Histopathological Spectrum of Psoriasiform Dermatitis Jayalakshmy PL1, Babitha AM2, Sankar S1, Nandakumar G3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Diagnostic Approach to Pruritus
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by DigitalCommons@University of Nebraska University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln U.S. Air Force Research U.S. Department of Defense 2011 A Diagnostic Approach to Pruritus Brian V. Reamy Christopher W. Bunt Stacy Fletcher Follow this and additional works at: https://digitalcommons.unl.edu/usafresearch This Article is brought to you for free and open access by the U.S. Department of Defense at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in U.S. Air Force Research by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. A Diagnostic Approach to Pruritus BRIAN V. REAMY, MD, Uniformed Services University of the Health Sciences, Bethesda, Maryland CHRISTOPHER W. BUNT, MAJ, USAF, MC, and STACY FLETCHER, CAPT, USAF, MC Ehrling Bergquist Family Medicine Residency Program, Offutt Air Force Base, Nebraska, and the University of Nebraska Medical Center, Omaha, Nebraska Pruritus can be a symptom of a distinct dermatologic condition or of an occult underlying systemic disease. Of the patients referred to a dermatologist for generalized pruritus with no apparent primary cutaneous cause, 14 to 24 percent have a systemic etiology. In the absence of a primary skin lesion, the review of systems should include evaluation for thyroid disorders, lymphoma, kidney and liver diseases, and diabetes mellitus. Findings suggestive of less seri- ous etiologies include younger age, localized symptoms, acute onset, involvement limited to exposed areas, and a clear association with a sick contact or recent travel. Chronic or general- ized pruritus, older age, and abnormal physical findings should increase concern for underly- ing systemic conditions. -

FIG. 4A © O O Wo 2015/042110 Al III III II II III III 1 1 II III II II III III II III
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date W O 2015/042110 A l 2 6 March 2015 (26.03.2015) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61P 37/00 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/US20 14/056021 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, ΓΝ , IR, IS, JP, KE, KG, KN, KP, KR, 17 September 2014 (17.09.2014) KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, (25) Filing Language: English PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, (26) Publication Language: English SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 61/880,522 20 September 2013 (20.09.2013) (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant: CHILDREN'S MEDICAL CENTER COR¬ GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, PORATION [US/US]; 55 Shattuck Street, Boston, Mas¬ TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, sachusetts 021 15 (US). -

ORIGINAL ARTICLE a Clinical and Histopathological Study of Lichenoid Eruption of Skin in Two Tertiary Care Hospitals of Dhaka
ORIGINAL ARTICLE A Clinical and Histopathological study of Lichenoid Eruption of Skin in Two Tertiary Care Hospitals of Dhaka. Khaled A1, Banu SG 2, Kamal M 3, Manzoor J 4, Nasir TA 5 Introduction studies from other countries. Skin diseases manifested by lichenoid eruption, With this background, this present study was is common in our country. Patients usually undertaken to know the clinical and attend the skin disease clinic in advanced stage histopathological pattern of lichenoid eruption, of disease because of improper treatment due to age and sex distribution of the diseases and to difficulties in differentiation of myriads of well assess the clinical diagnostic accuracy by established diseases which present as lichenoid histopathology. eruption. When we call a clinical eruption lichenoid, we Materials and Method usually mean it resembles lichen planus1, the A total of 134 cases were included in this study prototype of this group of disease. The term and these cases were collected from lichenoid used clinically to describe a flat Bangabandhu Sheikh Mujib Medical University topped, shiny papular eruption resembling 2 (Jan 2003 to Feb 2005) and Apollo Hospitals lichen planus. Histopathologically these Dhaka (Oct 2006 to May 2008), both of these are diseases show lichenoid tissue reaction. The large tertiary care hospitals in Dhaka. Biopsy lichenoid tissue reaction is characterized by specimen from patients of all age group having epidermal basal cell damage that is intimately lichenoid eruption was included in this study. associated with massive infiltration of T cells in 3 Detailed clinical history including age, sex, upper dermis. distribution of lesions, presence of itching, The spectrum of clinical diseases related to exacerbating factors, drug history, family history lichenoid tissue reaction is wider and usually and any systemic manifestation were noted. -

