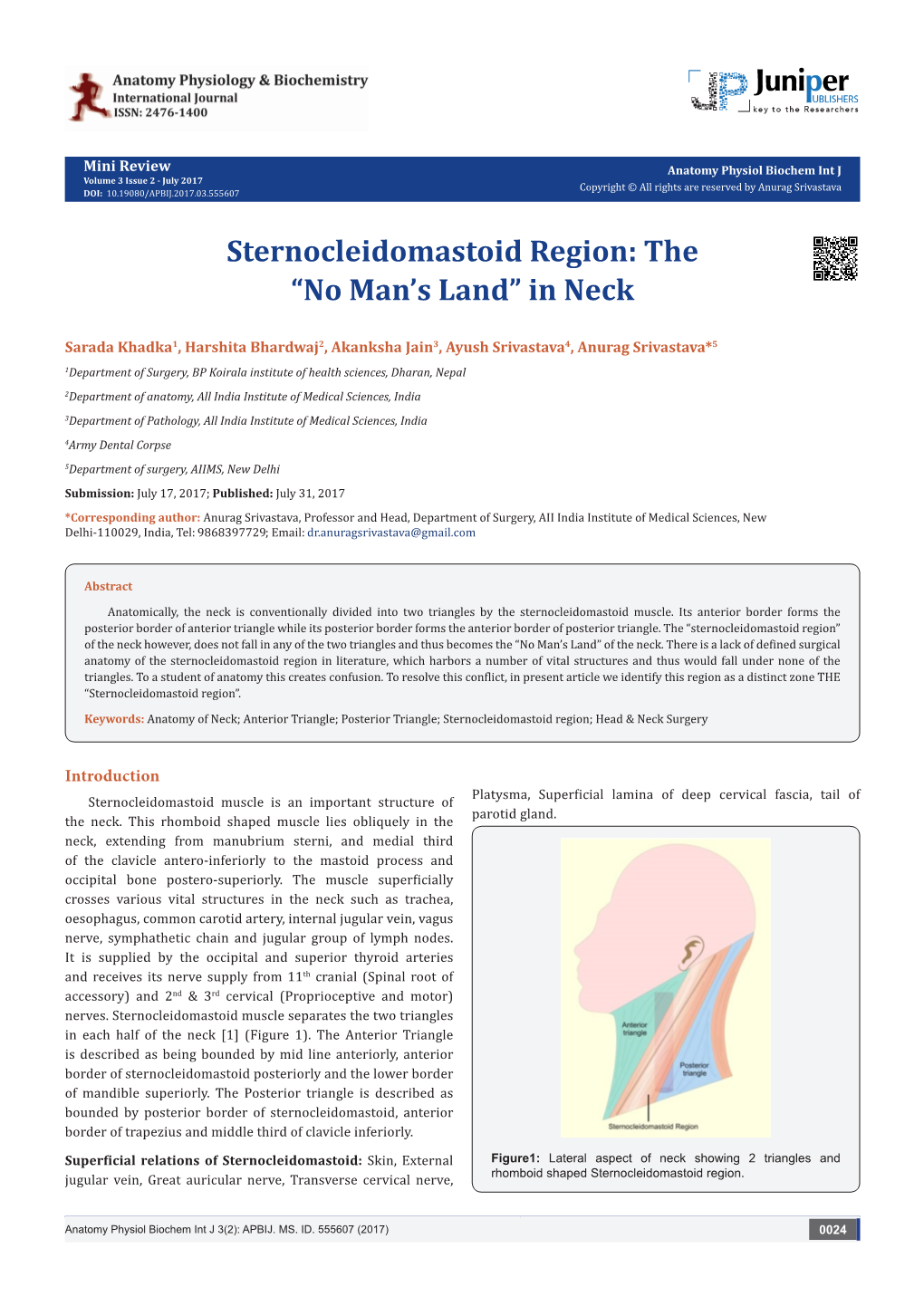
Sternocleidomastoid Region: the “No Man’S Land” in Neck
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

