Measurement of Blood Pressure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypertension – Adult – Clinical Practice Guideline
Hypertension – Adult – Clinical Practice Guideline Table of Contents EXECUTIVE SUMMARY ........................................................................................................... 3 SCOPE ...................................................................................................................................... 4 METHODOLOGY ...................................................................................................................... 5 INTRODUCTION ....................................................................................................................... 5 RECOMMENDATIONS .............................................................................................................. 5 Establish the Diagnosis ........................................................................................... 5 Patient Evaluation ................................................................................................... 7 Treatment Goals ..................................................................................................... 7 Lifestyle Modifications ............................................................................................. 8 Table 4 – Lifestyle Modifications ........................................................................ 9 Medication Treatment............................................................................................ 11 Figure 1 - Initiation and Titration of Antihypertensive Medication ..................... 13 Table 7 - Antihypertensive -
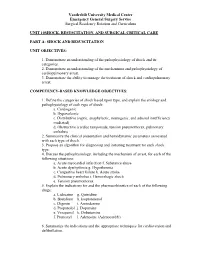
Unit 10 Shock,Resuscitation Part A
Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum UNIT 10SHOCK, RESUSCITATION, AND SURGICAL CRITICAL CARE PART A: SHOCK AND RESUSCITATION UNIT OBJECTIVES: 1. Demonstrate an understanding of the pathophysiology of shock and its categories. 2. Demonstrate an understanding of the mechanisms and pathophysiology of cardiopulmonary arrest. 3. Demonstrate the ability to manage the treatment of shock and cardiopulmonary arrest. COMPETENCY-BASED KNOWLEDGE OBJECTIVES: 1. Define the categories of shock based upon type, and explain the etiology and pathophysiology of each type of shock: a. Cardiogenic b. Hypovolemic c. Distributive (septic, anaphylactic, neurogenic, and adrenal insufficiency mediated) d. Obstructive (cardiac tamponade, tension pneumothorax, pulmonary embolus) 2. Summarize the clinical presentation and hemodynamic parameters associated with each type of shock. 3. Propose an algorithm for diagnosing and initiating treatment for each shock type. 4. Discuss the pathophysiology, including the mechanism of arrest, for each of the following situations: a. Acute myocardial infarction f. Substance abuse b. Acute dysrhythmia g. Hypothermia c. Congestive heart failure h. Acute stroke d. Pulmonary embolus i. Hemorrhagic shock e. Tension pneumothorax 5. Explain the indications for and the pharmacokinetics of each of the following drugs: a. Lidocaine g. Quinidine b. Bretylium h. Isoproterenol c. Digoxin i. Amiodarone d. Propanolol j. Dopamine e. Verapamil k. Dobutamine f. Pronestyl l. Adenosine (Adenocard®) 6. Summarize the indications and the appropriate techniques for cardioversion and defibrillation. Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum 7. Outline the signs and symptoms of acute airway obstruction and define the appropriate intervention in adult and pediatric patients. -

Complex Hypertension
COMPLEX HYPERTENSION Anita Ralstin, FNP-BC Next Step Health Consultant, LLC Incidence Of Hypertension ¨ About 70 million American adults have high blood pressure. About 33% of the population ¨ Only 52% have BP under control. ¨ Nearly a third of US adults have prehypertension. ¨ Hypertension costs $46 billion a year. (healthcare services, medications, missed work) From CDC Blood Pressure Facts 2015 What is Hypertension? ¨ JNC 7 (1997) definitions Stages Systolic Diastolic Prehypertension 102-129 OR 80-89 High BP Stage 1 140-159 OR 90-99 High BP Stage 2 160 or higher OR 100 or higher ¨ JNC 7 Goal BP = <140/90 ¨ JNC 8: did not define classification ¤ Patients 60 and +, start Rx when BP > 150/90* ¤ Patient < 60, start Rx when BP > 140/80 From National Heart, Lung Blood Institute SPRINT Study ¨ NIH supported study ¨ 9000+ subjects ¨ With at least one risk factor for CV disease ¨ Preliminary findings--- ¨ Adults 50 and older with HBP, targeting a SBP <120 reduced rates of CV events by 25%; reduced risk of death by 27% compared to a target of SBP 140. National Heart, Lung and Blood Institute Complex/Resistant Hypertension ¨ Resistant hypertension is defined as blood pressure that remains above goal despite concurrent use of three antihypertensive agents of different classes, one of which should be a diuretic. ¨ Patients whose blood pressure is controlled with four or more medications are considered to have resistant hypertension. Complex Hypertension ¨ BP above goal- 140/90 most patients. 130/80 diabetics or renal disease. ¨ Confirmed on at least two occasions with appropriate size cuff. ¨ Adherence to appropriate 3 drug regiment including a diuretic. -

