5Th COMMON REVIEW MISSION REPORT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Answered On:02.12.2002 Discovery of Ancient Site by Asi Chandra Vijay Singh
GOVERNMENT OF INDIA TOURISM AND CULTURE LOK SABHA UNSTARRED QUESTION NO:2136 ANSWERED ON:02.12.2002 DISCOVERY OF ANCIENT SITE BY ASI CHANDRA VIJAY SINGH Will the Minister of TOURISM AND CULTURE be pleased to state: (a) names of the monuments in the Moradabad and Bareilly division under ASI; (b) whether Excavations conducted at Madarpur in Moradabad District of Uttar Pradesh have unearthed an archaeological site dating to 2nd century B.C.; (c) steps taken for preservation of the site and the amount allocated for the purpose; and (d) steps proposed to be taken to further explore to excavate the area? Answer MINISTER FOR TOURISM AND CULTURE (SHRI JAGMOHAN ) (a) A list of Centrally protected monuments in Moradabad and Bareilly division is annexed. (b) The excavation conducted in January, 2000 revealed findings datable to 2nd millennium B.C. (c) & (d) Steps have been taken to conserve the site. An amount of Rs.1,84,093/- has been incurred so far. Further steps have been initiated to explore adjacent areas to assess its archaeological potentiality. ANNEXURE ANNEXURE REFFERED TO IN REPLY OF LOK SABHA UNSTARRED QUESTION NO.2136 TO BE ANSWERED ON 2.12.2002 REGARDING DISCOVERY OF ANCIENT SITE BY ASI (a) Moradabad Division (i) Moradabad District: S.No. Locality Name of the Centrally Protected Monument/Site 1. Alipur, Tehsil :Chandausi Amarpati Khera 2. Alipur, Tehsil:Chandausi Chandesvara Khera 3. Berni, Tehsil;Chandausi Khera or Mound reputed to be the ruin or palace or Raja Vena 4. Bherabharatpur, Tehsil Amorha Large mound, the site of an ancient temple 5. -

Proposed UGC- Minor Research Project
Introduction Regional disparity is a ubiquitous phenomenon in both developed and developing economies. But in the latter it is more acute and glaring. When economic development occurs unequally across a country, regional differences in the levels of living become an important political issue. State economies are often composed of sets of smaller and localized economies. If the national economy is to prosper then its constituent regional economies must be brought into some sort of harmony. Any attempt to implement regional balanced -growth strategy, it is necessary to identify nature and pattern of regional development, the availability of basic amenities and the quality of infrastructure available. In Uttar Pradesh too, area disparities in the level of poverty, unemployment, income, infrastructure, agriculture, industry and above all the level of living of people exist substantially across the regions. Numerous measures have been undertaken in the last sixty years of planning to achieve balanced regional development of the State, yet wide disparities in area development continues in this state. In the regional analysis of development one comes across regions which are well developed and the peopl e in such region enjoy reasonable standard of living while in others, resource utilization and development is low owing to historical circumstances or other wise, resulting in the underdeveloped of the region whereby people have a poor 1 standard of living. The problem of imbalance in regional development thus assumes a great significance. Regional development, therefore, is interpreted as intra-regional development design to solve the problems of regions lagging behind. The first connotation of regional is e conomic in which the differences in growth, in volume and structure of production, income, and employment are taken as the measure of economic progress. -

