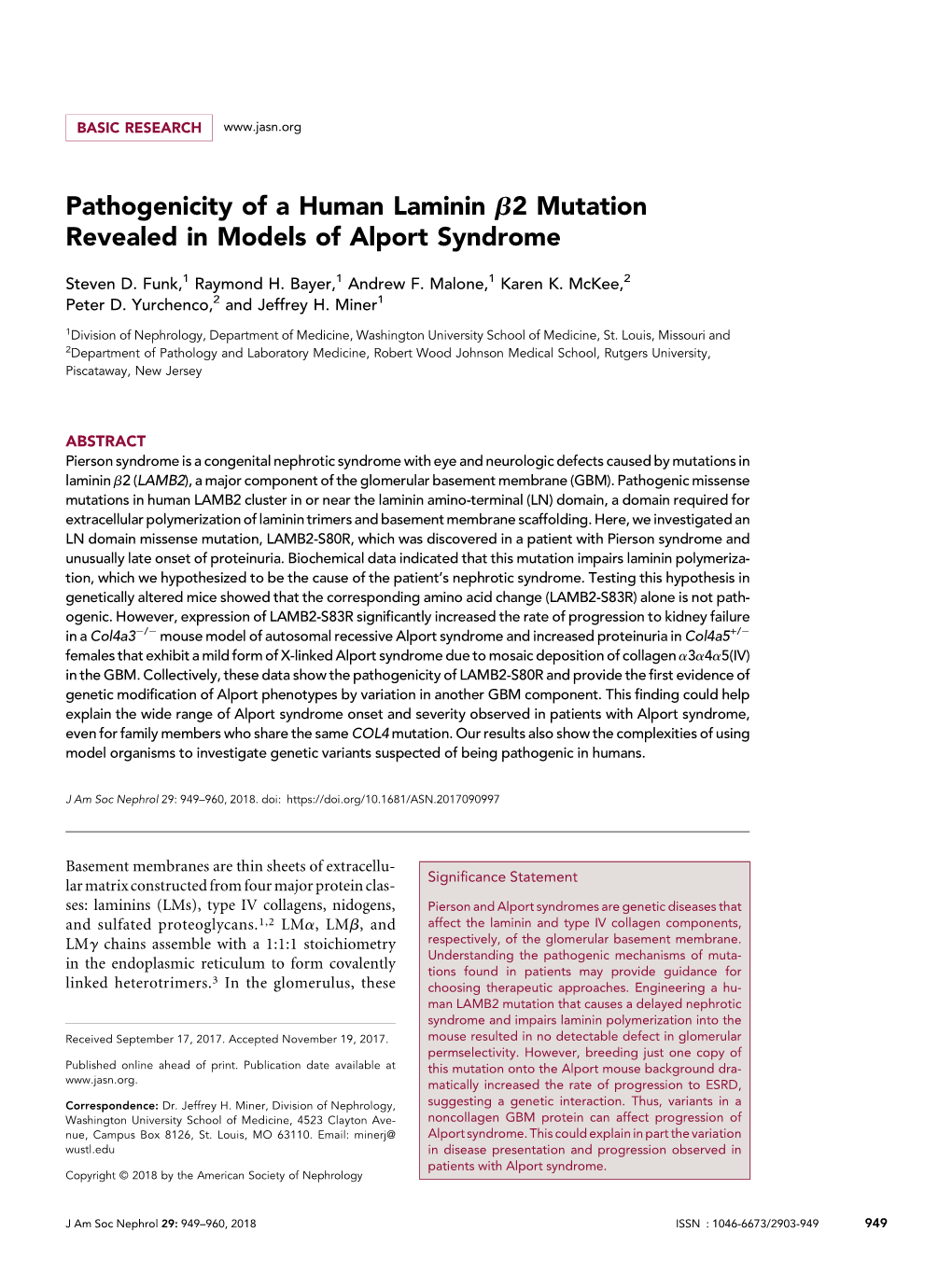
Pathogenicity of a Human Laminin Β2 Mutation Revealed in Models Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![Alport Syndrome of the European Dialysis Population Suffers from AS [26], and Simi- Lar Figures Have Been Found in Other Series](https://docslib.b-cdn.net/cover/5855/alport-syndrome-of-the-european-dialysis-population-suffers-from-as-26-and-simi-lar-figures-have-been-found-in-other-series-435855.webp)
Alport Syndrome of the European Dialysis Population Suffers from AS [26], and Simi- Lar Figures Have Been Found in Other Series
DOCTOR OF MEDICAL SCIENCE Patients with AS constitute 2.3% (11/476) of the renal transplant population at the Mayo Clinic [24], and 1.3% of 1,000 consecutive kidney transplant patients from Sweden [25]. Approximately 0.56% Alport syndrome of the European dialysis population suffers from AS [26], and simi- lar figures have been found in other series. AS accounts for 18% of Molecular genetic aspects the patients undergoing dialysis or having received a kidney graft in 2003 in French Polynesia [27]. A common founder mutation was in Jens Michael Hertz this area. In Denmark, the percentage of patients with AS among all patients starting treatment for ESRD ranges from 0 to 1.21% (mean: 0.42%) in a twelve year period from 1990 to 2001 (Danish National This review has been accepted as a thesis together with nine previously pub- Registry. Report on Dialysis and Transplantation in Denmark 2001). lished papers by the University of Aarhus, February 5, 2009, and defended on This is probably an underestimate due to the difficulties of establish- May 15, 2009. ing the diagnosis. Department of Clinical Genetics, Aarhus University Hospital, and Faculty of Health Sciences, Aarhus University, Denmark. 1.3 CLINICAL FEATURES OF X-LINKED AS Correspondence: Klinisk Genetisk Afdeling, Århus Sygehus, Århus Univer- 1.3.1 Renal features sitetshospital, Nørrebrogade 44, 8000 Århus C, Denmark. AS in its classic form is a hereditary nephropathy associated with E-mail: [email protected] sensorineural hearing loss and ocular manifestations. The charac- Official opponents: Lisbeth Tranebjærg, Allan Meldgaard Lund, and Torben teristic renal features in AS are persistent microscopic hematuria ap- F. -

The Ehlers–Danlos Syndromes
PRIMER The Ehlers–Danlos syndromes Fransiska Malfait1 ✉ , Marco Castori2, Clair A. Francomano3, Cecilia Giunta4, Tomoki Kosho5 and Peter H. Byers6 Abstract | The Ehlers–Danlos syndromes (EDS) are a heterogeneous group of hereditary disorders of connective tissue, with common features including joint hypermobility, soft and hyperextensible skin, abnormal wound healing and easy bruising. Fourteen different types of EDS are recognized, of which the molecular cause is known for 13 types. These types are caused by variants in 20 different genes, the majority of which encode the fibrillar