REQUIREMENTS for MEDICAL IMAGING MONITORS (Part I)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Adaptive Quantization Matrices for High Definition Resolutions in Scalable HEVC
Original citation: Prangnell, Lee and Sanchez Silva, Victor (2016) Adaptive quantization matrices for HD and UHD display resolutions in scalable HEVC. In: IEEE Data Compression Conference, Utah, United States, 31 Mar - 01 Apr 2016 Permanent WRAP URL: http://wrap.warwick.ac.uk/73957 Copyright and reuse: The Warwick Research Archive Portal (WRAP) makes this work by researchers of the University of Warwick available open access under the following conditions. Copyright © and all moral rights to the version of the paper presented here belong to the individual author(s) and/or other copyright owners. To the extent reasonable and practicable the material made available in WRAP has been checked for eligibility before being made available. Copies of full items can be used for personal research or study, educational, or not-for profit purposes without prior permission or charge. Provided that the authors, title and full bibliographic details are credited, a hyperlink and/or URL is given for the original metadata page and the content is not changed in any way. Publisher’s statement: © 2016 IEEE. Personal use of this material is permitted. Permission from IEEE must be obtained for all other uses, in any current or future media, including reprinting /republishing this material for advertising or promotional purposes, creating new collective works, for resale or redistribution to servers or lists, or reuse of any copyrighted component of this work in other works. A note on versions: The version presented here may differ from the published version or, version of record, if you wish to cite this item you are advised to consult the publisher’s version. -

Dell 24 USB-C Monitor - P2421DC User’S Guide
Dell 24 USB-C Monitor - P2421DC User’s Guide Monitor Model: P2421DC Regulatory Model: P2421DCc NOTE: A NOTE indicates important information that helps you make better use of your computer. CAUTION: A CAUTION indicates potential damage to hardware or loss of data if instructions are not followed. WARNING: A WARNING indicates a potential for property damage, personal injury, or death. Copyright © 2020 Dell Inc. or its subsidiaries. All rights reserved. Dell, EMC, and other trademarks are trademarks of Dell Inc. or its subsidiaries. Other trademarks may be trademarks of their respective owners. 2020 – 03 Rev. A01 Contents About your monitor ......................... 6 Package contents . 6 Product features . .8 Identifying parts and controls . .9 Front view . .9 Back view . 10 Side view. 11 Bottom view . .12 Monitor specifications . 13 Resolution specifications . 14 Supported video modes . 15 Preset display modes . 15 MST Multi-Stream Transport (MST) Modes . 16 Electrical specifications. 16 Physical characteristics. 17 Environmental characteristics . 18 Power management modes . 19 Plug and play capability . 25 LCD monitor quality and pixel policy . 25 Maintenance guidelines . 25 Cleaning your monitor. .25 Setting up the monitor...................... 26 Attaching the stand . 26 │ 3 Connecting your monitor . 28 Connecting the DP cable . 28 Connecting the monitor for DP Multi-Stream Transport (MST) function . 28 Connecting the USB Type-C cable . 29 Connecting the monitor for USB-C Multi-Stream Transport (MST) function. 30 Organizing cables . 31 Removing the stand . 32 Wall mounting (optional) . 33 Operating your monitor ..................... 34 Power on the monitor . 34 USB-C charging options . 35 Using the control buttons . 35 OSD controls . 36 Using the On-Screen Display (OSD) menu . -
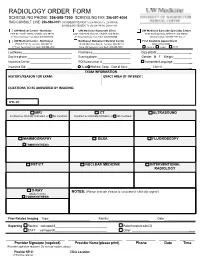
Radiology Order Form
RADIOLOGY ORDER FORM SCHEDULING PHONE: 206-598-7200 SCHEDULING FAX: 206-597-4004 RAD CONSULT LINE: 206-598-0101 UW RADIOLOGY RECORDS: Tel: 206-598-6206 Fax: 206-598-7690 NW RADIOLOGY RECORDS: Tel: 206-668-1748 Fax: 206-688-1398 UW Medical Center - Montlake UW Medicine Roosevelt Clinic UW Medicine Eastside Specialty Center 1959 NE Pacific Street, Seattle, WA 98195 4245 Roosevelt Way NE, Seattle, WA 98105 3100 Northup Way, Bellevue, WA 98004 2nd Floor Radiology Front Desk: 206-598-6200 2nd Floor Radiology Front Desk: 206-598-6868 ESC Front Desk: 425-646-7777 Opt. 2 UW Medical Center - Northwest Northwest Outpatient Medical Center First Available Appointment 1550 N 115th St, Seattle, WA 98133 10330 Meridian Ave N, Seattle, WA 98133 (ANY LOCATION) 2nd Floor Radiology Front Desk: 206-668-1302 Suite 130 Radiology Front Desk: 206-668-6050 Routine Urgent STAT Last Name: First Name: Date of Birth: _ Daytime phone: Evening phone: Gender: M F Weight:___________ Insurance Carrier: RQI/Authorization #: Interpreter/Language: __ Insurance ID#: Auto Workers’ Comp Date of Injury: ______ Claim # __ EXAM INFORMATION HISTORY/REASON FOR EXAM: EXACT AREA OF INTEREST: EXAM INFORMATION QUESTIONS TO BE ANSWERED BY IMAGING: ICD-10: MRI CT ULTRASOUND Contrast as clinically indicated, or No Contrast Contrast as clinically indicated, or No Contrast MAMMOGRAPHY DEXA FLUOROSCOPY TOMOSYNTHESIS PET/CT NUCLEAR MEDICINE INTERVENTIONAL RADIOLOGY X-RAY NOTES: (Please indicate if exam is considered “clinically urgent”) (Walk-In Only) TOMOSYNTHESIS Prior Related Imaging Type:_________________________ Facility:_________________________ Date:___________________ Reporting Routine call report # Patient to return with CD STAT call report # Other: __________ ________________________ ______________________ ____________ _______ ______ Provider Signature (required) Provider Name (please print) Phone Date Time (Provider signature required. -