Section-VIII : Laboratory Services
Section‐VIII Laboratory Services 8. Laboratory Services 8.1 Haemoglobin Test ‐ State level As can be seen from the graph, hemoglobin test is being carried out at almost every FRU studied However, 10 percent medical colleges do not provide the basic Hb test. Division wise‐ As the graph shows, 96 percent of the FRUs on an average are offering this service, with as many as 13 divisions having 100 percent FRUs contacted providing basic Hb test. Hemoglobin test is not available at District Women Hospital (Mau), District Women Hospital (Budaun), CHC Partawal (Maharajganj), CHC Kasia (Kushinagar), CHC Ghatampur (Kanpur Nagar) and CHC Dewa (Barabanki). 132 8.2 CBC Test ‐ State level Complete Blood Count (CBC) test is being offered at very few FRUs. While none of the sub‐divisional hospitals are having this facility, only 25 percent of the BMCs, 42 percent of the CHCs and less than half of the DWHs contacted are offering this facility. Division wise‐ As per the graph above, only 46 percent of the 206 FRUs studied across the state are offering CBC (Complete Blood Count) test service. None of the FRUs in Jhansi division is having this service. While 29 percent of the health facilities in Moradabad division are offering this service, most others are only a shade better. Mirzapur (83%) followed by Gorakhpur (73%) are having maximum FRUs with this facility. CBC test is not available at Veerangna Jhalkaribai Mahila Hosp Lucknow (Lucknow), Sub Divisional Hospital Sikandrabad, Bullandshahar, M.K.R. HOSPITAL (Kanpur Nagar), LBS Combined Hosp (Varanasi), -

Uttar Pradesh (UP) Dominates, and Indeed Is Often
Chapter - 1 Uttar Pradesh : An Overview ttar Pradesh (UP) dominates, and indeed is often Box 1.1: Salient Demographic and Economic Features U seen to represent, the region described as the “Hindi- of the State speaking heartland” of India. UP’s population is the highest in the country and it is the fifth largest State. 1 Population, (crore) 2001 16.62 On November 9, 2000, 13 districts of the Hill region 2 Geographical area (lakh sq.km.) 2001 2.41 as well as the district of Hardwar in the west were 3 Population density (per sq.km.) 2001 689 reconstituted into the new State of Uttaranchal. At the 4 Forest area (lakh ha.) 2001-02 16.9 moment, UP covers 240928 sq.kms. and accounts for 7.3 5 Culturable waste/usar land (lakh ha.) 2001-02 11.1 percent of total area of the country, while its share in country’s population is 16.2 percent. UP is organized into 6 Fallow land (lakh ha.) 2001-02 16.5 70 districts, 300 tehsils and 813 development blocks. There 7 Cultivated Land (lakh ha.) 2001-02 168.1 are 52028 village panchayats in the State covering 97134 8 Percentage share in total workers (2001) inhabited villages. The majority of UP’s villages are small, 1. Agriculture 66.0 with an average population of around 3194 per panchayat. 2. House hold Industries 6.0 Situated in the Indo-Gangetic plain and intersected 3. Other services 28.0 by rivers, UP has had a long history of human settlement. 9 Percentage share in State Income The fertile plains of the Ganga have led to a high (2002-03) population density and the dominance of agriculture as an economic activity. -