collagen types I, III and V, modifying or processing enzymes for those proteins, and enzymes that can modify glycosaminoglycan chains of proteoglycans. For the hypermobile type of EDS, the molecular underpinnings remain unknown. As connective tissue is ubiquitously distributed throughout the body, manifestations of the different types of EDS are present, to varying degrees, in virtually every organ system. This can make these disorders particularly challenging to diagnose and manage. Management consists of a care team responsible for surveillance of major and organ-specific complications (for example, arterial aneurysm and dissection), integrated physical medicine and rehabilitation. No specific medical or genetic therapies are available for any type of EDS. The Ehlers–Danlos syndromes (EDS) comprise a genet six EDS types, denominated by a descriptive name6. The ically heterogeneous group of heritable conditions that most recent classification, the revised EDS classification in share several clinical features, such as soft and hyper 2017 (Table 1) identified 13 distinct clinical EDS types that extensible skin, abnormal wound healing, easy bruising are caused by alterations in 19 genes7. -

Genetic Disorder
Genetic disorder Single gene disorder Prevalence of some single gene disorders[citation needed] A single gene disorder is the result of a single mutated gene. Disorder Prevalence (approximate) There are estimated to be over 4000 human diseases caused Autosomal dominant by single gene defects. Single gene disorders can be passed Familial hypercholesterolemia 1 in 500 on to subsequent generations in several ways. Genomic Polycystic kidney disease 1 in 1250 imprinting and uniparental disomy, however, may affect Hereditary spherocytosis 1 in 5,000 inheritance patterns. The divisions between recessive [2] Marfan syndrome 1 in 4,000 and dominant types are not "hard and fast" although the [3] Huntington disease 1 in 15,000 divisions between autosomal and X-linked types are (since Autosomal recessive the latter types are distinguished purely based on 1 in 625 the chromosomal location of Sickle cell anemia the gene). For example, (African Americans) achondroplasia is typically 1 in 2,000 considered a dominant Cystic fibrosis disorder, but children with two (Caucasians) genes for achondroplasia have a severe skeletal disorder that 1 in 3,000 Tay-Sachs disease achondroplasics could be (American Jews) viewed as carriers of. Sickle- cell anemia is also considered a Phenylketonuria 1 in 12,000 recessive condition, but heterozygous carriers have Mucopolysaccharidoses 1 in 25,000 increased immunity to malaria in early childhood, which could Glycogen storage diseases 1 in 50,000 be described as a related [citation needed] dominant condition. Galactosemia -

Ehlers-Danlos Syndrome Type VI in a 17-Year-Old Iranian Boy with Severe Muscular Weakness – a Diagnostic Challenge?
