Complex Hypertension
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypertension – Adult – Clinical Practice Guideline
Hypertension – Adult – Clinical Practice Guideline Table of Contents EXECUTIVE SUMMARY ........................................................................................................... 3 SCOPE ...................................................................................................................................... 4 METHODOLOGY ...................................................................................................................... 5 INTRODUCTION ....................................................................................................................... 5 RECOMMENDATIONS .............................................................................................................. 5 Establish the Diagnosis ........................................................................................... 5 Patient Evaluation ................................................................................................... 7 Treatment Goals ..................................................................................................... 7 Lifestyle Modifications ............................................................................................. 8 Table 4 – Lifestyle Modifications ........................................................................ 9 Medication Treatment............................................................................................ 11 Figure 1 - Initiation and Titration of Antihypertensive Medication ..................... 13 Table 7 - Antihypertensive -

Evidence Synthesis Number 197 Screening for Hypertension in Adults
Evidence Synthesis Number 197 Screening for Hypertension in Adults: A Systematic Evidence Review for the U.S. Preventive Services Task Force Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov Contract No. HHSA-290-2015-000017-I-EPC5, Task Order No. 5 Prepared by: Kaiser Permanente Research Affiliates Evidence-based Practice Center Kaiser Permanente Center for Health Research Portland, OR Investigators: Janelle M. Guirguis-Blake, MD Corinne V. Evans, MPP Elizabeth M. Webber, MS Erin L. Coppola, MPH Leslie A. Perdue, MPH Meghan Soulsby Weyrich, MPH AHRQ Publication No. 20-05265-EF-1 June 2020 This report is based on research conducted by the Kaiser Permanente Research Affiliates Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. HHSA-290-2015-000017-I-EPC5, Task Order No. 5). The findings and conclusions in this document are those of the authors, and do not necessarily represent the views of AHRQ. Therefore, no statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help health care decision makers—patients and clinicians, health system leaders, and policymakers, among others—make well-informed decisions and thereby improve the quality of health care services. This report is not intended to be a substitute for the application of clinical judgment. Anyone who makes decisions concerning the provision of clinical care should consider this report in the same way as any medical reference and in conjunction with all other pertinent information (i.e., in the context of available resources and circumstances presented by individual patients). -
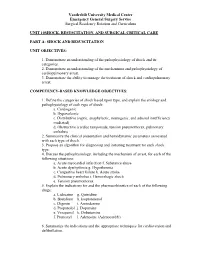
Unit 10 Shock,Resuscitation Part A
Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum UNIT 10SHOCK, RESUSCITATION, AND SURGICAL CRITICAL CARE PART A: SHOCK AND RESUSCITATION UNIT OBJECTIVES: 1. Demonstrate an understanding of the pathophysiology of shock and its categories. 2. Demonstrate an understanding of the mechanisms and pathophysiology of cardiopulmonary arrest. 3. Demonstrate the ability to manage the treatment of shock and cardiopulmonary arrest. COMPETENCY-BASED KNOWLEDGE OBJECTIVES: 1. Define the categories of shock based upon type, and explain the etiology and pathophysiology of each type of shock: a. Cardiogenic b. Hypovolemic c. Distributive (septic, anaphylactic, neurogenic, and adrenal insufficiency mediated) d. Obstructive (cardiac tamponade, tension pneumothorax, pulmonary embolus) 2. Summarize the clinical presentation and hemodynamic parameters associated with each type of shock. 3. Propose an algorithm for diagnosing and initiating treatment for each shock type. 4. Discuss the pathophysiology, including the mechanism of arrest, for each of the following situations: a. Acute myocardial infarction f. Substance abuse b. Acute dysrhythmia g. Hypothermia c. Congestive heart failure h. Acute stroke d. Pulmonary embolus i. Hemorrhagic shock e. Tension pneumothorax 5. Explain the indications for and the pharmacokinetics of each of the following drugs: a. Lidocaine g. Quinidine b. Bretylium h. Isoproterenol c. Digoxin i. Amiodarone d. Propanolol j. Dopamine e. Verapamil k. Dobutamine f. Pronestyl l. Adenosine (Adenocard®) 6. Summarize the indications and the appropriate techniques for cardioversion and defibrillation. Vanderbilt University Medical Center Emergency General Surgery Service Surgical Residency Rotation and Curriculum 7. Outline the signs and symptoms of acute airway obstruction and define the appropriate intervention in adult and pediatric patients. -