7-Khyati Santram
J. Anat. Sciences, 24(2): Dec. 2016, 33-35 Case Report ANATOMICAL VARIATION OF THE TRAPEZIUS MUSCLE- A CASE REPORT Khayati Sant Ram*, Anjali Aggarwal*,Tulika Gupta *,Amandeep kaur*,Jyoti Rajput*, Daisy Sahni* *Department of Anatomy, Post Graduate Institute of Medical Education and Research, Chandigarh, ABSTRACT During routine cadaveric dissection for undergraduate teaching variation in the course and insertion of fibers left trapezius muscle was noticed in two embalmed male cadavers. Some of the occipital fibers while descending towards clavicle got separated from rest of the muscle, inclined medially and inserted on the 1cm area of middle third of superior surface of clavicle. The remaining occipital fibers got inserted after a gap of on 1.5cm on the superior surface of lateral part of clavicle. Detached portion of trapezius muscles was tendinous in insertion. Two structures namely external jugular vein and supraclavicular nerves were seen passing through the gap in one cadaver (Case 1) whereas in other cadaver (Case 2) only external jugular vein was passing through the gap. Knowledge of this variation is clinically important in surgical exploration of posterior triangle.supraclavicular nerve entrapment syndrome and in various approaches involving external jugular vein. Key words: - trapezius muscle, cleidoccipital, supraclavicular nerves INTRODUCTION insertion of clavicular fibers left trapezius muscle of Trapezius muscle(TM) is a flat triangular muscle left side was noticed in two adult male cadavers. which extends over back of the neck and upper Case 1- In 78- years-old male cadaver trapezius thorax. On either side the muscle is attached to muscle of left side took usual origin from the medial medial third of superior nuchal line, external occipital portion of superior nuchal line, external occipital protuberance, ligamentum nuchae and apices of the protuberance, ligamentum nuchae and apices of the spinous processes and their supraspinous ligament spinous processes of thoracic vertebrae. -

Neck Dissection Using the Fascial Planes Technique
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY NECK DISSECTION USING THE FASCIAL PLANE TECHNIQUE Patrick J Bradley & Javier Gavilán The importance of identifying the presence larised in the English world in the mid-20th of metastatic neck disease with head and century by Etore Bocca, an Italian otola- neck cancer is recognised as a prominent ryngologist, and his colleagues 5. factor determining patients’ prognosis. The current available techniques to identify Fascial compartments allow the removal disease in the neck all have limitations in of cervical lymphatic tissue by separating terms of accuracy; thus, elective neck dis- and removing the fascial walls of these section is the usual choice for management “containers” along with their contents of the clinically N0 neck (cN0) when the from the underlying vascular, glandular, risk of harbouring occult regional metasta- neural, and muscular structures. sis is significant (≥20%) 1. Methods availa- ble to identify the N+ (cN+) neck include Anatomical basis imaging (CT, MRI, PET), ultrasound- guided fine needle aspiration cytology The basic understanding of fascial planes (USGFNAC), and sentinel node biopsy, in the neck is that there are two distinct and are used depending on resource fascial layers, the superficial cervical fas- availability, for the patient as well as the cia, and the deep cervical fascia (Figures local health service. In many countries, 1A-C). certainly in Africa and Asia, these facilities are not available or affordable. In such Superficial cervical fascia circumstances patients with head and neck cancer whose primary disease is being The superficial cervical fascia is a connec- treated surgically should also have the tive tissue layer lying just below the der- neck treated surgically. -

Unusual Organization of the Ansa Cervicalis: a Case Report
CASE REPORT ISSN- 0102-9010 UNUSUAL ORGANIZATION OF THE ANSA CERVICALIS: A CASE REPORT Ranjana Verma1, Srijit Das2 and Rajesh Suri3 Department of Anatomy, Maulana Azad Medical College, New Delhi-110002, India. ABSTRACT The superior root of the ansa cervicalis is formed by C1 fibers carried by the hypoglossal nerve, whereas the inferior root is contributed by C2 and C3 nerves. We report a rare finding in a 40-year-old male cadaver in which the vagus nerve fused with the hypoglossal nerve immediately after its exit from the skull on the left side. The vagus nerve supplied branches to the sternohyoid, sternothyroid and superior belly of the omohyoid muscles and also contributed to the formation of the superior root of the ansa cervicalis. In this arrangement, paralysis of the infrahyoid muscles may result following lesion of the vagus nerve anywhere in the neck. The cervical location of the vagus nerve was anterior to the common carotid artery within the carotid sheath. This case report may be of clinical interest to surgeons who perform laryngeal reinnervation and neurologists who diagnose nerve disorders. Key words: Ansa cervicalis, hypoglossal nerve, vagus nerve, variations INTRODUCTION cadaver. The right side was normal. The neck region The ansa cervicalis is a nerve loop formed was dissected and the neural structures in the carotid by the union of superior and inferior roots. The and muscular triangle regions were exposed, with superior root is a branch of the hypoglossal nerve particular attention given to the organization of the containing C1 fibers, whereas the inferior root is ansa cervicalis. -

