A Review of Topical and Systemic Vitamin Supplementation in Ocular Surface Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Role of Citicoline in the Management of Traumatic Brain Injury
pharmaceuticals Review Role of Citicoline in the Management of Traumatic Brain Injury Julio J. Secades Medical Department, Ferrer, 08029 Barcelona, Spain; [email protected] Abstract: Head injury is among the most devastating types of injury, specifically called Traumatic Brain Injury (TBI). There is a need to diminish the morbidity related with TBI and to improve the outcome of patients suffering TBI. Among the improvements in the treatment of TBI, neuroprotection is one of the upcoming improvements. Citicoline has been used in the management of brain ischemia related disorders, such as TBI. Citicoline has biochemical, pharmacological, and pharmacokinetic characteristics that make it a potentially useful neuroprotective drug for the management of TBI. A short review of these characteristics is included in this paper. Moreover, a narrative review of almost all the published or communicated studies performed with this drug in the management of patients with head injury is included. Based on the results obtained in these clinical studies, it is possible to conclude that citicoline is able to accelerate the recovery of consciousness and to improve the outcome of this kind of patient, with an excellent safety profile. Thus, citicoline could have a potential role in the management of TBI. Keywords: CDP-choline; citicoline; pharmacological neuroprotection; brain ischemia; traumatic brain injury; head injury Citation: Secades, J.J. Role of 1. Introduction Citicoline in the Management of Traumatic brain injury (TBI) is among the most devastating types of injury and can Traumatic Brain Injury. result in a different profile of neurological and cognitive deficits, and even death in the most Pharmaceuticals 2021, 14, 410. -

Topical Serum for Treatment of Keratomalacia
PROCEDURES PRO > OPHTHALMOLOGY > PEER REVIEWED Topical Serum for Treatment of Keratomalacia Amy Knollinger, DVM, DACVO Eye Care for Animals Salt Lake City, Utah Corneal Anatomy An understanding of corneal anatomy is vital to determine if serum therapy for the treatment of keratomalacia should be initiated. The cornea makes up the anterior por- tion of the globe and provides multiple functions for vision: it is transparent (despite originating from surface ectoderm), thereby allowing for clear vision; it acts as the major refractive (bending of light) surface of the globe; and it provides a protective barrier between the globe and the environment The cornea consists of 4 layers in domestic species, being approximately 0.45–0.55 mm thick in the normal dog. The corneal epithelium is the most external layer overly- What You Will Need ing the stromal layer, which accounts for 90% of the total corneal thickness. The cor- n Sterile gloves neal epithelium in the dog and cat is 5–11 cells thick and has a turnover rate of n approximately 7 days.1 The stroma is made up of collagen fibers, which are precisely Clean #40 clipper blade arranged in parallel sheets running the entire diameter of the cornea, allowing for its n Chlorhexidine scrub and solution transparency. The third layer is an acellular membrane (ie, Descemet’s membrane), n Sterile needle and syringe which forms the basement membrane for the innermost layer, the endothelium. The n corneal endothelium is a single layer of hexagonally shaped cells forming the internal Red top sterile blood collection or barrier between the anterior chamber and the cornea.2 serum separator tube n Centrifuge Corneal Disease n Sterile pipette Corneal ulcers are classified by underlying cause. -

