Collecting Sexual Orientation and Gender Identity (SO/GI) Data in Electronic Health Records
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Homophobia and Transphobia Illumination Project Curriculum
Homophobia and Transphobia Illumination Project Curriculum Andrew S. Forshee, Ph.D., Early Education & Family Studies Portland Community College Portland, Oregon INTRODUCTION Homophobia and transphobia are complicated topics that touch on core identity issues. Most people tend to conflate sexual orientation with gender identity, thus confusing two social distinctions. Understanding the differences between these concepts provides an opportunity to build personal knowledge, enhance skills in allyship, and effect positive social change. GROUND RULES (1015 minutes) Materials: chart paper, markers, tape. Due to the nature of the topic area, it is essential to develop ground rules for each student to follow. Ask students to offer some rules for participation in the postperformance workshop (i.e., what would help them participate to their fullest). Attempt to obtain a group consensus before adopting them as the official “social contract” of the group. Useful guidelines include the following (Bonner Curriculum, 2009; Hardiman, Jackson, & Griffin, 2007): Respect each viewpoint, opinion, and experience. Use “I” statements – avoid speaking in generalities. The conversations in the class are confidential (do not share information outside of class). Set own boundaries for sharing. Share air time. Listen respectfully. No blaming or scapegoating. Focus on own learning. Reference to PCC Student Rights and Responsibilities: http://www.pcc.edu/about/policy/studentrights/studentrights.pdf DEFINING THE CONCEPTS (see Appendix A for specific exercise) An active “toolkit” of terminology helps support the ongoing dialogue, questioning, and understanding about issues of homophobia and transphobia. Clear definitions also provide a context and platform for discussion. Homophobia: a psychological term originally developed by Weinberg (1973) to define an irrational hatred, anxiety, and or fear of homosexuality. -

Media Reference Guide
media reference guide NINTH EDITION | AUGUST 2014 GLAAD MEDIA REFERENCE GUIDE / 1 GLAAD MEDIA CONTACTS National & Local News Media Sports Media [email protected] [email protected] Entertainment Media Religious Media [email protected] [email protected] Spanish-Language Media GLAAD Spokesperson Inquiries [email protected] [email protected] Transgender Media [email protected] glaad.org/mrg 2 / GLAAD MEDIA REFERENCE GUIDE TABLE OF CONTENTS INTRODUCTION FAIR, ACCURATE & INCLUSIVE 4 GLOSSARY OF TERMS / LANGUAGE LESBIAN / GAY / BISEXUAL 5 TERMS TO AVOID 9 TRANSGENDER 12 AP & NEW YORK TIMES STYLE 21 IN FOCUS COVERING THE BISEXUAL COMMUNITY 25 COVERING THE TRANSGENDER COMMUNITY 27 MARRIAGE 32 LGBT PARENTING 36 RELIGION & FAITH 40 HATE CRIMES 42 COVERING CRIMES WHEN THE ACCUSED IS LGBT 45 HIV, AIDS & THE LGBT COMMUNITY 47 “EX-GAYS” & “CONVERSION THERAPY” 46 LGBT PEOPLE IN SPORTS 51 DIRECTORY OF COMMUNITY RESOURCES 54 GLAAD MEDIA REFERENCE GUIDE / 3 INTRODUCTION Fair, Accurate & Inclusive Fair, accurate and inclusive news media coverage has played an important role in expanding public awareness and understanding of lesbian, gay, bisexual and transgender (LGBT) lives. However, many reporters, editors and producers continue to face challenges covering these issues in a complex, often rhetorically charged, climate. Media coverage of LGBT people has become increasingly multi-dimensional, reflecting both the diversity of our community and the growing visibility of our families and our relationships. As a result, reporting that remains mired in simplistic, predictable “pro-gay”/”anti-gay” dualisms does a disservice to readers seeking information on the diversity of opinion and experience within our community. Misinformation and misconceptions about our lives can be corrected when journalists diligently research the facts and expose the myths (such as pernicious claims that gay people are more likely to sexually abuse children) that often are used against us. -

Transfeminist Perspectives in and Beyond Transgender and Gender Studies