Common Dermatoses in Patients with Obsessive Compulsive Disorders Mircea Tampa Carol Davila University of Medicine and Pharmacy, Tampa [email protected]
Journal of Mind and Medical Sciences Volume 2 | Issue 2 Article 7 2015 Common Dermatoses in Patients with Obsessive Compulsive Disorders Mircea Tampa Carol Davila University of Medicine and Pharmacy, [email protected] Maria Isabela Sarbu Victor Babes Hospital for Infectious and Tropical Diseases, [email protected] Clara Matei Carol Davila University of Medicine and Pharmacy Vasile Benea Victor Babes Hospital for Infectious and Tropical Diseases Simona Roxana Georgescu Carol Davila University of Medicine and Pharmacy Follow this and additional works at: http://scholar.valpo.edu/jmms Part of the Medicine and Health Sciences Commons Recommended Citation Tampa, Mircea; Sarbu, Maria Isabela; Matei, Clara; Benea, Vasile; and Georgescu, Simona Roxana (2015) "Common Dermatoses in Patients with Obsessive Compulsive Disorders," Journal of Mind and Medical Sciences: Vol. 2 : Iss. 2 , Article 7. Available at: http://scholar.valpo.edu/jmms/vol2/iss2/7 This Review Article is brought to you for free and open access by ValpoScholar. It has been accepted for inclusion in Journal of Mind and Medical Sciences by an authorized administrator of ValpoScholar. For more information, please contact a ValpoScholar staff member at [email protected]. JMMS 2015, 2(2): 150- 158. Review Common dermatoses in patients with obsessive compulsive disorders Mircea Tampa1, Maria Isabela Sarbu2, Clara Matei1, Vasile Benea2, Simona Roxana Georgescu1 1 Carol Davila University of Medicine and Pharmacy, Department of Dermatology and Venereology 2 Victor Babes Hospital for Infectious and Tropical Diseases, Department of Dermatology and Venereology Corresponding author: Maria Isabela Sarbu, e-mail: [email protected] Running title: Dermatoses in obsessive compulsive disorders Keywords: Factitious disorders, obsessive-compulsive disorders, acne excoriee www.jmms.ro 2015, Vol. -

Lichen Simplex Chronicus
LICHEN SIMPLEX CHRONICUS http://www.aocd.org Lichen simplex chronicus is a localized form of lichenified (thickened, inflamed) atopic dermatitis or eczema that occurs in well defined plaques. It is the result of ongoing, chronic rubbing and scratching of the skin in localized areas. It is generally seen in patients greater than 20 years of age and is more frequent in women. Emotional stress can play a part in the course of this skin disease. There is mainly one symptom: itching. The rubbing and scratching that occurs in response to the itch can become automatic and even unconscious making it very difficult to treat. It can be magnified by seeming innocuous stimuli such as putting on clothes, or clothes rubbing the skin which makes the skin warmer resulting in increased itch sensation. The lesions themselves are generally very well defined areas of thickened, erythematous, raised area of skin. Frequently they are linear, oval or round in shape. Sites of predilection include the back of the neck, ankles, lower legs, upper thighs, forearms and the genital areas. They can be single lesions or multiple. This can be a very difficult condition to treat much less resolve. It is of utmost importance that the scratching and rubbing of the skin must stop. Treatment is usually initiated with topical corticosteroids for larger areas and intralesional steroids might also be considered for small lesion(s). If the patient simply cannot keep from rubbing the area an occlusive dressing might be considered to keep the skin protected from probing fingers. Since this is not a histamine driven itch phenomena oral antihistamines are generally of little use in these cases. -

Triamcinolone Acetonide Injectable Suspension, USP)
KENALOG®-10 INJECTION (triamcinolone acetonide injectable suspension, USP) NOT FOR USE IN NEONATES CONTAINS BENZYL ALCOHOL For Intra-articular or Intralesional Use Only NOT FOR INTRAVENOUS, INTRAMUSCULAR, INTRAOCULAR, EPIDURAL, OR INTRATHECAL USE DESCRIPTION Kenalog®-10 Injection (triamcinolone acetonide injectable suspension, USP) is triamcinolone acetonide, a synthetic glucocorticoid corticosteroid with marked anti-inflammatory action, in a sterile aqueous suspension suitable for intralesional and intra-articular injection. THIS FORMULATION IS SUITABLE FOR INTRA-ARTICULAR AND INTRALESIONAL USE ONLY. Each mL of the sterile aqueous suspension provides 10 mg triamcinolone acetonide, with 0.66% sodium chloride for isotonicity, 0.99% (w/v) benzyl alcohol as a preservative, 0.63% carboxymethylcellulose sodium, and 0.04% polysorbate 80. Sodium hydroxide or hydrochloric acid may have been added to adjust pH between 5.0 and 7.5. At the time of manufacture, the air in the container is replaced by nitrogen. The chemical name for triamcinolone acetonide is 9-Fluoro-11β,16α,17,21-tetrahydroxypregna- 1,4-diene-3,20-dione cyclic 16,17-acetal with acetone. Its structural formula is: 1 Reference ID: 4241593 MW 434.50 CLINICAL PHARMACOLOGY Glucocorticoids, naturally occurring and synthetic, are adrenocortical steroids that are readily absorbed from the gastrointestinal tract. Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt- retaining properties, are used as replacement therapy in adrenocortical deficiency states. -