Iran J Pediatr Case Report Sep 2010; Vol 20 (No 3), Pp: 358-362 Ehlers-Danlos Syndrome Type VI in a 17-Year-Old Iranian Boy with Severe Muscular Weakness – A Diagnostic Challenge? Ariana Kariminejad*1, MD; Bita Bozorgmehr1, MD; Alireza Khatami2; MD; Mohamad-Hasan Kariminejad1, MD; Cecilia Giunta3, MD, and Beat Steinmann3, MD 1. Kariminejad Najmabadi Pathology and Genetics Center, Tehran, IR Iran 2. Mofid Children's Hospital, Shahid Beheshti University of Medical Sciences, Tehran, IR Iran 3. Division of Metabolism and Molecular Pediatrics, University Children's Hospital Zurich, Switzerland Received: May 20, 2009; Final Revision: Nov 14, 2009; Accepted: Jan 18, 2010 Abstract Background: The Ehlers-Danlos syndrome type VI (EDSVI) is an autosomal recessive connective tissue disease which is characterized by severe hypotonia at birth, progressive kyphoscoliosis, skin hyperelasticity and fragility, joint hypermobility and (sub-)luxations, microcornea, rupture of arteries and the eye globe, and osteopenia. The enzyme collagen lysyl hydroxylase (LH1) is deficient in these patients due to mutations in the PLOD1 gene. Case Presentation: We report a 17-year-old boy, born to related parents, with severe kyphoscoliosis, scar formation, joint hypermobility and multiple dislocations, muscular weakness, rupture of an ocular globe, and a history of severe infantile hypotonia. EDS VI was suspected clinically and confirmed by an elevated ratio of urinary total lysyl pyridinoline to hydroxylysyl pyridinoline, abnormal electrophoretic mobility of the α-collagen chains, and mutation analysis. Conclusion: Because of the high rate of consanguineous marriages in Iran and, as a consequence thereof, an increased rate of autosomal recessive disorders, we urge physicians to consider EDS VI in the differential diagnosis of severe infantile hypotonia and muscular weakness, a disorder which can easily be confirmed by the analysis of urinary pyridinolines that is highly specific, sensitive, robust, fast, non-invasive, and inexpensive. -

Type IV Collagens and Basement Membrane Diseases: Cell Biology and Pathogenic Mechanisms
CHAPTER THREE Type IV Collagens and Basement Membrane Diseases: Cell Biology and Pathogenic Mechanisms Mao Mao, Marcel V. Alavi, Cassandre Labelle-Dumais and Douglas B. Gould* Departments of Ophthalmology and Anatomy, Institute for Human Genetics, UCSF School of Medicine, San Francisco, CA, USA *Corresponding author: E-mail: [email protected] Contents 1. Genomic Organization and Protein Structure of Type IV Collagens 62 1.1 Introduction and history 62 1.2 Genomic structure 64 1.3 Protein domain structure 66 1.3.1 7S domain 68 1.3.2 Triple helical domain 69 1.3.3 NC1 domain 70 2. Type IV Collagen Biosynthesis 72 2.1 Heat shock protein 47 72 2.2 Protein disulfide isomerase 73 2.3 Peptidylprolyl isomerases 74 2.4 Prolyl 4-hydroxylases 74 2.5 Prolyl 3-hydroxylases 75 2.6 Lysyl hydroxylases 76 2.7 Transport and Golgi organization 1 78 3. Type IV Collagen-Related Pathology 78 3.1 COL4A3eA6-associated pathology 78 3.1.1 Goodpasture disease 78 3.1.2 Alport syndrome 79 3.2 COL4A1/COL4A2-associated pathology 81 3.2.1 Ocular dysgenesis 81 3.2.2 Porencephaly 82 3.2.3 Small vessel disease 83 3.2.4 Cerebral cortical lamination defects 84 3.2.5 Myopathy 85 3.2.6 HANAC syndrome and nephropathy 85 4. Mechanisms for Type IV Collagen-Related Pathology 86 4.1 Overview 86 Current Topics in Membranes, Volume 76 ISSN 1063-5823 © 2015 Elsevier Inc. http://dx.doi.org/10.1016/bs.ctm.2015.09.002 All rights reserved. 61 j 62 Mao Mao et al. -
An Access-Dictionary of Internationalist High Tech Latinate English