JMSCR Vol||08||Issue||02||Page 208-210||February 2020
JMSCR Vol||08||Issue||02||Page 208-210||February 2020 http://jmscr.igmpublication.org/home/ ISSN (e)-2347-176x ISSN (p) 2455-0450 DOI: https://dx.doi.org/10.18535/jmscr/v8i2.40 Keratomalacia - A Case Report Authors Deepthi Pullepu1*, Deepthi Janga2, V Murali Krishna3 *Corresponding Author Deepthi Pullepu Department of Ophthalmology, Rangaraya Medical College, Kakinada, Andhra Pradesh, India Abstract Xerophthalmia refers to an ocular condition of destructive dryness of conjunctiva and cornea caused due to severe vitamin A deficiency. Usually affects infants, children and women of reproductive age group. It is estimated to affect about one-third of children under the age of five around the world. Keratomalacia means dry and cloudy cornea which melts and perforates, caused due to severe vitamin A deficiency. Here we describe a case of 21 year old female with neurofibromatosis type 1 presenting with keratomalacia. Keywords: Vitamin A deficiency, Xerophthalmia, Keratomalacia. Introduction blindness is a significant contributor Vitamin A is essential for the functioning of the In India, it is estimated that there are immune system, healthy growth and development approximately 6.8 million people who have vision of body and is usually acquired through diet. less than 6/60 in at least one eye due to corneal Globally, 190 million children under five years of diseases; of these, about a million have bilateral age are affected by vitamin A deficiency involvement. They suffer from an increased risk of visual Corneal blindness resulting due to this disease can impairment, illness and death from childhood be completely prevented by institution of effective infections such as measles and those causing preventive or prophylactic measures at the diarrhoea community level. -
Eletriptan Smpc
For the use only of a neurologist/ specialist or a Hospital or a Laboratory Generic Name Citicoline Trade Name Ceham 1. NAME OF THE MEDICINAL PRODUCT: Citicoline 2. QUALITATIVE AND QUANTITATIVE COMPOSITION: Each film coated tablet contains: Citicoline sodium equivalent to Citicoline……………………………500mg 3. PHARMACEUTICAL FORM: Film coated tablet 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications: For the treatment of disturbance of consciousness as resulting from head injuries, brain operation and acute stage of cerebral infarction in adult only. For the treatment of patients with serious cerebral injuries of vascular traumatic nature with or without loss of consciousness & for treatment of degenerative damages & chronic cerebral vascular injuries in senile dementia. 4.2 Posology and Method of Administration The usually recommended dose of Citicoline is 500mg to 1000mg daily and can increase up to 2000mg. Elderly: No dosage adjustment is required in this patient population and the usually recommended adult dose can be administered. 4.3 Contraindications Hypersensitivity to citicoline or any other component of the formulation 4.4 Special Warnings and Special Precautions for Use: Citicoline may cause hypotension and in case necessary the hypotensive effect can be treated with corticosteroids or sympathomimetics. 4.5 Interaction with Other Medicinal Products and Other Forms of Interaction: Citicoline must not be used with medicines containing meclophenoxates (or centrophenoxine). Citicoline increases the effects of L-dopa. 4.6 Fertility, Pregnancy and Lactation There are no adequate and well controlled studies of citicoline during pregnancy and lactation. Citicoline should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. -

More Treatments on Deck for Alcohol Use Disorder
News & Analysis Medical News & Perspectives More Treatments on Deck for Alcohol Use Disorder Jeff Lyon hirteen years have passed since the Raye Z. Litten, PhD, acting director of the ment for AUD were actually prescribed an US Food and Drug Administration NIAAA’s Division of Medications Develop- AUD medication. T (FDA) last approved a new medica- ment and principal investigator of the trial, It is a complicated problem, says John tion to help the nation’s millions of people says the agency is “excited.” Rotrosen, MD, a psychiatrist and addiction withalcoholusedisorder(AUD)stopormod- Nevertheless, the science of alcohol ad- specialist at New York University School of erate their drinking. diction has seen its share of medicines that Medicine. “To a large extent primary care Only 3 such formulations exist, and 1, failed to live up to their early promise dur- physicians don’t screen for alcoholism,” he disulfiram, dates to the Prohibition era. ing full-scale testing. So Litten said the said. “When they do, they may note it, but Known commercially as Antabuse and agency isn’t putting all its eggs in one bas- don’t really do anything about it.” introduced in 1923, it makes people memo- ket. “You need as many weapons as pos- As far as the failure to prescribe exist- rably ill if they ingest alcohol, but it doesn’t sible to treat a complex disease like alcohol ing medications for AUD, Rotrosen blames stop the cravings. The other 2, naltrexone use disorder,” he said. a lack of knowledge. “A lot of doctors in and acamprosate, approved in 1994 and But therein lies a second difficulty. -