Blood Pressure Training Curriculum for the Dental Team
Blood Pressure Training Curriculum for the Dental Team 2018 Blood Pressure Training Curriculum for the Dental Team TABLE OF CONTENTS Learning Objectives 1 Hypertension: An Introduction 1 Hypertension: Implications for the Dental Team 4 Recording Blood Pressure 7 Special Case Scenarios 9 Close the Loop: Refer to the Primary Care Physician 10 Appendix A: List of anti-hypertensive medications 11 Appendix B: Template referral form to primary care provider 13 LEARNING OBJECTIVES At the end of this training, the participant should: • Understand the basics of hypertension. • Identify various categories of hypertension. • Understand the appropriate technique of recording blood pressure. • Recognize the need to measure blood pressure for every new patient, and at least annually on follow-up visits. • Recognize the need to refer a patient with hypertension to a primary care provider. Hypertension: An Introduction What is blood pressure? Blood pressure is the force of blood pushing against the walls of the arteries that carry blood from the heart to other parts of the body. Blood pressure normally rises and falls throughout the day based on an individual’s activity. High blood pressure, also known as hypertension (HTN), is a disease that occurs when blood pressure stays above normal for a long time. As a result, the walls of arteries get stretched beyond their healthy limit and damage occurs creating a variety of other health problems.1 What is the burden of hypertension?2 • Hypertension is the 13th leading cause of death in the United States. • In North Carolina in 2015, hypertension was the primary cause of 942 deaths (about 1% of all deaths) and a contributing cause to 23,495 heart disease and stroke deaths. -

Thirty-Minute Office Blood Pressure Monitoring in Primary Care
Thirty-Minute Office Blood Pressure Monitoring in Primary Care Michiel J. Bos, MD, PhD ABSTRACT Sylvia Buis, MD, MPH PURPOSE Automated office blood pressure monitoring during 30 minutes Gezondheidscentrum Ommoord, Rotter- (OBP30) may reduce overtreatment of patients with white-coat hypertension dam, the Netherlands in primary health care. OBP30 results approximate those of ambulatory blood pressure monitoring, but OBP30 is much more convenient. In this study, we compared OBP30 with routine office blood pressure (OBP) readings for different indications in primary care and evaluated how OBP30 influenced the medication prescribing of family physicians. METHODS All consecutive patients who underwent OBP30 for medical reasons over a 6-month period in a single primary health care center in the Netherlands were enrolled. We compared patients’ OBP30 results with their last preceding routine OBP reading, and we asked their physicians why they ordered OBP30, how they treated their patients, and how they would have treated their patients without it. RESULTS We enrolled 201 patients (mean age 68.6 years, 56.7% women). The mean systolic OBP30 was 22.8 mm Hg lower than the mean systolic OBP (95% CI, 19.8-26.1 mm Hg). The mean diastolic OBP30 was 11.6 mm Hg lower than the mean diastolic OBP (95% CI, 10.2-13.1 mm Hg). Considerable differences between OBP and OBP30 existed in patients with and without suspected white- coat hypertension, and differences were larger in individuals aged 70 years or older. Based on OBP alone, physicians said they would have started or intensified medication therapy in 79.1% of the studied cases (95% CI, 73.6%-84.6%). -

Effects of White-Coat Hypertension on Heart Rate Recovery and Blood Pressure Response During Exercise Test
Kosin Medical Journal 2020;35:89-100. https://doi.org/10.7180/kmj.2020.35.2.89 Effects of White-coat Hypertension on Heart Rate Recovery and Blood Pressure Response during Exercise Test Sol Jin 1, Jung Ho Heo 2, Bong Jun Kim 2 1Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea 2Department of Cardiology, Kosin University College of Medicine, Busan, Korea Objectives : White-coat hypertension is defined as high blood pressure (BP) on clinical assessment but normal BP elsewhere or on ambulatory measurement. Autonomic dysfunction may be one of the mechanisms causing white-coat hypertension. Slowed heart rate recovery and excessive BP response during exercise test are associated with autonomic dysfunction. The purpose of this study was to determine the association between white-coat hypertension and abnormal autonomic nervous system response. Methods : We assessed 295 patients stratified into three groups via 24hr ambulatory BP monitoring, following 2017 ACC/AHA guidelines : normal BP group, white-coat hypertension group, and a hypertension group. We analyzed medical history, blood test, echocardiography, 24hr ambulatory BP monitoring, and exercise test data. Results : There was no difference in basement characteristics and echocardiography among the groups. Blunted heart rate recovery of each group showed a significant difference. Control group had 0% blunted heart rate recovery, but 33.3% in white coat group and 27.6% in true hypertension group ( P < 0.001). Also, in the control group, 4.5% showed excessive BP response, but 31.5% in the white coat hypertension group and 29.3% in the true hypertension group ( P < 0.001). -