An Access-Dictionary of Internationalist High Tech Latinate English Excerpted from Word Power, Public Speaking Confidence, and Dictionary-Based Learning, Copyright © 2007 by Robert Oliphant, columnist, Education News Author of The Latin-Old English Glossary in British Museum MS 3376 (Mouton, 1966) and A Piano for Mrs. Cimino (Prentice Hall, 1980) INTRODUCTION Strictly speaking, this is simply a list of technical terms: 30,680 of them presented in an alphabetical sequence of 52 professional subject fields ranging from Aeronautics to Zoology. Practically considered, though, every item on the list can be quickly accessed in the Random House Webster’s Unabridged Dictionary (RHU), updated second edition of 2007, or in its CD – ROM WordGenius® version. So what’s here is actually an in-depth learning tool for mastering the basic vocabularies of what today can fairly be called American-Pronunciation Internationalist High Tech Latinate English. Dictionary authority. This list, by virtue of its dictionary link, has far more authority than a conventional professional-subject glossary, even the one offered online by the University of Maryland Medical Center. American dictionaries, after all, have always assigned their technical terms to professional experts in specific fields, identified those experts in print, and in effect held them responsible for the accuracy and comprehensiveness of each entry. Even more important, the entries themselves offer learners a complete sketch of each target word (headword). Memorization. For professionals, memorization is a basic career requirement. Any physician will tell you how much of it is called for in medical school and how hard it is, thanks to thousands of strange, exotic shapes like <myocardium> that have to be taken apart in the mind and reassembled like pieces of an unpronounceable jigsaw puzzle. -

Engineering Biointerfaces to Reveal Collagen IV Disease Mechanisms
Ngandu Mpoyi, Elie (2017) Engineering biointerfaces to reveal collagen IV disease mechanisms. PhD thesis. https://theses.gla.ac.uk/9032/ Copyright and moral rights for this work are retained by the author A copy can be downloaded for personal non-commercial research or study, without prior permission or charge This work cannot be reproduced or quoted extensively from without first obtaining permission in writing from the author The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the author When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given Enlighten: Theses https://theses.gla.ac.uk/ [email protected] Engineering biointerfaces to reveal collagen IV disease mechanisms Elie Ngandu Mpoyi (BSc (Hons), MRes2) Submitted in fulfilment of the requirements for the Degree of Doctor of Philosophy Biomedical Engineering School of Engineering University of Glasgow August 2017 Abstract Basement Membranes (BMs) are specialised extracellular matrix (ECM) structures that underlie all endothelial and epithelial cells, and provide structural support to tissues as well as influence cell behaviour and signalling. Mutations in the BMs major component collagen IV cause eye, kidney and cerebrovascular disease including intracerebral haemorrhaging (ICH). Haemorrhagic stroke accounts for 15% adult stroke and 50% paediatric stroke, and carries the worst prognosis and there are no therapeutic strategies. Mutations in the genes COL4A1/COL4A2 (collagen IV alpha chain 1 and 2) cause BM defects due to mutant protein incorporation in the BM or its absence by ER retention, and ER-stress due to intracellular accumulation of collagen IV. -

Desordens Genéticas Nome Modelo Idade 40 Sexo F Data De Emissão 10-04-2020
Desordens Genéticas Nome Modelo Idade 40 Sexo F Data de Emissão 10-04-2020 Prescritor Modelo Convenio Modelo Nossa metodologia: Sequenciamento do Genoma Inteiro Humano - WGS O WGS está inaugurando uma nova era, a da verdadeira Medicina Personalizada, Preditiva e Preventiva, ao realizar o sequenciamento do genoma total. A tecnologia WGS, utilizada pela FULLDNA, permite, a partir de resultados indiscutíveis, detalhados e específicos de variantes genéticas, a criação de uma Identidade Genética Personalizada de cada pessoa, composta de suas Características, Necessidades e Suscetibilidades genéticas, além de se poder gerar, a partir das análises, Tratamentos Geneticamente Personalizados, pois os avanços com a tecnologia WGS já estão permitindo a orientação de tratamentos para cânceres comuns (como câncer colorretal e