RADIOGRAPHY to Prepare Individuals to Become Registered Radiologic Technologists
RADIOGRAPHY To prepare individuals to become Registered Radiologic Technologists. THE WORKFORCE CAPITAL This two-year, advanced medical program trains students in radiography. Radiography uses radiation to produce images of tissues, organs, bones and vessels of the body. The radiographer is an essential member of the health care team who works in a variety of settings. Responsibili- ties include accurately positioning the patient, producing quality diagnostic images, maintaining equipment and keeping computerized records. This certificate program of specialized training focuses on each of these responsibilities. Graduates are eligible to apply for the national credential examination to become a registered technologist in radiography, RT(R). Contact Student Services for current tuition rates and enrollment information. 580.242.2750 Mission, Goals, and Student Learning Outcomes Program Effectiveness Data Radiography Program Guidelines (Policies and Procedures) “The programs at Autry prepare you for the workforce with no extra training needed after graduation.” – Kenedy S. autrytech.edu ENDLESS POSSIBILITIES 1201 West Willow | Enid, Oklahoma, 73703 | 580.242.2750 | autrytech.edu COURSE LENGTH Twenty-four-month daytime program î August-July î Monday-Friday Academic hours: 8:15am-3:45pm Clinical hours: Eight-hour shifts between 7am-5pm with some ADMISSION PROCEDURES evening assignments required Applicants should contact Student Services at Autry Technology Center to request an information/application packet. Applicants who have a completed application on file and who have met entrance requirements will be considered for the program. Meeting ADULT IN-DISTRICT COSTS the requirements does not guarantee admission to the program. Qualified applicants will be contacted for an interview, and class Year One: $2732 (Additional cost of books and supplies approx: $1820) selection will be determined by the admissions committee. -

Acr–Nasci–Sir–Spr Practice Parameter for the Performance and Interpretation of Body Computed Tomography Angiography (Cta)
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2021 (Resolution 47)* ACR–NASCI–SIR–SPR PRACTICE PARAMETER FOR THE PERFORMANCE AND INTERPRETATION OF BODY COMPUTED TOMOGRAPHY ANGIOGRAPHY (CTA) PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -

MRC Review of Positron Emission Tomography (PET) Within the Medical Imaging Research Landscape
MRC Review of Positron Emission Tomography (PET) within The Medical Imaging Research Landscape August 2017 Content 1 Introduction 3 2 The medical imaging research landscape in the UK 4 2.1 Magnetic resonance imaging (MRI) 4 2.2 PET, including PET-MRI 6 2.3 Magnetoencephalography 7 3 Scientific uses and demand for PET imaging 8 3.1 Clinical practice 8 3.2 Research use of PET 8 3.3 Demand for PET 10 4 Bottlenecks 11 4.1 Cost 11 4.2 Radiochemistry requirements 12 4.3 Capacity 13 4.4 Analysis and modelling 13 5 Future Opportunities 14 5.1 Mitigating the high costs 14 5.2 Capacity building 14 5.3 Better Networking 15 6 Discussion and conclusions 16 Appendix 1 Experts consulted in the review 17 Appendix 2 Interests of other funders 18 Appendix 3 Usage and cost of PET in research 21 Appendix 4 Summary of facilities and capabilities across UK PET centres of excellence 23 2 1. Introduction This report aims to provide a review of Positron Emission Tomography (PET) within the medical imaging research landscape and a high level strategic review of the UK’s capabilities and needs in this area. The review was conducted by face-to-face and telephone interviews with 35 stakeholders from UK centres of excellence, international experts, industry and other funders (list at appendix 1). Data were also collected on facilities, resources and numbers of scans conducted across the centres of excellence using a questionnaire. The review has focused predominantly on PET imaging, but given MRC’s significant recent investment in other imaging modalities (7T Magnetic Resonance Imaging (MRI), hyperpolarised MRI) through the Clinical Research Infrastructure (CRI) Initiative, these are also considered more briefly. -

Detectability Model for the Evaluation of Lossy Compression Methods on Radiographic Images Vivek Ramaswami Iowa State University
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 1996 Detectability model for the evaluation of lossy compression methods on radiographic images Vivek Ramaswami Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Electrical and Electronics Commons Recommended Citation Ramaswami, Vivek, "Detectability model for the evaluation of lossy compression methods on radiographic images" (1996). Retrospective Theses and Dissertations. 250. https://lib.dr.iastate.edu/rtd/250 This Thesis is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Detectability model for the evaluation of lossy compression methods on radiographic images by Vivek Ramaswami A thesis submitted to the graduate faculty in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Major: Electrical Engineering Major Professors: Satish S. Udpa and Joseph N. Gray Iowa State University Ames, Iowa 1996 Copyright © Vivek Ramaswami, 1996. All rights reserved. 11 Graduate College Iowa State University This is to certify that the Master's thesis of Vivek Ramaswami has met the t hesis requirements of Iowa State University Signature redacted for privacy 111 TABLE OF CONTENTS ACKNOWLEDGEMENTS IX 1 INTRODUCTION . 1 2 IMAGE COMPRESSION METHODS 5 201 Introduction o 0 0 0 0 0 5 2o2 Vector quantization 0 0 ..... 5 20201 Classified vector quantizer 6 20202 Coding of shade blocks o ..... -

EN User Manual 1 Customer Care and Warranty 28 Troubleshooting & Faqs 32 Table of Contents
499P9 www.philips.com/welcome EN User manual 1 Customer care and warranty 28 Troubleshooting & FAQs 32 Table of Contents 1. Important ...................................... 1 1.1 Safety precautions and maintenance ................................. 1 1.2 Notational Descriptions ............ 3 1.3 Disposal of product and packing material .......................................... 4 2. Setting up the monitor .............. 5 2.1 Installation .................................... 5 2.2 Operating the monitor .............. 9 2.3 Built-in Windows Hello™ pop- up webcam .................................14 2.4 MultiClient Integrated KVM .....16 2.5 MultiView ..................................... 17 2.6 Remove the Base Assembly for VESA Mounting ..........................18 3. Image Optimization ..................19 3.1 SmartImage .................................19 3.2 SmartContrast ............................20 3.3 Adaptive Sync .............................21 4. HDR ............................................. 22 5. Technical Specifications ......... 23 5.1 Resolution & Preset Modes ...26 6. Power Management ................ 27 7. Customer care and warranty . 28 7.1 Philips’ Flat Panel Displays Pixel Defect Policy ..............................28 7.2 Customer Care & Warranty ...... 31 8. Troubleshooting & FAQs ......... 32 8.1 Troubleshooting ........................ 32 8.2 General FAQs ............................. 33 8.3 Multiview FAQs .........................36 1. Important discoloration and damage to the 1. Important monitor. This electronic -