Initial Approach to Hypertension in the Hemodynamics Unit: Review Article
REVIEW ARTICLE Initial approach to hypertension in the hemodynamics unit: review article Abordagem inicial da hipertensão arterial sistêmica em unidade de hemodinâmica: artigo de revisão Gustavo Teixeira Fulton Schimit1, José Manoel da Silva Silvestre2, Wander Eduardo Sardinha2, Eduardo Durante Ramires2, Domingos de Morais Filho2, Guilon Otávio Santos Tenório1, Fernando Barbosa Trevisan1 Abstract Correct identification and early management of hypertensive disorders should be a part of the therapeutic repertoire of every professional working in hemodynamics units. Based on recent publications, this study aims to propose a practical approach to the identification and early management of these disorders in this type of service. Keywords: hypertension; blood pressure; therapeutics; antihypertensive agents. Resumo O reconhecimento correto e manejo inicial das síndromes hipertensivas devem fazer parte do arsenal terapêutico de todo profissional que trabalhe em unidade de hemodinâmica. Este trabalho tem por objetivo, baseado em publicações recentes, propor uma abordagem prática para identificação e manejo inicial destes agravos nessa unidade. Palavras-chave: hipertensão; pressão arterial; terapêutica; anti-hipertensivos. 1Hospital Universitário Regional do Norte do Paraná, Londrina, PR, Brazil. 2Departamento de Clínica Cirúrgica, Universidade Estadual de Londrina – UEL, Londrina, PR, Brazil. Conflict of interest: No conflicts of interest declared concerning the publication of this article. Submitted on: 01.21.12. Accepted on: 03.25.13. The study was carried out at Hospital Universitário da Universidade Estadual de Londrina – UEL, Londrina, PR, Brazil. J Vasc Bras. 2013 Jun; 12(2):133-138 133 Hypertension in the hemodynamics unit INTRODUCTION been objectively adopted for the definition of normal Constant technical advances in the profession, blood pressure, and increases of 20/10 mm Hg above as well as in materials and new technologies, have this level double the risk of cardiovascular diseases11. -

3 Blood Pressure and Its Measurement
Chapter 3 / Blood Pressure and Its Measurement 49 3 Blood Pressure and Its Measurement CONTENTS PHYSIOLOGY OF BLOOD FLOW AND BLOOD PRESSURE PHYSIOLOGY OF BLOOD PRESSURE MEASUREMENT POINTS TO REMEMBER WHEN MEASURING BLOOD PRESSURE FACTORS THAT AFFECT BLOOD PRESSURE READINGS INTERPRETATION OF BLOOD PRESSURE MEASUREMENTS USE OF BLOOD PRESSURE MEASUREMENT IN SPECIAL CLINICAL SITUATIONS REFERENCES PHYSIOLOGY OF BLOOD FLOW AND BLOOD PRESSURE The purpose of the arterial system is to provide oxygenated blood to the tissues by converting the intermittent cardiac output into a continuous capillary flow and this is achieved by the structural organization of the arterial system. The blood flow in a vessel is basically determined by two factors: 1. The pressure difference between the two ends of the vessel, which provides the driving force for the flow 2. The impediment to flow, which is essentially the vascular resistance This can be expressed by the following formula: 6P Q = R where Q is the flow, 6P is the pressure difference, and R is the resistance. The pressure head in the aorta and the large arteries is provided by the pumping action of the left ventricle ejecting blood with each systole. The arterial pressure peaks in systole and tends to fall during diastole. Briefly, the peak systolic pressure achieved is determined by (see Chapter 2): 1. The momentum of ejection (the stroke volume, the velocity of ejection, which in turn are related to the contractility of the ventricle and the afterload) 2. The distensibility of the proximal arterial system 3. The timing and amplitude of the reflected pressure wave When the arterial system is stiff, as in the elderly, for the same amount of stroke output, the peak systolic pressure achieved will be higher. -