Transfeminist Perspectives Edited by ANNE ENKE Transfeminist Perspectives in and beyond Transgender and Gender Studies TEMPLE UNIVERSITY PRESS Philadelphia TEMPLE UNIVERSITY PRESS Philadelphia, Pennsylvania 19122 www.temple.edu/tempress Copyright © 2012 by Temple University All rights reserved Published 2012 Library of Congress Cataloging-in-Publication Data Transfeminist perspectives in and beyond transgender and gender studies / edited by Anne Enke. p. cm. Includes bibliographical references and index. ISBN 978-1-4399-0746-7 (cloth : alk. paper) ISBN 978-1-4399-0747-4 (pbk. : alk. paper) ISBN 978-1-4399-0748-1 (e-book) 1. Women’s studies. 2. Feminism. 3. Transgenderism. 4. Transsexualism. I. Enke, Anne, 1964– HQ1180.T72 2012 305.4—dc23 2011043061 Th e paper used in this publication meets the requirements of the American National Standard for Information Sciences—Permanence of Paper for Printed Library Materials, ANSI Z39.48-1992 Printed in the United States of America 2 4 6 8 9 7 5 3 1 Contents Acknowledgments vii Introduction: Transfeminist Perspectives 1 A. Finn Enke Note on Terms and Concepts 16 A. Finn Enke PART I “This Much Knowledge”: Flexible Epistemologies 1 Gender/Sovereignty 23 Vic Muñoz 2 “Do Th ese Earrings Make Me Look Dumb?” Diversity, Privilege, and Heteronormative Perceptions of Competence within the Academy 34 Kate Forbes 3 Trans. Panic. Some Th oughts toward a Th eory of Feminist Fundamentalism 45 Bobby Noble 4 Th e Education of Little Cis: Cisgender and the Discipline of Opposing Bodies 60 A. Finn Enke PART II Categorical Insuffi ciencies and “Impossible People” 5 College Transitions: Recommended Policies for Trans Students and Employees 81 Clark A. -
The Audre Lorde Project
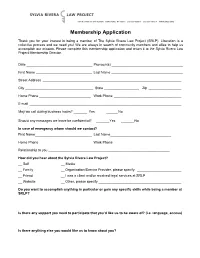
Membership Application Thank you for your interest in being a member of The Sylvia Rivera Law Project (SRLP). Liberation is a collective process and we need you! We are always in search of community members and allies to help us accomplish our mission. Please complete this membership application and return it to the Sylvia Rivera Law Project Membership Director. Date Pronoun(s) First Name Last Name Street Address ________________________________________________________________________ City State __________________ Zip _________________ Home Phone ___________________________ Work Phone ___________________________________ E-mail _______________________________________________________________________________ May we call during business hours? _______ Yes ______ No Should any messages we leave be confidential? Yes No In case of emergency whom should we contact? First Name Last Name Home Phone ___________________________ Work Phone _____________________________ Relationship to you _______________________________________________________________ How did you hear about the Sylvia Rivera Law Project? __ Self __ Media __ Family __ Organization/Service Provider, please specify _______________________ __ Friend __ I was a client and/or received legal services at SRLP __ Website __ Other, please specify ___________________________________________ Do you want to accomplish anything in particular or gain any specific skills while being a member at SRLP? Is there any support you need to participate that you’d like us to be aware of? (i.e. language, access) Is there anything else you would like us to know about you? MEDIA RELEASE: I _________________________ (print name) give the Sylvia Rivera Law Project (SRLP) permission to use my image, audio, writing, and photograph in any print, online, video, or other form of media/communications. I understand that I will not be compensated and release SRLP from any and all claims in connection with the use of my image or name, likeness and identity including any claims for libel or publicity. -

Trans Issues and Later Life
Factsheet 16 Trans issues and later life July 2021 About this factsheet This factsheet provides information about later life for trans people. The main focus is on growing older for people who have transitioned and live permanently in their affirmed gender. It also provides information for people in later life who are thinking about gender reassignment. The factsheet covers a range of legal, financial and social care issues. It includes a guide to terminology and details of where to go for further information and support. Terminology used by trans people to describe their experiences and identities is varied and changes over time. We are committed to reflecting this diversity but recognise that terms used in this factsheet may vary in their usage or become outdated. The information in this factsheet is applicable to England and Wales. If you are in Scotland or Northern Ireland, please contact Age Scotland or Age NI for information. Contact details are at the back of the factsheet. Age UK Advice can give you contact details for a local Age UK in England. In Wales, call Age Cymru Advice. Contact details for any organisation mentioned in this factsheet can be found in the Useful organisations section. Page 1 of 32 Contents 1 Recent developments 4 2 Who is trans? 