their support and active engagement in pre-testing and finalizing the package. The materials are based on state-of-the-art resources from UNICEF, the World Health Organization (WHO), European and American Centers for Disease Control, academic journals and the immunization websites of a range of governments and foundations. Authors: Robert Karam, Johns Hopkins Center for Communication Programs Waverly Rennie, Consultant, Johns Hopkins Center for Communication Programs Stephanie Clayton, Johns Hopkins Center for Communication Programs Design: Benussi&theFish Cover Photo: © UNICEF/UN040868/Bicanski © United Nations Children’s Fund (UNICEF), 2019. Some rights reserved. -
Immunization Policies and Procedures Manual
Immunization Policies and Procedures Manual Louisiana Department of Health Office of Public Health Immunization Program Revised September 2017 i Center for Community and Preventive Health Bureau of Infectious Diseases Immunization Program TABLE OF CONTENTS I. POLICY AND GENERAL CLINIC POLICY ............................................................................................................................. 1 PURPOSE ........................................................................................................................................................................................... 1 POLICY ON CLINIC SCHEDULING ............................................................................................................................................ 2 POLICY ON PUBLICITY FOR IMMUNIZATION ACTIVITIES .............................................................................................. 4 POLICY ON EDUCATIONAL ACTIVITIES (HEALTH EDUCATION IN IMMUNIZATION CLINICS) .......................... 5 POLICY ON CHECKING IMMUNIZATION STATUS OF ALL CHILDREN RECEIVING SERVICES THROUGH THE HEALTH DEPARTMENT ...................................................................................................................................................... 6 POLICY ON MAXIMIZING TIME SPENT WITH PARENTS DURING IMMUNIZATION CLINICS ............................... 7 POLICY ON ASSISTANCE TO FOREIGN TRAVELERS .......................................................................................................... 9 II. POLICY -

UNICEF Immunization Roadmap 2018-2030
UNICEF IMMUNIZATION ROADMAP 2018–2030 Cover: ©UNICEF/UN065768/Khouder Al-Issa A health worker vaccinates 3-year-old Rahaf in Tareek Albab neighborhood in the eastern part of Aleppo city. UNICEF IMMUNIZATION ROADMAP 2018–2030 Photograph credits: Pages vi-vii: © Shutterstock/thi Page 5: © UNICEF/UN060913/Al-Issa Page 6: © UNICEF/UNI41364/Estey Page 10: © UNICEF/UN061432/Dejongh Page 14: © UNICEF/UNI76541/Holmes Page 18: © UNICEF/UN0125829/Sharma Page 24: © UNICEF/UN059884/Zar Mon Page 26: © UNICEF/UN065770/Al-Issa Page 33: © UNICEF/UN0143438/Alhariri Page 34: © UNICEF/UNI45693/Estey Page 38: © UNICEF/UNI77040/Holmes Page 40: © UNICEF/UN0125861/Sharma Page 44: © UNICEF/UNI41211/Holmes © United Nations Children’s Fund (UNICEF), September 2018 Permission is required to reproduce any part of this publication. Permission will be freely granted to educational or non-profit organizations. Please contact: Health Section, Immunization Team UNICEF 3 United Nations Plaza New York, NY 100017 Contents Abbreviations viii Executive summary 1 1. Introduction 7 1.1 Background 7 1.2 Developing the Roadmap 9 2. Key considerations informing the UNICEF Immunization Roadmap 11 2.1 Key drivers of immunization through 2030 11 2.2 Evolving immunization partnerships 15 2.3 UNICEF’s comparative advantage in immunization 16 3. What is new in this Roadmap? 19 3.1 Immunization coverage as a tracer indicator of child equity 19 3.2 Key areas of work 21 4. Roadmap programming framework 27 4.1 Vision and impact statements 27 4.2 Programming principles 27 4.3 Context-driven responses 27 4.4 Objectives and priorities 29 4.5 Populations and platforms 32 4.6 Country-level immunization strategies 32 5. -

AAMC Standardized Immunization Form
AAMC Standardized Immunization Form Middle Last Name: First Name: Initial: DOB: Street Address: Medical School: City: Cell Phone: State: Primary Email: ZIP Code: AAMC ID: MMR (Measles, Mumps, Rubella) – 2 doses of MMR vaccine or two (2) doses of Measles, two (2) doses of Mumps and (1) dose of Rubella; or serologic proof of immunity for Measles, Mumps and/or Rubella. Choose only one option. Copy Note: a 3rd dose of MMR vaccine may be advised during regional outbreaks of measles or mumps if original MMR vaccination was received in childhood. Attached Option1 Vaccine Date MMR Dose #1 MMR -2 doses of MMR vaccine MMR Dose #2 Option 2 Vaccine or Test Date Measles Vaccine Dose #1 Serology Results Measles Qualitative -2 doses of vaccine or Measles Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Mumps Vaccine Dose #1 Serology Results Mumps Qualitative -2 doses of vaccine or Mumps Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Serology Results Rubella Qualitative Positive Negative -1 dose of vaccine or Rubella Vaccine Titer Results: positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Tetanus-diphtheria-pertussis – 1 dose of adult Tdap; if last Tdap is more than 10 years old, provide date of last Td or Tdap booster Tdap Vaccine (Adacel, Boostrix, etc) Td Vaccine or Tdap Vaccine booster (if more than 10 years since last Tdap) Varicella (Chicken Pox) - 2 doses of varicella vaccine or positive serology Varicella Vaccine #1 Serology Results Qualitative Varicella Vaccine #2 Titer Results: Positive Negative Serologic Immunity (IgG antibody titer) Quantitative Titer Results: _____ IU/ml Influenza Vaccine --1 dose annually each fall Date Flu Vaccine © 2020 AAMC. -

Hepatitis B Vaccine – Frequently Asked Questions (Information from the CDC)
AAMC Standardized Immunization Form 2020 Hepatitis B Vaccine – Frequently Asked Questions (Information from the CDC) 1. What are the hepatitis B vaccines licensed for use in the United States? Three single-antigen vaccines and two combination vaccines are currently licensed in the United States. Single-antigen hepatitis B vaccines: • ENGERIX-B® • RECOMBIVAX HB® • HEPLISAV-B™ Combination vaccines: • PEDIARIX®: Combined hepatitis B, diphtheria, tetanus, acellular pertussis (DTaP), and inactivated poliovirus (IPV) vaccine. Cannot be administered before age 6 weeks or after age 7 years. • TWINRIX®: Combined Hepatitis A and hepatitis B vaccine. Recommended for people aged ≥18 years who are at increased risk for both HAV and HBV infections. 2. What are the recommended schedules for hepatitis B vaccination? The vaccination schedule most often used for children and adults is three doses given at 0, 1, and 6 months. Alternate schedules have been approved for certain vaccines and/or populations. A new formulation, Heplisav-B (HepB-CpG), is approved to be given as two doses one month apart. 3. If there is an interruption between doses of hepatitis B vaccine, does the vaccine series need to be restarted? No. The series does not need to be restarted but the following should be considered: • If the vaccine series was interrupted after the first dose, the second dose should be administered as soon as possible. • The second and third doses should be separated by an interval of at least 8 weeks. • If only the third dose is delayed, it should be administered as soon as possible. 4. Is it harmful to administer an extra dose of hepatitis B vaccine or to repeat the entire vaccine series if documentation of the vaccination history is unavailable or the serology test is negative? No, administering extra doses of single-antigen hepatitis B vaccine is not harmful.