Quality Control of the Foot Revascularization Using Indocyanine Green Fluorescence Imaging
World J Surg (2017) 41:1919–1926 DOI 10.1007/s00268-017-3950-6 ORIGINAL SCIENTIFIC REPORT Quality Control of the Foot Revascularization Using Indocyanine Green Fluorescence Imaging 1 1 1 1 Nicla Settembre • Petteri Kauhanen • Anders Alba¨ck • Kristyna Spillerova • Maarit Venermo1 Published online: 6 March 2017 Ó Socie´te´ Internationale de Chirurgie 2017 Abstract Objectives Critical limb ischemia (CLI) is a clinical diagnosis, confirmed by objective tests, usually ankle-brachial index (ABI), toe pressure (TP) and TcPO2. Furthermore, the anatomical lesions in patients affected by CLI were visualized by ultrasound, angiography, CTA, or MRA. Indocyanine green fluorescence imaging (ICG-FI) is a diagnostic modality for assessing foot perfusion. We aimed to study the usefulness of ICG-FI in the quality control of revascularization. Materials and methods One hundred and four CLI limbs in 101 patients were studied with ICG-FI using SPY Elite before and after open or endovascular revascularization. ABI and TP were also measured. After ICG-FI, assessment of circulation was done using time–intensity curve derived from the two regions of interest the one being in the plantar side of the foot and the other in the dorsal side of the foot. Three parameters were derived from the curves: maximum intensity (the absolute value of the maximum intensity); intensity rate (the value from the time–intensity curve describing the increase in maximum intensity/s) and SPY10 (the intensity achieved during the first 10 s after the foot starts to gain intensity). Results Sixty-two limbs presented category 3 of Rutherford classification, 12 limbs category 4, and 30 limbs category 5. -

The Effect of Pseudoephedrine on Blood Pressure in Patients With
The Effect Of Pseudoephedrine On Blood Pressure J Am Board Fam Pract: first published as 10.3122/jabfm.4.4.201 on 1 July 1991. Downloaded from In Patients With Controlled, Uncomplicated Hypertension: A Randomized, Double-Blind, Placebo-Controlled Trial John G. Bradley, M.D., Ken]. Kallai~ Ph.D., John N. Dorsch, M.D., andJoan Fox, R.N. Abslrtlet: Pseudoephedrine is frequendy used as a decongestant. Because of concern about 1be safety of pseudoephedrine in hypertensive patients, a clinical1rial was conducted to detennine whether blood pressure control was actuallya1fected by 1bis drug in a selected group of patients with hypertension. 1Wenty-nine patients wi1b controlled, uncomplicated hypertension, who received drug therapy and ranged in age from 25 to 50 years, were randomized to a treatment or a control group. Subjects took eI1ber 60 mg of pseudoephedrine or placebo capsules four times a day for 3 days. From 0800 hours until 2200 hours each day, the subjects obtained hourly blood pressure measurements using a porlable sphygmomanometer. An analysis of variance wi1b repeated measures was calculated to determine group differences for systolic and diastoUc readings. No statistically or clinically signiftcant differences were found. 1berapeu1ic: doses of pseudoephedrine did not adversely affect control of hypertension in 1bese selected patients. 0 Am Board Fam Pract 1991; 4:201-6.) Pseudoephedrine, phenylpropanolamine, and in hypertensive patients. While no adverse effect phenylephrine are oral sympathomimetic agents was found,IO this study was uncontrolled, a com commonly used as decongestants in prescription bination of drugs was used, and patient compli and over-the-counter preparations. Long-stand ance was unverified. -