Deep Neck Infections 55
Deep Neck Infections 55 Behrad B. Aynehchi Gady Har-El Deep neck space infections (DNSIs) are a relatively penetrating trauma, surgical instrument trauma, spread infrequent entity in the postpenicillin era. Their occur- from superfi cial infections, necrotic malignant nodes, rence, however, poses considerable challenges in diagnosis mastoiditis with resultant Bezold abscess, and unknown and treatment and they may result in potentially serious causes (3–5). In inner cities, where intravenous drug or even fatal complications in the absence of timely rec- abuse (IVDA) is more common, there is a higher preva- ognition. The advent of antibiotics has led to a continu- lence of infections of the jugular vein and carotid sheath ing evolution in etiology, presentation, clinical course, and from contaminated needles (6–8). The emerging practice antimicrobial resistance patterns. These trends combined of “shotgunning” crack cocaine has been associated with with the complex anatomy of the head and neck under- retropharyngeal abscesses as well (9). These purulent col- score the importance of clinical suspicion and thorough lections from direct inoculation, however, seem to have a diagnostic evaluation. Proper management of a recog- more benign clinical course compared to those spreading nized DNSI begins with securing the airway. Despite recent from infl amed tissue (10). Congenital anomalies includ- advances in imaging and conservative medical manage- ing thyroglossal duct cysts and branchial cleft anomalies ment, surgical drainage remains a mainstay in the treat- must also be considered, particularly in cases where no ment in many cases. apparent source can be readily identifi ed. Regardless of the etiology, infection and infl ammation can spread through- Q1 ETIOLOGY out the various regions via arteries, veins, lymphatics, or direct extension along fascial planes. -

Tentorium Cerebelli: the Bridge Between the Central and Peripheral Nervous System, Part 2
Open Access Review Article DOI: 10.7759/cureus.5679 Tentorium Cerebelli: the Bridge Between the Central and Peripheral Nervous System, Part 2 Bruno Bordoni 1 , Marta Simonelli 2 , Maria Marcella Lagana 3 1. Cardiology, Foundation Don Carlo Gnocchi, Milan, ITA 2. Osteopathy, French-Italian School of Osteopathy, Pisa, ITA 3. Radiology, IRCCS Fondazione Don Carlo Gnocchi Onlus, Milan, ITA Corresponding author: Bruno Bordoni, [email protected] Abstract The tentorium cerebelli is a meningeal portion in relation to the skull, the nervous system, and the cervical tract. In this second part, the article discusses the systematic tentorial relationships, such as the central and cervical neurological connections, the venous circulation and highlights possible clinical alterations that could cause pain. To understand the function of anatomy, we should always remember that every area of the human body is never a segment, but a functional continuum. Categories: Physical Medicine & Rehabilitation, Anatomy, Osteopathic Medicine Keywords: tentorium cerebelli, fascia, pain, venous circulation, neurological connections, cranio Introduction And Background Cervical neurological connections The ansa cervicalis characterizes the first cervical roots and connects all anterior cervical nerve exits with the inferior floor of the oral cavity, the trigeminal system, the respiratory control system, and the sympathetic system. The descending branch of the hypoglossal nerve anastomoses with C1, forming the ansa hypoglossi or ansa cervicalis superior [1]. The inferior root of the ansa cervicalis, also known as descendens cervicalis, is formed by ascendant fibers from spinal nerves C2-C3 and occasionally fibers C4, lying anteriorly to the common carotid artery (it passes laterally or medially to the internal jugular vein upon anatomical variations) [1]. -