Involvement of the Eye in Protein Malnutrition * -303
Bull. Org. mond. Sante 1958, 19, 303-314 Bull. Wld Hith Org. INVOLVEMENT OF THE EYE IN PROTEIN MALNUTRITION * D. S. McLAREN, M.D., Ph.D., D.T.M. & H. Medical Research Officer, East African Institute for Medical Research, Mwanza, Tanganyika Formerly at the MRC Human Nutrition Research Unit, National Institute for Medical Research, London SYNOPSIS An extensive review of the literature on protein malnutrition, with special reference to the frequency of involvement of the eyes, has been made by the author. Consideration of accounts from all parts of the world and in many different languages, including early as well as more recent descriptions of the syndrome, indicates that this important complication has not received sufficient attention hitherto. The evidence available suggests that it is nearly always an accompanying deficiency of vitamin A that is responsible. Less commonly reported-and producing less severe effects-is deficiency of the B-complex vitamins, and there is no clear evidence to date that protein deficiency itself damages the eyes in these cases. The ways in which protein lack might interfere with various aspects of vitamin-A metabolism are discussed, but it is pointed out that their actual significance in human disease is not yet known. A low dietary intake of vitamin A is regarded by the author as being the prime factor in the causation of eye complications, and attention is drawn to the necessity to correct this as part of any prophylactic or therapeutic programme aimed primarily at combat- ing protein malnutrition. The syndrome known by such various names as kwashiorkor, nutritional oedema syndrome, sindrome pluricarencial, and many others (Trowell, Davies & Dean, 1954), and characterized chiefly by a dietary deficiency ofprotein, has been reported as occurring amongst most of the malnourished communities of the world. -

Effect of Combined Therapy with Thrombolysis and Citicoline in a Rat
Journal of the Neurological Sciences 247 (2006) 121–129 www.elsevier.com/locate/jns Effect of combined therapy with thrombolysis and citicoline in a rat model of embolic stroke ⁎ María Alonso de Leciñana a,e, , María Gutiérrez a,d, Jose María Roda a,c, Fernando Carceller a,c, Exuperio Díez-Tejedor a,b a Cerebrovascular Research Unit, La Paz University Hospital, Universidad Autónoma de Madrid, Madrid, Spain b Department of Neurology, La Paz University Hospital, Madrid, Spain c Department of Neurosurgery, La Paz University Hospital, Madrid, Spain d Cerebrovascular Experimental Lab, La Paz University Hospital, Madrid, Spain e Department of Neurology, Ramón y Cajal University Hospital, Madrid, Spain Received 28 April 2005; received in revised form 3 January 2006; accepted 3 March 2006 Available online 22 June 2006 Abstract An approach combining reperfusion mediated by thrombolytics with pharmacological neuroprotection aimed at inhibiting the physiopathological disorders responsible for ischemia-reperfusion damage, could provide an optimal treatment of ischemic stroke. We investigate, in a rat embolic stroke model, the combination of rtPA with citicoline as compared to either alone as monotherapy, and whether the neuroprotector should be provided before or after thrombolysis to achieve a greater reduction of ischemic brain damage. One hundred and nine rats have been studied: four were sham-operated and the rest embolized in the right internal carotid artery with an autologous clot and divided among 5 groups: 1) control; 2) iv rtPA 5 mg/kg 30 min post-embolization 3) citicoline 250 mg/kg ip ×3 doses, 10 min, 24 h and 48 h post-embolization; 4) citicoline combined with rtPA following the same pattern; 5) rtPA combined with citicoline, with a first dose 10 min after thrombolysis. -

Abstract: a 19 Year Old Male Was Diagnosed with Vitamin a Deficiency
Robert Adam Young Abstract: A 19 year old male was diagnosed with vitamin A deficiency (VAD). Clinical examination shows conjunctival changes with central and marginal corneal ulcers. Patient history and lab testing were used to confirm the diagnosis. I. Case History 19 year old Hispanic Male Presents with chief complaint of progressive blur at distance and near in both eyes, foreign body sensation, ocular pain, photophobia, and epiphora; signs/symptoms are worse in the morning upon wakening. Started 6 months to 1 year ago, and has progressively gotten worse. Patient reports that the right eye is worse than the left eye. Ocular history of Ocular Rosacea Medical history of Hypoaldosteronism, Pernicious Anemia, and Type 2 Polyglandular Autoimmune Syndrome Last eye examination was two weeks ago at a medical center Presenting topical/systemic medications - Tobramycin TID OU, Prednisolone Acetate QD OU (has used for two weeks); Fludrocortisone (used long-term per PCP) Other pertinent info includes reports that patient cannot gain weight, although he has a regular appetite. Patient presents looking very slim, malnourished, and undersized for his age. II. Pertinent findings Entering unaided acuities are 20/400 OD with no improvement with pinhole; 20/50 OS that improves to 20/25 with pinhole. Pupil testing shows (-)APD; Pupils are 6mm in dim light, and constrict to 4mm in bright light. Ocular motilities are full and smooth with no reports of diplopia or pain. Tonometry was performed with tonopen and revealed intraocular pressures of 12 mmHg OD and 11 mmHG OS. Slit lamp examination shows 2+ conjunctival injection with trace-mild bitot spots both nasal and temporal, OU. -