Pseudo-Hypertension in the Elderly: Still Hazy, After All These Years*
Journal of Human Hypertension (1997) 11, 621–623 1997 Stockton Press. All rights reserved 0950-9240/97 $12.00 COMMENTARY Pseudo-hypertension in the elderly: still hazy, after all these years* JD Spence Departments of Clinical Neurological Sciences Internal Medicine, and Pharmacology and Toxicology, University of Western Ontario, Canada Keywords: pseudohypertension; blood pressure measurement; elderly (*with apologies to Simon and Garfunkel) The study reported in a recent issue of the Journal of and 12 Osler-negative (OM−) patients matched for Human Hypertension by Wright and Looney1 raises age and sex, they found no significant difference important issues about the difficulty of obtaining between the two groups; the over-estimation of dias- accurate measurements of blood pressure (BP), parti- tolic pressure by the cuff was 18.4 + 15.7 in the OM+, cularly in the elderly. How common is pseudohy- and 12 + 5.8 mm Hg in the OM−. They found, as did pertension, and how can it be reliably detected short we4 and Messerli et al,2 that there was a good corre- of doing intra-arterial BP measurements? It is inter- lation between the pulse wave velocity and the mag- esting that these issues remain unresolved, after 20 nitude of cuff artifact. years. Lewis et al5 did intra-arterial pressures in 15 nor- They studied Osler’s manoeuver, the sign of cuff motensives and 21 hypertensive elderly patients artifact due to arterial stiffness described by Mes- (age 65–89; mean age was 79 for the normotensives serli et al2 and so named because Osler, in his 1892 and 76 for the hypertensive group). -

Clinical Appraisal of Arterial Stiffness: Heart: First Published As 10.1136/Hrt.2005.067025 on 9 December 2005
Heart Online First, published on December 9, 2005 as 10.1136/hrt.2005.067025 1 Clinical appraisal of arterial stiffness: Heart: first published as 10.1136/hrt.2005.067025 on 9 December 2005. Downloaded from The Argonauts in front of the Golden Fleece Charalambos Vlachopoulos, Konstantinos Aznaouridis, Christodoulos Stefanadis. 1st Department of Cardiology, University of Athens Medical School, Hippokration Hospital, Athens, Greece Wordcount: 3594 (excluding Tables, Figure legends and References) http://heart.bmj.com/ Keywords: arterial stiffness, wave reflection, arterial elastic properties, aorta, peripheral vessels on September 25, 2021 by guest. Protected copyright. Corresponding author: Christodoulos Stefanadis 9 Tepeleniou Str. Paleo Psychico, 154 52 Athens, Greece Tel: + 30 210 770 3052 Fax: + 30 210 748 5039 e-mail: [email protected] Copyright Article author (or their employer) 2005. Produced by BMJ Publishing Group Ltd (& BCS) under licence. 2 The interest for evaluation of arterial elastic properties is growing during recent years Heart: first published as 10.1136/hrt.2005.067025 on 9 December 2005. Downloaded from impressively and in parallel with the widespread availability of noninvasive methods for assessment of arterial stiffness. In this article we discuss the current evidence concerning the clinical value of estimating arterial stiffness (mainly of large, elastic-type arteries, such as the aorta and the carotids) in the contemporary era of cardiovascular (CV) medicine. In this context, one has to keep in mind that the clinical -

ACCF/AHA 2011 Expert Consensus Document on Hypertension in The
Journal of the American College of Cardiology Vol. 57, No. 20, 2011 © 2011 by the American College of Cardiology Foundation and the American Heart Association, Inc. ISSN 0735-1097/$36.00 Published by Elsevier Inc. doi:10.1016/j.jacc.2011.01.008 EXPERT CONSENSUS DOCUMENT ACCF/AHA 2011 Expert Consensus Document on Hypertension in the Elderly A Report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents Developed in Collaboration With the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension Writing Wilbert S. Aronow, MD, FACC, Co-Chair* Eduardo Ortiz, MD, MPH† Committee Jerome L. Fleg, MD, FACC, Co-Chair† Efrain Reisin, MD, FASN** Members Carl J. Pepine, MD, MACC, Co-Chair* Michael W. Rich, MD, FACC†† Douglas D. Schocken, MD, FACC, FAHA‡‡ Nancy T. Artinian, PHD, RN, FAHA‡ Michael A. Weber, MD, FACC§§ ʈʈ George Bakris, MD, FASN Deborah J. Wesley, RN, BSN Alan S. Brown, MD, FACC, FAHA‡ *American College of Cardiology Foundation Representative; †Na- Keith C. Ferdinand, MD, FACC§ tional Heart, Lung, and Blood Institute; ‡American Heart Association ʈ Representative; §Association of Black Cardiologists Representative; Mary Ann Forciea, MD, FACP ʈAmerican College of Physicians Representative; ¶American Academy William H. Frishman, MD, FACC* of Neurology Representative; #European Society of Hypertension Representative; **American Society of Nephrology Representative; Cheryl Jaigobin, MD¶ ††American Geriatrics Society Representative; ‡‡American Society for Preventive Cardiology Representative; §§American Society of Hyper- John B. Kostis, MD, FACC tension Representative; ʈʈACCF Task Force on Clinical Expert Con- Giuseppi Mancia, MD# sensus Documents Representative. -