Converting Dry Latrines in the District of Budaun, Uttar Pradesh
Converting Dry Latrines in the District of Budaun, Uttar Pradesh: A Story of Commitment, Determination and Dignity An Intiative of the District Administration, Budaun, UP August, 2011 This initiative of District Administration, Budaun was documented by UNICEF Office for Uttar Pradesh in August, 2011 EXECUTIVE SUMMARY In July 2010, a survey initiated by the district administration in rural Budaun estimated there were around 50,000 dry latrines. This meant there were about 3,00,000 users and at least 2,000 women engaged in manual scavenging across the district. The administration was moved to conduct this survey following the visit of Amit Gupta (District Magistrate, Budaun August 2009 – June 2011) to Ramzanpur, a village estimated to have more than 1200 dry latrines. The Budaun district administration took on the task of converting all dry latrines to pour flush toilets in a campaign mode: over 47,000 dry latrines have been converted in less than one year. Much of the district is now free of this practice, and work is under way to ensure the task is completed in the entire district. A dry latrine is a place to defecate in the house, which is cleaned once a day by a scavenger who removes the faeces and discards it in a field outside the village. Almost all scavengers are women and girls. Proximity of the dry latrine to living space in homes causes serious health hazards, especially among children who have a lower immunity. The campaign owes its success to the determination and commitment of a dynamic District Magistrate. Forging partnerships with multiple stakeholders, effective community mobilisation, mobilisation of all the departments falling under the district administration, quick rehabilitation of scavengers are all elements that have made this campaign a success. -

PLAGUE Amérique
— 293 — Notifications reçues du 27 mai au 2 juin 1966 — Notifications received from 27 May to 2 June 1966 PESTE — PLAGUE Asie — Asia C D c D C D INDE (suite) 17-23.IV 24-30.IV 1-7.V C D Amérique -- America INDIA (continued) VIET-NAM, REP. 22-28.V C D Bihar, State Nhatrang (PA) . 1 0 ÉQUATEUR — ECUADOR Saigon (excl. PA) . Is 0 Districts Darbhanga......................... 16/7 7p Chimborazo, Province 15-2I.V Hazanbagh ..................... 1 p Op Muzzaffarpur..................... 14P 4 p Alausi, Canton Darlac, Province Saharsa .... 36p 9p Achupallas, Parr. 6-12.UI 2 0 Banmethuot.............. 12j 0 Gujarat, State Chunchi, Canton Ninh-Thuân, Province Districts Chunchi, Parr. 17-23.IV 3 l Ahmedabad . 6p Op 12p Op Phanrang, District . 9s 0 Baroda ............................. ip Op K a ir a ................................. Ip Op El Oro, Province S u r a t ............... 42p 2p 32p ip 43p Op Ârenillas, Canton Mehsana ■ 21.V Victoria, Parr. 6-12.UI 4 0 CHOLÉRA — CHOLERA Kerala, State Pinas, Canton Trivandrum, D.................... 1P ip Marcabeli, Parr. 3-9.IV 1 0 Asie — Asia Madras, State Loja, Province C D Districts Calvas, Canton BIRMANIE — BURMA 22-28.V Chingleput . Ip Op Amaluza, Parr. 24-30.IV 1 0 M adurai............................. 1P Op ip ôp Tiruchirapalli...................... 4p Op Bassein ( P ) ............... 7 0 Celica, Canton Rangoon (PA) (excl. A) 1 0 Kanyakumari ■ 21.V Pindal, Parr. 27.UI-2.IV 1 0 15-21.V Maharashtra, State Pozul, Parr. 6-12.UI 1 0 Pegu, Division Districts Macara, Canton Hanthawaddy, District 4 1 Ahmednagar..................... 2P Op Amravati Tacamoros, Parr. -