Vascular Supply to the Head and Neck
Vascular supply to the head and neck Sumamry This lesson covers the head and neck vascular supply. ReviseDental would like to thank @KIKISDENTALSERVICE for the wonderful drawings in this lesson. Arterial supply to the head Facial artery: Origin: External carotid Branches: submental a. superior and inferior labial a. lateral nasal a. angular a. Note: passes superiorly over the body of there mandible at the masseter Superficial temporal artery: Origin: External carotid Branches: It is a continuation of the ex carotid a. Note: terminal branch of the ex carotid a. and is in close relation to the auricular temporal nerve Transverse facial artery: Origin: Superficial temporal a. Note: exits the parotid gland Maxillary branch: supplies the areas missed from the above vasculature Origin: External carotid a. Branches: (to the face) infraorbital, buccal and inferior alveolar a.- mental a. Note: Terminal branch of the ex carotid a. The ophthalmic branches Origin: Internal carotid a. Branches: Supratrochlear, supraorbital, lacrimal, anterior ethmoid, dorsal nasal Note:ReviseDental.com enters orbit via the optic foramen Note: The face arterial supply anastomose freely. ReviseDental.com ReviseDental.com Venous drainage of the head Note: follow a similar pathway to the arteries Superficial vessels can communicate with deep structures e.g. cavernous sinus and the pterygoid plexus. (note: relevant for spread of infection) Head venous vessels don't have valves Supratrochlear vein Origin: forehead and communicates with the superficial temporal v. Connects: joins with supra-orbital v. Note: from the angular vein Supra-orbital vein Origin: forehead and communicates with the superficial temporal v. Connects: joins with supratrochlear v. -

The Levator Scapulae Muscle – Morphological Variations K
International Journal of Anatomy and Research, Int J Anat Res 2019, Vol 7(4.3):7169-75. ISSN 2321-4287 Original Research Article DOI: https://dx.doi.org/10.16965/ijar.2019.335 THE LEVATOR SCAPULAE MUSCLE – MORPHOLOGICAL VARIATIONS K. Satheesh Naik 1, Sadhu Lokanadham 2. *1 Assistant Professor, Department of Anatomy, Viswabharathi Medical College & General Hospital, Penchikalapadu, Kurnool, Andhrapradesh, India. 2 Associate Professor, Department of Anatomy, Santhiram Medical College and General Hospital, Nandyal, Andhrapradesh, India. ABSTRACT Introduction: Anatomical variations of the levator scapulae are important and therefore clinically relevant. The levator scapulae are now believed to be the leading cause of discomfort in patients with chronic tension-type neck and shoulder pain and a link between anatomical variants of the muscle and increased risk of developing pain has been speculated. The results obtained were compared with previous studies. Materials and methods: The study was conducted on 32 levator scapulae muscle of 16 cadavers over a period of 3 years. The dissection of head and neck was done carefully to preserve all minute details, observing the morphological variations of the muscle in the department of Anatomy, Viswabharathi Medical College, Penchikalapadu, and Kurnool. Results: Total 32 levator scapulae muscles were used. All the sample values were measured to 2 decimal places. The average age of the cadavers in the sample was 82.87 years. The oldest cadaver in the sample was 100 years old and the youngest 61 years. Measurements of the proximal and distal attachments and the total length of the muscles were taken. Between 3 and 6 muscle slips were reported at the proximal attachment. -