2016 Essentials of Dermatopathology Slide Library Handout Book
2016 Essentials of Dermatopathology Slide Library Handout Book April 8-10, 2016 JW Marriott Houston Downtown Houston, TX USA CASE #01 -- SLIDE #01 Diagnosis: Nodular fasciitis Case Summary: 12 year old male with a rapidly growing temple mass. Present for 4 weeks. Nodular fasciitis is a self-limited pseudosarcomatous proliferation that may cause clinical alarm due to its rapid growth. It is most common in young adults but occurs across a wide age range. This lesion is typically 3-5 cm and composed of bland fibroblasts and myofibroblasts without significant cytologic atypia arranged in a loose storiform pattern with areas of extravasated red blood cells. Mitoses may be numerous, but atypical mitotic figures are absent. Nodular fasciitis is a benign process, and recurrence is very rare (1%). Recent work has shown that the MYH9-USP6 gene fusion is present in approximately 90% of cases, and molecular techniques to show USP6 gene rearrangement may be a helpful ancillary tool in difficult cases or on small biopsy samples. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors, 5th edition. Mosby Elsevier. 2008. Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011 Oct;91(10):1427-33. Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013 Jul;463(1):97-8. CONTRIBUTED BY KAREN FRITCHIE, MD 1 CASE #02 -- SLIDE #02 Diagnosis: Cellular fibrous histiocytoma Case Summary: 12 year old female with wrist mass. -

Seborrheic Dermatitis
432 Teams Dermatology Done by: Wael Al Saleh & Abdulrahman Al-Akeel Reviewer: Wael Al Saleh & Abdulrahman Al-Akeel 9 Team Leader: Basil Al Suwaine Color Code: Original, Team’s note, Important, Doctor’s note, Not important, Old teamwork 432 Dermatology Team Lecture 9: Atopic dermatitis/ Eczema Objectives 1- To know the definition & classification of Dermatitis/Eczema 2- To recognize the primary presentation of different types of eczema 3- To understand the possible pathogenesis of each type of eczema 4- To know the scheme of managements lines P a g e | 1 432 Dermatology Team Lecture 9: Atopic dermatitis/ Eczema Introduction: A groups and spectrum of related disorders with pruritus being the hallmark of the disease, they also come with dry skin. Every atopic dermatitis is eczema but not every eczema are atopic dermatitis. Atopic dermatitis mean that the patient has eczema (excoriated skin, itching and re-onset) and atopy (atopy; the patient or one of his family has allergic rhinitis, asthma or eczema). It starts early of life (eczema can happen at any time). It classified as: - Acute, characterized by erythema, papules, vesicles, oozing, and crusting. - Subacute, clinically it is represented by erythema, scaling, and crusting. - Chronic, presents with thickening of the skin, skin markings become prominent (lichenification); pigmentation and fissuring of the skin occur. Acute on top of chronic very dry 4 years old boy with chronic, itchy, well defined brownish plaque with bleeding plaques. lichenifications. Ill defined plaques Well defined erythematous excoriated Lichenification is the hallmark for plaques on both cheeks with erosion. chronic course. P a g e | 2 432 Dermatology Team Lecture 9: Atopic dermatitis/ Eczema Dermatitis Classification of dermatitis: Atopic, more common in children Seborrheic (oily skin)- (like naso-labial folds, scalp, ears) Contact dermatitis, substance cause eczema - Allergic - Irritant Nummular, coined shape, usually in the shin. -
Xerotic Eczema
433 Dermatology Team Other type of eczema Lecture(10) Other type of eczema [email protected] 1 | P a g e 433 Dermatology Team Other type of eczema Content of lecture: To know the classification of Eczema. To recognize the primary presentation of different types of eczema. To understand the possible pathogenesis of each type of eczema. To know the scheme of managements lines. Color index: slides, doctor notes, 432 notes, Important 2 | P a g e 433 Dermatology Team Other type of eczema 1-Nummular Dermatitis: Coin shaped patches and plaques Secondary to xerosis cutis Primary symptom itch Notice the surrounding xerosis 2- Regional Eczema: A. Ear eczema B. Eyelid dermatitis Note: using of moisturizing C. Nipple eczema woreworse perorbital D. Hand eczema dermatitis. E. Diaper dermatitis F. Juvenile plantar dermatosis A- Ear Eczema Most frequently caused by seborrheic or atopic dermatitis Staph, Strep, or Psoeudomonas Earlobe is pathognomonic of nickel allergy B- Eyelid dermatitis When on one eye only, it is most frequently caused by nail polish When both eyelids are involved, consider mascara, eye shadow, eyelash cement, eyeliner, etc 3 | P a g e 433 Dermatology Team Other type of eczema C- Nipple eczema Painful fissuring, seen especially in nursing mothers. Maybe an isolated manifestation of atopic dermatitis. If persist more than 3 month, and/or unilateral, biopsy is mandatory to rule out Pagets disease . D- Hand eczema Spongiosis histologically . Irritant hand dermatitis- seen in homemakers, nurses. Resulting from excessive exposure to soaps. Pompholyx- tapioca vesicles, on sides of fingers, palms, and soles. Irritant versus allergic. Note: Adult atopic dermatitis has the greatest risk for hand dermatitis E- Juvenile plantar dermatitis Begins as a patchy symmetrical, smooth, red, glazed macules on the base of the great toes Affect age 3 to puberty. -