Anticraving Therapy for Alcohol Use Disorder: a Clinical Review
Received: 10 April 2018 | Revised: 11 June 2018 | Accepted: 11 June 2018 DOI: 10.1002/npr2.12028 INVITED REVIEW Anticraving therapy for alcohol use disorder: A clinical review Winston W. Shen1,2 1Department of Psychiatry, Wan Fang Medical Center, Taipei Medical University, Abstract Taipei, Taiwan Aim: In this review, the author focused on anticraving therapy for alcohol use disor- 2Department of Psychiatry, College of der (AUD) defined by DMS‐5. A comprehensive review was carried out on the avail- Medicine, Taipei Medical University, Taipei, Taiwan able published papers on anticraving drugs for treating AUD patients. Methods: The author described all drugs with anticraving benefits for treating Correspondence Winston W. Shen, Department of AUD patients approved by the Food and Drug Administration of the United States Psychiatry, Wan Fang Medical Center, No. (US FDA) and European Medicines Agency of the European Union. Then, the com- 111, Section 3, Hsing Long Road, Taipei 116, Taiwan. monly prescribed anticraving drugs and those under development were also Email: [email protected] described. Results: The US FDA‐approved anticraving drugs included acamprosate and naltrex- one, and those approved by European Medicines Agency were gamma‐hydroxybuty- rate and nalmefene. The author also highlighted topiramate, gabapentin, ondansetron, LY196044, ifenprodil, varenicline, ABT‐436, mifepristone, citicoline, and baclofen. The putative mechanisms of action of and the use in clinical practice of those anticraving drugs were also described. Conclusion: Although slowly developing, the field of anticraving drugs is getting into shape as a promising entity of a pharmaceutical class of drugs. Then, the author addressed on the underused issues of those recommended, and suggested anticraving drugs by the practice guideline of the American Psychiatric Association. -