4 3 Trans and other gender identities 5 3.1 Transsexual people 5 3.2 People who cross-dress 6 3.3 Non-binary people 6 4 Transitioning in later life 7 5 The transitioning process 7 5.1 Transition and hormones 9 5.1.1 The trans man’s transition 9 5.1.2 The trans woman’s transition -
Trans Resources Helpful Organizations, Products, and Information
Trans Resources Helpful Organizations, Products, and Information Contents Coming Out As Transgender ......................................................................................................................... 2 Transition ...................................................................................................................................................... 2 . DFAB Appearance ............................................................................................................................ 3 . DMAB Appearance ........................................................................................................................... 4 Healthcare, Hormones & Surgery ................................................................................................................. 5 Trans Rights ................................................................................................................................................... 7 Emergency/Crisis Support ............................................................................................................................. 8 Spiritual & Religious Support ........................................................................................................................ 9 Advocacy in Schools .................................................................................................................................... 10 Employment ............................................................................................................................................... -

How Trans People Simultaneously Challenge and Reproduce
Complicating Normal: How Trans People Simultaneously Challenge and Reproduce Heteronormativity A thesis presented to the faculty of the College of Arts and Sciences of Ohio University Master of Arts Katherine M. Kassner August 2010 © 2010 Katherine M. Kassner. All Rights Reserved. 2 This thesis titled Complicating Normal: How Trans People Simultaneously Challenge and Reproduce Heteronormativity By KATHERINE M. KASSNER has been approved for the Department of Sociology and Anthropology and the College of Arts and Sciences by ________________________________________ Cynthia D. Anderson Associate Professor of Sociology and Anthropology ________________________________________ Benjamin M. Ogles Dean, College of Arts and Sciences 3 ABSTRACT KASSNER, KATHERINE M., M.A., August 2010, Sociology Complicating Normal: How Trans People Simultaneously Challenge and Reproduce Heteronormativity (84 pp.) Director of Thesis: Cynthia D. Anderson This thesis examines the interactions between trans people and structural heteronormativity. Twenty-five in-depth interviews were conducted with self-identified trans people to assess how interviewees feel they’ve been affected by structural heteronormativity across the institutions of marriage, family, healthcare, education, and work. Interview questions further examined whether interviewees feel they challenge or reproduce structural heteronormativity. Analytic induction was used to analyze the interview data. Results demonstrate that all interviewees identify that they challenge structural heteronormativity and slightly more than half of interviewees identify that they reproduce structural heteronormativity. However, further analysis of the data suggests that some interviewees may challenge or reproduce heteronormativity at an individual level and had no effect or sometimes the opposite effect at the structural level. These findings were highly dependent on whether interviewees identify themselves as out or stealth as a trans person. -