A Comprehensive Review of Anatomy and Regional Anesthesia Techniques of Clavicle Surgeries
vv ISSN: 2641-3116 DOI: https://dx.doi.org/10.17352/ojor CLINICAL GROUP Received: 31 March, 2021 Research Article Accepted: 07 April, 2021 Published: 10 April, 2021 *Corresponding author: Dr. Kartik Sonawane, Uncovering secrets of the Junior Consultant, Department of Anesthesiol- ogy, Ganga Medical Centre & Hospitals, Pvt. Ltd. Coimbatore, Tamil Nadu, India, E-mail: beauty bone: A comprehensive Keywords: Clavicle fractures; Floating shoulder sur- gery; Clavicle surgery; Clavicle anesthesia; Procedure review of anatomy and specific anesthesia; Clavicular block regional anesthesia techniques https://www.peertechzpublications.com of clavicle surgeries Kartik Sonawane1*, Hrudini Dixit2, J.Balavenkatasubramanian3 and Palanichamy Gurumoorthi4 1Junior Consultant, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India 2Fellow in Regional Anesthesia, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India 3Senior Consultant, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India 4Consultant, Department of Anesthesiology, Ganga Medical Centre & Hospitals, Pvt. Ltd., Coimbatore, Tamil Nadu, India Abstract The clavicle is the most frequently fractured bone in humans. General anesthesia with or without Regional Anesthesia (RA) is most frequently used for clavicle surgeries due to its complex innervation. Many RA techniques, alone or in combination, have been used for clavicle surgeries. These include interscalene block, cervical plexus (superficial and deep) blocks, SCUT (supraclavicular nerve + selective upper trunk) block, and pectoral nerve blocks (PEC I and PEC II). The clavipectoral fascial plane block is also a safe and simple option and replaces most other RA techniques due to its lack of side effects like phrenic nerve palsy or motor block of the upper limb. -

Comparing the Organs and Vasculature of the Head and Neck
in vivo 31 : 861-871 (2017) doi:10.21873/invivo.11140 Comparing the Organs and Vasculature of the Head and Neck in Five Murine Species MIN JAE KIM 1* , YOO YEON KIM 2* , JANET REN CHAO 3, HAE SANG PARK 1,4 , JIWON CHANG 1,4 , DAWOON OH 5, JAE JUN LEE 4,6 , TAE CHUN KANG 7, JUN-GYO SUH 2 and JUN HO LEE 1,4 1Department of Otorhinolaryngology-Head and Neck Surgery, College of Medicine, Hallym University, Chuncheon, Republic of Korea; 2Department of Medical Genetics, College of Medicine, Hallym University, Chuncheon, Republic of Korea; 3School of Medicine, George Washington University, Washington, DC, U.S.A.; 4Institute of New Frontier Research, Hallym University College of Medicine, Chuncheon, Republic of Korea; 5Department of Anesthesiology and Pain Medicine, Dongtan Sacred Heart Hospital, Hallym University, Dongtan, Republic of Korea; 6Department of Anesthesiology and Pain Medicine, College of Medicine, Hallym University, Chuncheon, Republic of Korea; 7Department of Anatomy and Neurobiology, College of Medicine, Hallym University, Chuncheon, Republic of Korea Abstract. Background/Aim: The purpose of the present Unique morphological characteristics were demonstrated by study was to delineate the cervical and facial vascular and comparing the five species, including symmetry of the associated anatomy in five murine species, and compare common carotid origin bilaterally in the Mongolian Gerbil, them for optimal use in research studies focused on a large submandibular gland in the hamster and an enlarged understanding the pathology and treatment of diseases in buccal branch in the Guinea Pig. In reviewing the humans. Materials and Methods: The specific adult male anatomical details, this staining technique proves superior animals examined were mice (C57BL/6J), rats (F344), for direct surgical visualization and identification. -

A Source of Complication in Vagus Nerve Stimulation
PEDIATRICS CASE REPORT J Neurosurg Pediatr 15:535–538, 2015 The “vagal ansa”: a source of complication in vagus nerve stimulation Chittur Viswanathan Gopalakrishnan, MS, MCh,1 John R. W. Kestle, MD,1 and Mary B. Connolly, MB, FRCP(C)2 1Division of Neurosurgery, Department of Surgery, University of British Columbia and BC Children’s Hospital; and 2Division of Neurology, Department of Paediatrics, University of British Columbia and BC Children’s Hospital, Vancouver, British Columbia, Canada A 16-year-old boy underwent vagus nerve stimulation for treatment-resistant multifocal epilepsy. During intraoperative system diagnostics, vigorous contraction of the ipsilateral sternomastoid muscle was observed. On re-exploration, a thin nerve fiber passing from the vagus to the sternomastoid was found hooked up in the upper electrode. Detailed inspec- tion revealed an abnormal course of the superior root of the ansa cervicalis, which descended down as a single nerve trunk with the vagus and separated to join the inferior root. The authors discuss the variation in the course of the ansa cervicalis and how this could be a reason for postoperative neck muscle contractions. http://thejns.org/doi/abs/10.3171/2014.10.PEDS14259 KEY WORDS ansa cervicalis; variation; vagus nerve stimulation; epilepsy; complication; peripheral nerve HE ansa cervicalis, located in the anterior triangle of We describe an intraoperative complication noticed the neck, is formed by the anterior rami of the first during testing of the VNS system after placement of the 3 or 4 cervical spinal nerves. This nerve loop in- electrodes and the pulse generator. To the best of our Tnervates the infrahyoid muscles.5 It is frequently encoun- knowledge, it has not been previously reported. -