melanoma) e determinação de quais medicamentos são seguros (e quais não são) para cada pessoa. A WGS é uma excepcional inovação tecnológica por executar o sequenciamento do genoma inteiro com expressiva eficiência. Quando comparado com tecnologias parciais de DNA autossômico, como o teste de DNA autossômico com microarrays ou sequenciamento de exoma (1% do genoma), a tecnologia WGS da FULLDNA fornece 3.000 vezes mais informações por fornecer dados sobre todos os seis bilhões de pares de bases do genoma humano. Ela fornece cobertura completa das regiões codificadoras e não codificadoras do genoma e variantes de um único nucleotídeo, inserções/deleções, alterações no número de cópias e grandes variantes estruturais, além da determinação das variações no número de cópias, rearranjos e outras variações estruturais. Com a utilização da tecnologia WGS, a FULLDNA realiza hoje a análise mais completa e única no mundo, o que oferece ao profissional de saúde e a cada pessoa um potencial preditivo e preventivo também único. -

Geographical Differences in Osteoporosis, Obesity, And
www.nature.com/scientificreports OPEN Geographical diferences in osteoporosis, obesity, and sarcopenia related traits in white Received: 6 November 2017 Accepted: 29 July 2019 American cohorts Published: xx xx xxxx Yu Zhou1,2, Kehao Wu1, Hui Shen1, Jigang Zhang1, Hong-Wen Deng1 & Lan-Juan Zhao 1 It has been reported that geographical variation infuences bone mineral density (BMD), obesity, and sarcopenia related traits in other countries. However, there is lack of similar studies in the US population. In this study, we compared data from three US study cohorts to evaluate geographical variations of BMD and body composition. BMD, fat mass and lean mass were collected from Dual- energy X-ray absorptiometry machine. ANCOVA and Chi-square tests were used to compare the diferences between BMDs, obesity and sarcopenia related traits from diferent regional sites (Omaha, Kansas City and Baton Rouge/New Orleans). Eta-squared was used to measure the efect sizes of these diferences. A total of 11,315 Caucasians from our previous three study cohorts were compared. There was no signifcant geographical diference in BMD for males or females under the criteria of p-values < 0.05 and efect size η2 > 0.01. There were signifcant geographical diferences with medium efect size (p-value < 0.001, 0.01 < η2 < 0.14) for whole body fat mass percentage and index of low muscle mass. For Caucasians in the United States, there is no signifcant geographical efect found on BMD. The obesity and sarcopenia related traits are signifcantly diferent between the three study cohorts. Osteoporosis, obesity, and sarcopenia (age-related decrease in skeletal muscle mass) are three of the most com- mon health issues in the world. -

Abt—Letterer—Siwe Disease 400 Accessory Bones 4 Acetabular
1105 Index A osteophytes 950 cervical spinous processes 631 atelosteogenesis 6 productive bone changes 69 cervical vertebrae 599, 626, 629, atheroma, calcified of calvarium 405 Abt—Letterer—Siwe disease 400 sesamoid bones 1091 631, 632 athyrosis, sella turcica 453 accessory bones 4 acromioclavicular joint 287–91 double trolley back 704 atlanto-occipital joint 572 acetabular index 816 anomalies 287–8 lumbar vertebrae 702–6 arthritis 599 depth-to-width 817, 818 calcification 287, 290 occipitoatlantoaxial joints 600 dislocation 596, 597 acetabulum degenerative change 290 sacroiliitis 755–6 dysplasia 622 accessory bones 821–2, 823 dislocation 280, 288, 289 thoracic vertebrae 662, 663 motion 573 accessory fossa 824 fractures 288, 289 triple trolley back 704 osteoarthritis 601 anatomy 811, 813, 814 inflammation 290 ankylosis synostosis 435, 588–9 apophyses joint space widening 290, 302 acquired bony 27–8 atlanto-occipital membrane, anterior marginal 804, 806–7 necrosis 289–90 apophyseal joint spaces 612, 613 603 persistence 821–2 normal variants 287–8 carpal inflammatory 131 atlantoaxial joint persistent accessory 807 osteoarthritis 290, 291 cervical spine 629, 630 fusions 589 bony defect 824 posttraumatic ossification 289 sacroiliac joint 758 osteoarthritis 601, 602 center—edge angle of Wiberg 817, pseudodislocation 288, 289 thoracic vertebrae 662–3 rotational analysis 574 818 rheumatic disorders 290 annulus fibrosus 558 atlantoaxial segmentation, irregular components 804 subluxation 288, 289 calcification 721, 722, 723 590 congenital dislocation -