Transfeminist Perspectives in and Beyond Transgender and Gender Studies Seeks to Highlight the Productive and Sometimes Fraught Potential of This Relationship
A. FINN ENKE Introduction Transfeminist Perspectives his book is born of the conviction that feminist studies and transgender studies are intimately connected to one another in their endeavor to T analyze epistemologies and practices that produce gender. Despite this connection, they are far from integrated. Transfeminist Perspectives in and beyond Transgender and Gender Studies seeks to highlight the productive and sometimes fraught potential of this relationship. Feminist, women’s, and gender studies grew partly from Simone de Beauvoir’s observation that “one is not born, but rather becomes, a woman.”1 Transgender studies extends this founda- tion, emphasizing that there is no natural process by which anyone becomes woman, and also that everyone’s gender is made: Gender, and also sex, are made through complex social and technical manipulations that naturalize some while abjecting others. In this, both feminist and transgender studies acknowledge the mutual imbrications of gender and class formations, dis/abilities, racializations, political economies, incarcerations, nationalisms, migrations and dislocations, and so forth. We share, perhaps, a certain delight and trepidation in the aware- ness that gender is trouble: Gender may trouble every imaginable social relation and fuel every imaginable social hierarchy; it may also threaten to undo itself and us with it, even as gender scholars simultaneously practice, undo, and rein- vest in gender.2 Women’s and gender studies have registered increasing interest in things transgender since the mid-1990s. Scholars have organized conferences on the topic, and numerous feminist journals have published special transgender issues.3 Th is interest has been inspired in part by inquiry into the meanings of gender, bodies, and embodiment, by transnational and cross-cultural studies that address the varied ways in which cultures ascribe gender, and also by insti- tutional practices that circumscribe or broaden the range of gender legibility. -
IPGLBT's Pride Guide
Pride Guide IPGLBT 2019 Letter from the Editor Last year, IPGLBT tried something different. We This year, we are also using the Pride flag that created the first edition of the Pride Guide with includes the black and brown stripe, introduced helpful information, programming examples, in June 2017 by the City of Philadelphia (with and featured resources and insights to help the help of IPG’s own Tierney). While not an offices and employees learn more about the “official” Pride flag, we feel the inclusion of the LGBTQ+ community. The feedback received black and brown stripe calls attention to the from employees and executives was extremely marginalization and, sometimes, intentional positive and also served as a catalyst for more exclusion of people of color from the LGBTQ+ employees across the network to learn more narrative. about and join IPGLBT. As always, something like this is a team But with all the good we are doing at IPG, the effort and I would like to thank David Azulay, LGBTQ+ community has taken a few hits in Christina Cairns, Barbara Harris, Melynda the last year as well. We have seen a roll back Rowe, and Jeremy Thomas as well as all the in protections for employment and public fabulous individuals who have taken time accommodations. We’ve seen the Pentagon out of their busy schedules to dial in for the issues a policy banning trans individuals national calls, push us to do more, and share from serving openly in the military and the their perspectives. I also want to thank the IPG Department of Health and Human Services Diversity & Inclusion Team including Heide (along with several state legislatures) working Gardner, Bridgette O’Neal, and Sandy Chum- to deny healthcare coverage to trans people. -

Heterosexual College Students Who Hookup with Same-Sex Partners