Current Health Issues in the Caribbean BLINDNESS in THE
Current Health Issues in the Caribbean BLINDNESS IN THE CARIBBEAN Alfred L. Anduze, M.D. St. Croix Vision Center St. Croix Hospital St. Croix U.S. Virgin Islands Caribbean Studies Association Merida, Mexico May 26, 1994 Abstract: Blindness in the Caribbean Background: The prevailing of blindness in the Caribbean region are reviewed in the context of world blindness statistics to identify differences and similarities that might exist. Method: A review of the status of blindness in the U.S. Virgin Islands, Barbados, Jamaica, Puerto Rico, Trinidad, and Mexico; individually with regard to causal etiology, epidemiology, treatment and possible future research. Results: Blindness in the Caribbean is the result of genetics, tropical environment and cultural habits of the inhabitants and consist of Age-related macular disease, Infectious diseases, Diabetes mellitus, Glaucoma, Congenital defects, Xerophthalmia, Trachoma, Trauma and Cataracts. Conclusion: There are almost 50 million people who are legally blind worldwide (i.e. with a vision of 20/200 or less) 2-3 million in the Caribbean region. The social and economic consequences are serious additional deterrents in developing countries. Outline: Causes of Blindness in the Caribbean I. Age-related macular disease a. Vascular insufficiency b. Senile macular degeneration II. Cataracts III. Glaucoma IV. Diabetes mellitus V. Infectious diseases a. Trachoma b. Onchocerciasis c. Leprosy d. Toxoplasmosis e. Toxocariasis f. AIDS VI. Trauma a. industrial/work-related b. sports c. home accidents VII. Nutritional a. Xerophthalmia/keratomalacia b. Iron-deficiency anemia c. Tobacco/Alcohol Retinopathy VIII. Congenital defects a. genetic syndromes b. strabismus Legal blindness is acceptably defined as vision 20/200 (6/60) or less. -
2002 Samel 10 Most Common Systemic Health Conditions with A
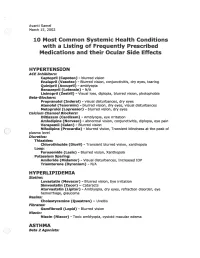
Avanti Samel / March 15, 2002 10 Most Common Systemic Health Conditions with a Listing of Frequently Prescribed Medications and their Ocular Side Effects HYPERTENSION ACE Inhibitors: Captopril (Capoten}- blurred vision Enalapril (Vasotec) - Blurred vision, conjunctivitis, dry eyes, tearing Quinipril (Accupril)- amblyopia Benazepril (Lotensin)- N/A Lisinopril (Zestril) - Visual loss, diplopia, blurred vision, photophobia Beta-Blockers: Propranolol (Inderal)- visual disturbances, dry eyes Atenolol (Tenormin)- blurred vision, dry eyes, visual disturbances Metoprolol (Lopressor) - blurred vision, dry eyes calcium Channel Blockers: Diltiazem (Cardizem)- Amblyopia, eye irritation Amlodipine (Norvasc)- abnormal vision, conjunctivitis, diplopia, eye pain Verapamil (Calan)- Blurred vision Nifedipine (Procardia) - blurred vision, Transient blindness at the peak of plasma level · Diuretics: Thiazides: Chlorothiazide (Diuril) - Transient blurred vision, xanthopsia Loop: Furosemide (Lasix) - Blurred vision, Xanthopsia Potassium Sparing: Amiloride (Midamor) - Visual disturbances, Increased lOP Triamterene (Dyrenium)- N/A HYPERLIPIDEMIA Statins: Lovastatin (Mevacor) - Blurred vision, Eye irritation Simvastatin (Zocor)- Cataracts Atorvastatin (Lipitor)- Amblyopia, dry eyes, refraction disorder, eye hemorrhage, glaucoma Resins: Cholestyramine (Questran)- Uveitis Fibrates: Gemfibrozil (Lopid)- Blurred vision Niacin: Niacin (Niacor) - Toxic amblyopia, cystoid macular edema ASTHMA ( ) Beta 2 Agonists: Albuterol (Proventil) - N/A ( Salmeterol (Serevent)- -

© Alan Macfarlane and Gerry Martin, 2002 1 MYOPIA: ITS
© Alan Macfarlane and Gerry Martin, 2002 MYOPIA: ITS COMPARATIVE INCIDENCE AND PROBABLE CAUSES What Rasmussen encountered in his many years of working with Chinese eye problem astonished him. He summarized his impressions thus. 'Three facts stand out clearly in both ancient and modern records of Chinese eyesight: one that they are a highly myopic nation; two that keratomalacia is the major cause of ocular disease; and three that presbyopia is earlier than in the West by about five years. They stand out against an historical background of neglect and abuse, malnutrition, and centuries of State indifference.' (p.48) Moving on to the statistics of myopia, he summarized the research of a quarter of a century by saying that 'only 20 per cent. of all lenses supplied by the ancients, and similar amount by the moderns (excluding high astigmatic) were for old-sight lenses. It is the other 80 per cent. that matters; the 65 per cent. for myopia and the 15 per cent. for glare and therapeutics.' (p.20) Elsewhere he gives slightly different statistics, which applied to those aged under forty years, showed that approximately 75 per cent. of the lenses were supplied for myopia. In a detailed table he presents the figures; in the 'Ancient Chinese Sight Records', 65% were for myopia; in the 'Modern Chinese Sight Records' myopia (simple) or with astigmatism combined accounted for 70% of the lenses.(p.48) The second figure of 70% was based on 120,000 case histories collected by Rasmussen and his colleagues over a period of 25 years. (p.49) The significance of the degree of myopia only comes out if we compare the Chinese figures with those for other nationalities.