Notice for Appointment of Regular/Rural Retail Outlets Dealerships
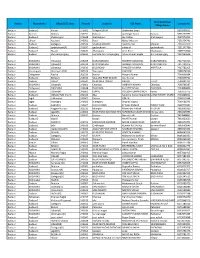
Notice for appointment of Regular/Rural Retail Outlets Dealerships Hindustan Petroleum Corporation Limited proposes to appoint Retail Outlet dealers in the State of Uttar Pradesh, as per following details: Fixed Fee Minimum Dimension (in / Min bid Security Estimated Type of Finance to be arranged by the Mode of amount ( Deposit ( Sl. No. Name Of Location Revenue District Type of RO M.)/Area of the site (in Sq. Site* applicant (Rs in Lakhs) selection monthly Sales Category M.). * Rs in Rs in Potential # Lakhs) Lakhs) 1 2 3 4 5 6 7 8 9a 9b 10 11 12 SC/SC CC 1/SC PH/ST/ST CC Estimated Estimated fund 1/ST working required for PH/OBC/OBC CC/DC/ capital Draw of Regular/Rural MS+HSD in Kls Frontage Depth Area development of CC 1/OBC CFS requirement Lots/Bidding infrastructure at PH/OPEN/OPE for operation RO N CC 1/OPEN of RO CC 2/OPEN PH ON LHS, BETWEEN KM STONE NO. 0 TO 8 ON 1 NH-AB(AGRA BYPASS) WHILE GOING FROM AGRA REGULAR 150 SC CFS 40 45 1800 0 0 Draw of Lots 0 3 MATHURA TO GWALIOR UPTO 3 KM FROM INTERSECTION OF SHASTRIPURAM- VAYUVIHAR ROAD & AGRA 2 AGRA REGULAR 150 SC CFS 20 20 400 0 0 Draw of Lots 0 3 BHARATPUR ROAD ON VAYU VIHAR ROAD TOWARDS SHASTRIPURAM ON LHS ,BETWEEN KM STONE NO 136 TO 141, 3 ALIGARH REGULAR 150 SC CFS 40 45 1800 0 0 Draw of Lots 0 3 ON BULANDSHAHR-ETAH ROAD (NH-91) WITHIN 6 KM FROM DIBAI DORAHA TOWARDS 4 NARORA ON ALIGARH-MORADABAD ROAD BULANDSHAHR REGULAR 150 SC CFS 40 45 1800 0 0 Draw of Lots 0 3 (NH 509) WITHIN MUNICIAPL LIMITS OF BADAUN CITY 5 BUDAUN REGULAR 120 SC CFS 30 30 900 0 0 Draw of Lots 0 3 ON BAREILLY -

Uttar Pradesh BSAP
NATIONAL BIODIVERSITY STRATEGY AND ACTION PLAN, UTTAR PRADESH (U.P.) Coordinator Coordinated by: U. Dhar GBPIHED TEAM S.S. Samant Asha Tewari R.S. Rawal NBSAP, U.P. Members Dr. S.S. Samant Dr. B.S. Burphal DR. Ipe M. Ipe Dr. Arun Kumar Dr. A.K. Singh Dr. S.K. Srivastava Dr. A.K. Sharma Dr. K.N. Bhatt Dr. Jamal A. Khan Miss Pia Sethi Dr. Satthya Kumar Miss Reema Banerjee Dr. Gopa Pandey Dr. Bhartendu Prakash Dr. Bhanwari Lal Suman Dr. R.D. Dixit Mr. Sameer Sinha Prof. Ajay S. Rawat 1 Contributors B.S. Burphal Pia Sethi S.K. Srivastava K.N. Bhatt D.K. pande Jamal A. Khan A.K. Sharma 2 CONTENTS CHAPTER 1. INTRODUCTION 1.1 . Brief background of the SAP 1.2 . Scope of the SAP 1.3 . Objectives of the SAP 1.4 . Contents of the SAP 1.5 . Brief description of the SAP CHAPTER 2. PROFILE OF THE AREA 2.6 . Geographical profile 2.7 . Socio- economic profile 2.8 . Political profile 2.9 . Ecological profile 2.10.Brief history CHAPTER 3. CURRENT (KNOWN) RANGE AND STATUS OF BIODIVERSITY 3.1. State of natural ecosystems and plant / animal species 3.2. State of agricultural ecosystems and domesticated plant/ animal species CHAPTER 4. STATEMENTS OF THE PROBLEMS RELATED TO BIODIVERSITY 4.1. Proximate causes of the loss of biodiversity 4.2. Root causes of the loss of biodiversity CHAPTER 5. MAJOR ACTORS AND THEIR CURRENT ROLES RELEVANT TO BIODIVERSITY 5.1. Governmental 5.2. Citizens’ groups and NGOs 5.3. Local communities, rural and urban 5.4. -