Archives of Sexual Behavior https://doi.org/10.1007/s10508-018-1194-7 ORIGINAL PAPER Heterosexual College Students Who Hookup with Same‑Sex Partners Arielle Kuperberg1 · Alicia M. Walker2 Received: 9 December 2016 / Revised: 13 March 2018 / Accepted: 14 March 2018 © Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract Individuals who identify as heterosexual but engage in same-sex sexual behavior fascinate both researchers and the media. We analyzed the Online College Social Life Survey dataset of over 24,000 undergraduate students to examine students whose last hookup was with a same-sex partner (N = 383 men and 312 women). The characteristics of a signifcant minority of these students (12% of men and 25% of women) who labelled their sexual orientation “heterosexual” difered from those who self- identifed as “homosexual,” “bisexual,” or “uncertain.” Diferences among those who identifed as heterosexual included more conservative attitudes, less prior homosexual and more prior heterosexual sexual experience, features of the hookups, and sentiments about the encounter after the fact. Latent class analysis revealed six distinctive “types” of heterosexually identifed students whose last hookup was with a same-sex partner. Three types, comprising 60% of students, could be clas- sifed as mostly private sexual experimentation among those with little prior same-sex experience, including some who did not enjoy the encounter; the other two types in this group enjoyed the encounter, but difered on drunkenness and desire for -

I Think I Might Be Gay Pamphlet
University of Rhode Island DigitalCommons@URI The ommittC ee to Eliminate Heterosexism and Gender and Sexuality Center Homophobia 1990 I think I Might be Gay Pamphlet Follow this and additional works at: https://digitalcommons.uri.edu/cmte-eliminate Recommended Citation "I think I Might be Gay Pamphlet" (1990). The Committee to Eliminate Heterosexism and Homophobia. Paper 182. https://digitalcommons.uri.edu/cmte-eliminate/182https://digitalcommons.uri.edu/cmte-eliminate/182 This Pamphlet is brought to you for free and open access by the Gender and Sexuality Center at DigitalCommons@URI. It has been accepted for inclusion in The ommittC ee to Eliminate Heterosexism and Homophobia by an authorized administrator of DigitalCommons@URI. For more information, please contact [email protected]. • Toll-free Hotlines I think I might You may want to call a hotline to speak to someone about being gay. You may want to be gay . .. call from a phone booth for privacy The people at the hotline will let you talk about your feelings, and will direct you to organiza tions that help gay people There may even be a gay youth group in your area. These hotline numbers are accurate as of ;\ugust 1990 and are toll-free from anywhere in the United States. Hotlines sometimes This brochure was written by Kevin Cran change If these don't work, try looking in a ston and Cooper Thompson with help from phone book. Most major cities have a lesbian members of BAGLY, Boston Alliance of Gay and gay hotline and Lesbian Youth, Inc r,Jational Lesbian and Gay Hotline: Produced and distributed by The Cam 1-800-SOS-GA YS paign to End Homophobia. -

Masculinity As Prison: Sexual Identity, Race, and Incarceration Russell K
Berkeley Law Berkeley Law Scholarship Repository Faculty Scholarship 1-1-2011 Masculinity as Prison: Sexual Identity, Race, and Incarceration Russell K. Robinson Berkeley Law Follow this and additional works at: http://scholarship.law.berkeley.edu/facpubs Part of the Law Commons Recommended Citation Russell K. Robinson, Masculinity as Prison: Sexual Identity, Race, and Incarceration, 99 Cal. L. Rev. 1309 (2011) This Article is brought to you for free and open access by Berkeley Law Scholarship Repository. It has been accepted for inclusion in Faculty Scholarship by an authorized administrator of Berkeley Law Scholarship Repository. For more information, please contact [email protected]. Masculinity as Prison: Sexual Identity, Race, and Incarceration Russell K. Robinson* The Los Angeles County Men's Jail segregatesgay and transgender inmates and says that it does so to protect them from sexual assault. But not all gay and transgenderinmates qualify for admission to the K6G unit. Transgender inmates must appear transgender to staff that inspect them. Gay men must identify as gay in a public space and then satisfactorily answer a series of cultural questions designed to determine whether they really are gay. This policy creates harms for those who are excluded, including vulnerable heterosexual and bisexual men, men who have sex with men but do not embrace gay identity, and gay-identified men who do not mimic white, affluent gay culture. Further,the policy harms those who are included in that it stereotypes them as inherent victims, exposes them to a heightened risk of HIV transmission, and disrupts relationships that cut across gender identity and sexual orientation.