DENT-1431: Head and Neck Anatomy 1
DENT-1431: Head and Neck Anatomy 1 DENT-1431: HEAD AND NECK ANATOMY Cuyahoga Community College Viewing: DENT-1431 : Head and Neck Anatomy Board of Trustees: 2018-01-25 Academic Term: 2018-01-16 Subject Code DENT - Dental Hygiene Course Number: 1431 Title: Head and Neck Anatomy Catalog Description: Study of structure and function of head and neck. General anatomy of the skull, related muscles, vascular and nerve supply and lymphatics of the region considered. Focus on muscles of mastication and their relationship to the temporomandibular joint; facial and trigeminal nerves and their relationship with dental injections. Discussion on spread of infection and its clinical manifestations. Credit Hour(s): 2 Lecture Hour(s): 2 Lab Hour(s): 0 Other Hour(s): 0 Requisites Prerequisite and Corequisite DENT-1300 Preventive Oral Health Services I Outcomes Course Outcome(s): Apply the foundational knowledge of anatomical landmarks and nerve innervation toward successful mastery of local anesthesia and pain management concepts and skills. Objective(s): 1. Identify on a skull, diagram, and by narrative description the bones, sutures, foramina, soft tissue and muscles of the head that are associated with dental injections. 2. Name the divisions of the Trigeminal Nerve, its exit from the cranium, branches and areas of supply. 3. Indicate the tissues anesthetized by each type of dental injection and indicate the target area and possible complications of those injections. 4. List the armamentarium necessary for dental injections and assemble/disassemble a syringe. Course Outcome(s): Utilize knowledge of head and neck examination techniques in clinical practice to differentiate between healthy conditions and possible pathologies. -

Eponyms in Head and Neck Anatomy and Radiology
Pictorial Essay Eponyms in Head and Neck Anatomy and Radiology Fernando Martín Ferraro1*, Hernán Chaves2*, Federico Martín Olivera Plata3,4*, Luis Ariel Miquelini1,3*, Suresh K. Mukherji5 1 Imaging Service, Hospital Británico, Ciudad Autónoma de Buenos Aires, Argentina 2 Imaging Department, Dr. Raúl Carrea Institute for Neurological Research (FLENI), Ciudad Autónoma de Buenos Aires, Argentina 3Imaging Service, Hospital Italiano de Buenos Aires, Ciudad Autónoma de Buenos Aires, Argentina 4 Magnetic Resonance and Computed Tomography Service, Centro Médico Deragopyan, Ciudad Autónoma de Buenos Aires, Argentina 5 Radiology Department, Michigan State University, East Lansing, USA Abstract The use of eponyms in medical language is frequent. While it is commonly thought that eponyms are on their way to extinction, this is not entirely true. There is dissent between those who believe that their use should be abandoned and those who advocate that eponyms make unmemorable terms memorable, convey complex concepts and promote an interest in the history of medicine. We feel part of this second group, and our intention is to make a review of eight eponyms linked to head and neck anatomy and radiology. We believe that this approach can be useful for the education of medical students, residents and diagnostic imaging specialists. Keywords Radiology; Eponyms; Anatomy; Head and neck; History of medicine Introduction for which they are known. Eponyms are illustrated by figures of dissections, radiological images and pictures. We believe When we look up the word eponym in Spanish (epónimo) that this approach can be useful for the education of medical in the dictionary of the Spanish Royal Academy, we find the students, residents and diagnostic imaging specialists.