Bareilly Zone CSC List
S Grampanchayat N District Block Name Village/CSC name Pincode Location VLE Name Contact No Village Name o Badaun Budaun2 Kisrua 243601 Village KISRUA Shailendra Singh 5835005612 Badaun Gunnor Babrala 243751 Babrala Ajit Singh Yadav Babrala 5836237097 Badaun Budaun1 shahavajpur 243638 shahavajpur Jay Kishan shahavajpur 7037970292 Badaun Ujhani Nausera 243601 Rural Mukul Maurya 7351054741 Badaun Budaun Dataganj 243631 VILLEGE MARORI Ajeet Kumar Marauri 7351070370 Badaun Budaun2 qadarchowk(R) 243637 qadarchowk sifate ali qadarchowk 7351147786 Badaun Budaun1 Bisauli 243632 dhanupura Amir Khan Dhanupura 7409212060 Badaun Budaun shri narayanganj 243639 mohalla shri narayanganj Ashok Kumar Gupta shri narayanganj 7417290516 Badaun BUDAUN1 Ujhani(U) 243639 NARAYANGANJ SHOBHIT AGRAWAL NARAYANGANJ 7417721016 Badaun BUDAUN1 Ujhani(U) 243639 NARAYANGANJ SHOBHIT AGRAWAL NARAYANGANJ 7417721016 Badaun BUDAUN1 Ujhani(U) 243639 BILSI ROAD PRADEEP MISHRA AHIRTOLA 7417782205 Badaun Vazeerganj Wazirganj (NP) 202526 Wazirganj YASH PAL 7499478130 Badaun Dahgawan Nadha 202523 Nadha Mayank Kumar 7500006864 Badaun Budaun2 Bichpuri 243631 VILL AND POST MIAUN Atul Kumar 7500379752 Badaun Budaun Ushait 243641 NEAR IDEA TOWER DHRUV Ushait 7500401211 Badaun BUDAUN1 Ujhani(R) 243601 Chandau AMBRISH KUMAR Chandau 7500766387 Badaun Dahgawan DANDARA 243638 DANDARA KULDEEP SINGH DANDARA 7534890000 Badaun Budaun Ujhani(R) 243601 KURAU YOGESH KUMAR SINGH Kurau 7535079775 Badaun Budaun2 Udhaiti Patti Sharki 202524 Bilsi Sandeep Kumar ShankhdharUGHAITI PATTI SHARKI 7535868001 -

ODOP-Final-For-Digital-Low.Pdf
ODOP FINAL-NEW24.qxd 8/6/2018 3:46 PM Page 1 ODOP FINAL-NEW24.qxd 8/6/2018 3:46 PM Page 2 ODOP FINAL-NEW24.qxd 8/6/2018 3:46 PM Page 3 ODOP FINAL-NEW24.qxd 8/6/2018 3:46 PM Page 4 First published in India, 2018 Times Group A division of Books Bennett, Coleman & Co. Ltd. The Times of India, 10 Daryaganj, New Delhi-110002 Phone: 011-39843333, Email: [email protected]; www.timesgroupbooks.com Copyright ©Bennett, Coleman & Co. Ltd., 2018 All rights reserved. No part of this work may be reproduced or used in any form or by any means (graphic, electronic, mechanical, photocopying, recording, tape, web distribution, information storage and retrieval systems or otherwise) without prior written permission of the publisher. Disclaimer Due care and diligence has been taken while editing and printing the Book. Neither the Publisher nor the Printer of the Book holds any responsibility for any mistake that may have crept in inadvertently. BCCL will be free from any liability for damages and losses of any nature arising from or related to the content. All disputes are subject to the jurisdiction of competent courts in Delhi. Digital Copy. Not for Sale. Printed at: Lustra Print Process Pvt. Ltd. ODOP FINAL-NEW24.qxd 8/6/2018 3:46 PM Page 5 ODOP FINAL-NEW24.qxd 8/6/2018 3:46 PM Page 6 ODOP FINAL-NEW24.qxd 8/6/2018 3:46 PM Page 7 ODOP FINAL-NEW24.qxd 8/6/2018 3:46 PM Page 8 ODOP FINAL-NEW24.qxd 8/6/2018 3:47 PM Page 9 jke ukbZd ODOP FINAL-NEW24.qxd 8/6/2018 3:47 PM Page 10 ODOP FINAL-NEW24.qxd 8/6/2018 3:47 PM Page 11 ;ksxh vkfnR;ukFk ODOP FINAL-NEW24.qxd 8/6/2018 3:47 PM Page 12 ODOP FINAL-NEW24.qxd 8/6/2018 3:47 PM Page 13 lR;nso ipkSjh ODOP FINAL-NEW24.qxd 8/6/2018 3:47 PM Page 14 ODOP FINAL-NEW24.qxd 8/6/2018 3:47 PM Page 15 vuwi pUnz ik.Ms; ODOP FINAL-NEW24.qxd 8/6/2018 3:47 PM Page 16 Contents Introduction . -