2019 Radiology Cpt Codes
2019 RADIOLOGY CPT CODES BONE DENSITOMETRY 1 Bone Density/DEXA 77080 CT 1 CT Abd & Pelvis W/ Contrast 74177 1 CT Enterography W/ Contrast 74177 1 CT Max/Facial W/O Contrast 70486 # CT Sinus Complete W/O Contrast 70486 1 CT Abd & Pelvis W W/O Contrast 74178 1 CT Extremity Lower W/ Contrast 73701 1 CT Neck W/ Contrast 70491 # CT Sinus Limited W/O Contrast 76380 1 CT Abd & Pelvis W/O Contrast 74176 1 CT Extremity Lower W/O Contrast 73700 1 CT Neck W/O Contrast 70490 # CT Spine Cervical W/ Contrast 72126 1 CT Abd W/ Contrast 74160 1 CT Extremity Upper W/ Contrast 73201 1 CT Orbit/ IAC W/ Contrast 70481 # CT Spine Cervical W/O Contrast 72125 1 CT Abd W/O Contrast 74150 1 CT Extremity Upper W/O Contrast 73200 1 CT Orbit/ IAC W/O Contrast 70480 # CT Spine Lumbar W/ Contrast 72132 1 CT Abd W W/O Contrast 74170 1 CT Head W/ Contrast 70460 1 CT Orbit/ IAC W W/O Contrast 70482 # CT Spine Lumbar W/O Contrast 72131 1 CT Chest W/ Contrast 71260 1 CT Head W/O Contrast 70450 1 CT Pelvis W/ Contrast 72193 # CT Spine Thoracic W/ Contrast 72129 1 CT Chest W/O Contrast 71250 1 CT Head W W/O Contrast 70470 1 CT Pelvis W/O Contrast 72192 # CT Spine Thoracic W/O Contrast 72128 1 CT Chest W W/O Contrast 71270 1 CT Max/Facial W/ Contrast 70487 1 CT Pelvis W W/O Contrast 72194 # CT Stone Protocol W/O Contrast 74176 CTA 1 Cardiac Calcium Score only 75571 1 CT Angiogram Abd & Pelvis W W/O Contrast 74174 1 CT Angiogram Head W W/O Contrast 70496 # CT / CTA Heart W Contrast 75574 1 CT Angiogram Abdomen W W/O Contrast 74175 1 CT Angiogram Chest W W/O Contrast 71275 -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Impact of Adaptation Dimensions on Video Quality
Impact of Adaptation Dimensions on Video Quality Jens Brandt and Lars Wolf Institute of Operating Systems and Computer Networks (IBR), Technische Universitat¨ Braunschweig, Germany [email protected] Abstract—The number and types of mobile devices which well as the network conditions, may vary more often over time are capable of presenting digital video streams is increasing compared to static devices. Thus, the experience of watching constantly. In most cases the devices are trade-offs between video streams on mobile devices differs to a great extent from powerful all-purpose computers and small mobile devices which are ubiquitously available and range from cellular phones to those scenarios related to static displays usually found in the notebooks. This great heterogeneity of mobile devices makes area of home entertainment. For sequences from soccer games video streaming to such devices a challenging task for content McCarthy et al. observed that potential users preferred lower providers. Each single device has its own capabilities and indi- frame rates but higher detail resolution on mobile devices [2]. vidual requirements, which need to be considered when sending For other genres similar findings were presented for scalable a video stream to it. Thus, to support a great range of different devices, the video streams need to be adapted to the requirements video coding by Eichhorn and Ni in [3]. Besides concentration of each device. To get an idea of how different adaptation methods solely on the temporal resolution of a video stream, in our may affect the experience of users watching a streamed video on a work we additionally investigated the effect of adapting the mobile device, we inspect the influence of three major adaptation spatial and the detail resolution as well. -

Diagnostic Radiography Is the Production of High Quality Images for the Purpose of Diagnosis of Injury Or Disease
A Career in Medical Imaging What is Diagnostic Radiography / Medical Imaging? Diagnostic Radiography is the production of high quality images for the purpose of diagnosis of injury or disease. It is a pivotal aspect of medicine and a patient's diagnosis and ultimate treatment is often dependent on the images produced. Diagnostic Radiography uses both ionising and non-ionising radiation in the imaging process. The equipment used is at the high end of technology and computerisation within medicine. What does a Diagnostic Radiographer / Medical Imaging Technologist do? A Diagnostic Radiographer/Medical Imaging Technologist is a key member of the health care team. They are responsible for producing high quality medical images that assist medical specialists and practitioners to describe, diagnose, monitor and treat a patient’s injury or illness. Much of the medical equipment used to gain the images is highly technical and involves state of the art computerisation. A Diagnostic Radiographer/Medical Imaging Technologist needs to have the scientific and technological background to understand and use the equipment within a modern Radiology department as well as compassion and strong interpersonal skills. They need to be able to demonstrate care and understanding and have a genuine interest in a patient's welfare. The Diagnostic Radiographer/Medical Imaging Technologist will also need to be able to explain to the patient the need for the preparation and post examination care as well as the procedure to be undertaken. The Diagnostic Radiographer/Medical Imaging Technologist is able to work in a highly advanced technical profession that requires excellent people skills. It is an exciting and rewarding profession to embark on and great opportunities await the graduate.