Out-Of-Clinic Blood Pressure Testing in Primary Care
Out-of-clinic blood pressure testing in primary care Out-of-clinic blood pressure monitoring is KEY practice points: increasingly regarded as a routine component of cardiovascular risk management. This is because it Out-of-clinic blood pressure measurements more accurately reflect a patient’s true blood pressure than do is a better predictor of cardiovascular events and clinic-based measurements and improve the quality of mortality than clinic-based measurements. General shared management decisions practices that use this technique can provide Consider out-of-clinic blood pressure testing to “rule-out” patients with more accurate cardiovascular risk the possibility of white-coat hypertension before initiating assessments and help them to make better decisions antihypertensive treatment about their health. Prescribers are also able to Out-of-clinic blood pressure testing can be used to more titrate blood pressure treatment regimens more accurately guide management once antihypertensive accurately using out-of-clinic measurements than treatment has been initiated if management was guided solely by clinic-based Consider out-of-clinic blood pressure testing for patients blood pressure assessments. Only validated devices with low cardiovascular risk, e.g. younger patients, where are recommended for the measurement of blood there is a clinical suspicion of masked hypertension pressure. Out-of-clinic blood pressure testing includes 24-hour ambulatory testing, where the patient wears an automated device, as well as home-based measurements performed by the patient. Ambulatory blood pressure monitoring is available as an outpatient test by DHBs, privately by some cardiologists or devices may be purchased by general practices. Home blood pressure testing devices are relatively inexpensive and validated devices can be purchased by patients or practices. -
Shock, Resuscitation, and Surgical Critical Care
SHOCK, RESUSCITATION, AND SURGICAL CRITICAL CARE PART A: SHOCK AND RESUSCITATION COMPETENCY-BASED KNOWLEDGE OBJECTIVES: 1. Define shock, categorize it based upon type, explain the etiology and pathophysiology of each type of shock: a. Cardiogenic b. Hypovolemic c. Distributive (septic, anaphylactic, neurogenic, and adrenal insufficiency mediated) d. Obstructive (cardiac tamponade, tension pneumothorax, pulmonary embolus) 2. Summarize the clinical presentation and hemodynamic parameters associated with each type of shock using clinical terms, such as heart rate, respiratory rate, and blood pressure and filling pressures. 3. Propose an algorithm for diagnosing and initiating treatment for each shock type. a. Cardiogenic b. Hypovolemic c. Distributive (septic, anaphylactic, neurogenic, and adrenal insufficiency mediated) d. Obstructive (cardiac tamponade, tension pneumothorax, pulmonary embolus) 4. Discuss the pathophysiology, including the mechanism of arrest, for each of the following situations: a. Acute myocardial infarction b. Acute dysrhythmia c. Congestive heart failure d. Hypovolemic shock (blood loss, dehydration) e. Burns f. Hemorrhagic shock (non-traumatic) g. Septic shock h. Anaphylactic shock (envenomation, drug related) i. Acute adrenal insufficiency j. Penetrating or blunt trauma (1) Tension pneumothorax (2) Pericardial tamponade (3) Hemorrhagic shock k. Hypothermia l. Substance abuse m. Electrical injury n. Suffocation o. Acute stroke 5. Explain the indications for and the pharmacokinetics of each of the following drugs: a. Lidocaine j. Vasopressin b. Digoxin k. Nitroglycerin c. Metoprolol l. Amrinone d. Diltiazem m. Milrinone e. Pronestyl n. Levophed f. Amiodarone o. Phenylephrine g. Dopamine p. Epinephrine h. Dobutamine i. Adenosine(Adenocard®) 6. Summarize the indication and appropriate technique for cardiac support, pressors, and Circulatory Assist Devices (IABP, LVAD, RVAD).