13F O1 Lz-*Z-O
\- ;rr##..-r, ?.#prft;?-?s+YfI .f,*6ft. O F' T.' I C I] O F T I I E (] II I Ii I' E L ECTO R A I, O I,' T' I C E R. D T] I, II I OI,D S1', STI,PlIEN'S COI,I,EGF] BTIII,DING. KASIIMF]RE GATE. DEI,}{I I IOOOq No.CF.O/COE/1 02( I 0,1y 201 e/ 86 C)-A--8669 Dated 13f o1 lz-*z-o To J'hc RctLrrning O1'ficers of all 70 A(ls. Govt. ol'NC'l- of I)clhi. Sub; U Peoplc Act. 195 I . Madarn/Sir. I am directccl to lbru rrcl he rovitlr a copy of' letter no. 116lt:.(:llF.EM/CEMS- l/trLJN/DISQl2}20-l dated 1310112020 rcce ivcd liorn thc [-.lcction Commission of lrrdia on the sLrb.iect citcd abovc along with the updatcd list ol'pcrsons disqualified under Scction l0A of the Representatiorr of tlre Pcoplc Act. l95l lbr vour kind inlbrmation and necessarv action. 'l'he list of disqualilicd pcrsons is also available on thc (lorrrnission's wcbsite wrvlv.cci.gov.in and can be viervcd undcr thc hcading Judicial Rcfere ncc - List of Disqualified Persons. Yours fully. Errcl: As abovc (-r'. MISAO) Lrl,flc'llON OIIFIC t1R (COE) I qffiMffi ffiEfrrr e@-rc,"ffi*-S *::*wx vi* x*l*M,r**qr{-r*$qqqqp-tywra*.yry6m/ww4 rgaim: 13 EffiTI& ftnee -k-* $ t"ir{t +i. w41 qMr**.8ffiqffiffi tpeeqM i qrq &xrq$;* ffi3w Hffiftfu adeftqq ls** * wql lfi?s 4 e*q ffi ffier?"qi ffi ffifr q* - flnrr-H* ! qsrqql/Edrqq: q g*. -

List of Common Service Centres Established in Uttar Pradesh
LIST OF COMMON SERVICE CENTRES ESTABLISHED IN UTTAR PRADESH S.No. VLE Name Contact Number Village Block District SCA 1 Aram singh 9458468112 Fathehabad Fathehabad Agra Vayam Tech. 2 Shiv Shankar Sharma 9528570704 Pentikhera Fathehabad Agra Vayam Tech. 3 Rajesh Singh 9058541589 Bhikanpur (Sarangpur) Fatehabad Agra Vayam Tech. 4 Ravindra Kumar Sharma 9758227711 Jarari (Rasoolpur) Fatehabad Agra Vayam Tech. 5 Satendra 9759965038 Bijoli Bah Agra Vayam Tech. 6 Mahesh Kumar 9412414296 Bara Khurd Akrabad Aligarh Vayam Tech. 7 Mohit Kumar Sharma 9410692572 Pali Mukimpur Bijoli Aligarh Vayam Tech. 8 Rakesh Kumur 9917177296 Pilkhunu Bijoli Aligarh Vayam Tech. 9 Vijay Pal Singh 9410256553 Quarsi Lodha Aligarh Vayam Tech. 10 Prasann Kumar 9759979754 Jirauli Dhoomsingh Atruli Aligarh Vayam Tech. 11 Rajkumar 9758978036 Kaliyanpur Rani Atruli Aligarh Vayam Tech. 12 Ravisankar 8006529997 Nagar Atruli Aligarh Vayam Tech. 13 Ajitendra Vijay 9917273495 Mahamudpur Jamalpur Dhanipur Aligarh Vayam Tech. 14 Divya Sharma 7830346821 Bankner Khair Aligarh Vayam Tech. 15 Ajay Pal Singh 9012148987 Kandli Iglas Aligarh Vayam Tech. 16 Puneet Agrawal 8410104219 Chota Jawan Jawan Aligarh Vayam Tech. 17 Upendra Singh 9568154697 Nagla Lochan Bijoli Aligarh Vayam Tech. 18 VIKAS 9719632620 CHAK VEERUMPUR JEWAR G.B.Nagar Vayam Tech. 19 MUSARRAT ALI 9015072930 JARCHA DADRI G.B.Nagar Vayam Tech. 20 SATYA BHAN SINGH 9818498799 KHATANA DADRI G.B.Nagar Vayam Tech. 21 SATYVIR SINGH 8979997811 NAGLA NAINSUKH DADRI G.B.Nagar Vayam Tech. 22 VIKRAM SINGH 9015758386 AKILPUR JAGER DADRI G.B.Nagar Vayam Tech. 23 Pushpendra Kumar 9412845804 Mohmadpur Jadon Dankaur G.B.Nagar Vayam Tech. 24 Sandeep Tyagi 9810206799 Chhaprola Bisrakh G.B.Nagar Vayam Tech.