Common Skin Conditions in Children
Common Skin Conditions in Children Liz Moore and Emma King Dermatology Nurse Consultants Diagnosis? Nummular Dermatitis Disc pattern rash (discoid eczema) Clearly demarcated edges Occurs at any age Can be associated with atopic eczema Itchy Surrounding skin not as dry at atopic eczema Prone to secondary bacterial infection Often thought to be ringworm Treatment General eczema management More resistant to treatment May require more intensive wet dressing application and admission Potent topical steroids Tar preparations Phototherapy (UV radiation) Intralesional steroid injections – nodular prurigo Diagnosis? Eczema Herpeticum Herpes simplex virus 1 Affinity for the skin and nervous system Fluid filled blisters – vesicles Multiple crusted erosions Grouped, punched out Painful, increased itch Viral swab Maybe unwell – fever and malaise Secondary bacterial infection Treatment NO TOPICAL STEROIDS Remove crusts – soaks or compresses +/- oral/IV Acylovir Most often oral Keflex Admission prn – severe extensive disease Ophthalmology review if involves the eyes Diagnosis? Molluscum Contagiosum Caused by a harmless virus (MCV) Poxvirus Very common in children Transmitted by swimming pools, sharing baths, towels and direct contact In adults most often a sexually acquired infection Pearly papule Central dimple and core Treatment Self limiting, but may take up to 2 years Complicated by atopic eczema Treatment involves irritating the lesions – Burow’s solution diluted 1:10, Benzac gel, occlusive tape, Aldara, Cantharone -
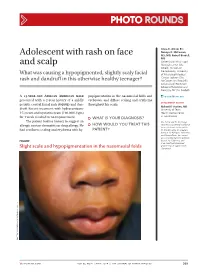
Adolescent with Rash on Face and Scalp
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

My Approach to Superficial Inflammatory Dermatoses K O Alsaad, D Ghazarian
1233 J Clin Pathol: first published as 10.1136/jcp.2005.027151 on 25 November 2005. Downloaded from REVIEW My approach to superficial inflammatory dermatoses K O Alsaad, D Ghazarian ............................................................................................................................... J Clin Pathol 2005;58:1233–1241. doi: 10.1136/jcp.2005.027151 Superficial inflammatory dermatoses are very common and diagnosis of inflammatory skin diseases, there are limitations to this approach. The size of the comprise a wide, complex variety of clinical conditions. skin biopsy should be adequate and representa- Accurate histological diagnosis, although it can sometimes tive of all four compartments and should also be difficult to establish, is essential for clinical include hair follicles. A 2 mm punch biopsy is too small to represent all compartments, and often management. Knowledge of the microanatomy of the skin insufficient to demonstrate a recognisable pat- is important to recognise the variable histological patterns tern. A 4 mm punch biopsy is preferred, and of inflammatory skin diseases. This article reviews the non- usually adequate for the histological evaluation of most inflammatory dermatoses. However, a vesiculobullous/pustular inflammatory superficial larger biopsy (6 mm punch biopsy), or even an dermatoses based on the compartmental microanatomy of incisional biopsy, might be necessary in panni- the skin. culitis or cutaneous lymphoproliferative disor- ders. A superficial or shave biopsy should be ..........................................................................