Case Report Bullous Systemic Lupus Erythematosus Associated with Esophagitis Dissecans Superficialis
Hindawi Publishing Corporation Case Reports in Rheumatology Volume 2015, Article ID 930683, 4 pages http://dx.doi.org/10.1155/2015/930683 Case Report Bullous Systemic Lupus Erythematosus Associated with Esophagitis Dissecans Superficialis Meera Yogarajah, Bhradeev Sivasambu, and Eric A. Jaffe Department of Medicine, Interfaith Medical Center, Brooklyn, NY 11213, USA Correspondence should be addressed to Meera Yogarajah; [email protected] Received 10 October 2014; Accepted 23 February 2015 Academic Editor: Tsai-Ching Hsu Copyright © 2015 Meera Yogarajah et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Bullous systemic lupus erythematosus is one of the rare autoantibody mediated skin manifestation of systemic lupus erythematosus (SLE) demonstrating subepidermal blistering with neutrophilic infiltrate histologically. We present a case of a 40-year-old Hispanic female who presented with a several months’ history of multiple blistering pruritic skin lesions involving the face and trunk, a photosensitive rash over the face and neck, swelling of the right neck lymph node, and joint pain involving her elbows and wrist. Her malady was diagnosed as bullous systemic lupus erythematosus based on the immunological workup and biopsy of her skin lesions. The patient also complained of odynophagia and endoscopy revealed esophagitis dissecans superficialis which is arare endoscopic finding characterized by sloughing of the esophageal mucosa. The bullous disorders typically associated with esophagitis dissecans superficialis are pemphigus and rarely bullous pemphigoid. However, this is the first reported case of bullous systemic lupus erythematosus associated with esophagitis dissecans superficialis. -

Autoimmune Diseases of the Skin.Pdf
Michael Hertl (ed.) Autoimmune Diseases of the Skin Pathogenesis, Diagnosis, Management Second, revised and enlarged edition SpringerWienNewYork Prof. Michael Hertl, MD Department of Dermatology and Allergology, Philipps University, Marburg, Germany This book was supported by Gesellschaft für Autoimmun-Krankheiten e.V., Schönkirchen bei Kiel This work is subject to copyright. All rights are reserved, whether the whole or part of the material is concerned, specifically those of translation, reprinting, re-use of illustrations, broadcasting, reproduction by photo- copying machines or similar means, and storage in data banks. © 2001 and 2005 Springer-Verlag Wien · Printed in Austria SpringerWienNewYork is a part of Springer Science + Business Media springeronline.com Product Liability: The publisher can give no guarantee for all the information contained in this book. This also refers to that on drug dosage and application thereof. In each indi- vidual case the respective user must check the accuracy of the information given by con- sulting other pharmaceutical literature.The use of registered names, trademarks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. Cover illustration: M. Hertl Typesetting: Composition & Design Services, Minsk 220027, Belarus Printing: Druckerei Theiss GmbH, A-9431 St. Stefan im Lavanttal Printed on acid-free and chlorine-free bleached paper SPIN: 10975923 With 77 partly coloured Figures Library of Congress Control Number: 2005920465 ISBN 3-211-20686-8 SpringerWienNewYork ISBN 3-211-83598-9 1st edition SpringerWienNewYork Foreword Based on recent advances in the understanding of the immunological patho- genesis of many chronic inflammatory disorders there is increasing evidence that several of them are characterized and potentially mediated by autoimmune phenomena.