White Coat Hypertension and Target Organ Involvement: the Impact of Different Cut-Off Levels on Albuminuria and Left Ventricular Mass and Geometry
Journal of Human Hypertension (1998) 12, 433–439 1998 Stockton Press. All rights reserved 0950-9240/98 $12.00 http://www.stockton-press.co.uk/jhh ORIGINAL ARTICLE White coat hypertension and target organ involvement: the impact of different cut-off levels on albuminuria and left ventricular mass and geometry AHøegholm, KS Kristensen, LE Bang and JW Nielsen Department of Internal Medicine, County Central Hospital, N{stved, Denmark The aim of this cross-sectional study which took place atory daytime BP of 135.6/90.4 mm Hg was found to cor- in a hypertension clinic at a district general hospital in respond to an office BP of 140/90 mm Hg in normal con- Denmark was to make a pragmatic definition of white trols; used as a cut-off level in patients with newly coat hypertension. A total of 420 patients were referred diagnosed hypertension it separated 19% as white coat consecutively from general practice with newly diag- hypertensives. The end-organ involvement of these nosed untreated essential hypertension and 146 normal white coat hypertensives differed significantly from subjects were drawn at random from the Danish those with established hypertension but not from the national register. The following measurements were normal controls. Lower cut-off levels were less efficient taken: office blood pressure; 24-h ambulatory blood in this respect, as was the case when the systolic BP pressure (BP) monitoring; echocardiography with deter- was not taken into account. mination of left ventricular mass index and relative wall In conclusion a pragmatic definition of white coat thickness; and early morning urine albumin/creatinine hypertension should—apart from well-established ratios. -

White Coat Hypertension in Children And
ISSN: 2474-3690 Çakıcı et al. J Hypertens Manag 2019, 5:043 DOI: 10.23937/2474-3690/1510043 Volume 5 | Issue 2 Journal of Open Access Hypertension and Management REsEaRch aRTiclE White Coat Hypertension in Children and Adolescents: Innocent or Not? Evrim Kargın Çakıcı*, Eda Didem Kurt Şükür, Fatma Yazılıtaş, Gökçe Gür, Tülin Güngör, Evra Çelikkaya, Deniz Karakaya and Mehmet Bülbül Department of Pediatric Nephrology and Rheumatology, Dr. Sami Ulus Maternity and Child Health and Check for Diseases Training and Research Hospital, Ankara, Turkey updates *Corresponding author: Evrim Kargin Cakici, MD, Department of Pediatric Nephrology and Rheumatology, Dr. Sami Ulus Maternity and Child Health and Diseases Training and Research Hospital, Ankara, Turkey, GSM: 00905052653472 Abstract Introduction Background: The clinical significance of white coat hyper- After the advent of ambulatory blood pressure tension is still uncertain. We aimed to evaluate children with monitoring (ABPM) the management of blood pres- white coat hypertension regarding their clinical, laboratory sure (BP) has dramatically changed [1,2]. Ambulatory characteristics, evidence of target organ damage and com- pare them to normotensive and hypertensive children. blood pressure monitoring provides a more accurate measurement of BP than auscultatory or automated Methods: Fourty patients diagnosed with white coat hy- office readings and it is shown to be superior in ad- pertension, 40 patients with primary hypertension and 40 normotensive children of similar age, gender and body ministration or adjustion of antihypertensive treat- mass index were included in the study. Ambulatory blood ment and prediction of cardiovascular morbidity. An- pressure monitoring and echocardiographic examination other superiority of ABPM is the detection of white were performed to all children. -

Initial Approach to Hypertension in the Hemodynamics Unit: Review Article
REVIEW ARTICLE Initial approach to hypertension in the hemodynamics unit: review article Abordagem inicial da hipertensão arterial sistêmica em unidade de hemodinâmica: artigo de revisão Gustavo Teixeira Fulton Schimit1, José Manoel da Silva Silvestre2, Wander Eduardo Sardinha2, Eduardo Durante Ramires2, Domingos de Morais Filho2, Guilon Otávio Santos Tenório1, Fernando Barbosa Trevisan1 Abstract Correct identification and early management of hypertensive disorders should be a part of the therapeutic repertoire of every professional working in hemodynamics units. Based on recent publications, this study aims to propose a practical approach to the identification and early management of these disorders in this type of service. Keywords: hypertension; blood pressure; therapeutics; antihypertensive agents. Resumo O reconhecimento correto e manejo inicial das síndromes hipertensivas devem fazer parte do arsenal terapêutico de todo profissional que trabalhe em unidade de hemodinâmica. Este trabalho tem por objetivo, baseado em publicações recentes, propor uma abordagem prática para identificação e manejo inicial destes agravos nessa unidade. Palavras-chave: hipertensão; pressão arterial; terapêutica; anti-hipertensivos. 1Hospital Universitário Regional do Norte do Paraná, Londrina, PR, Brazil. 2Departamento de Clínica Cirúrgica, Universidade Estadual de Londrina – UEL, Londrina, PR, Brazil. Conflict of interest: No conflicts of interest declared concerning the publication of this article. Submitted on: 01.21.12. Accepted on: 03.25.13. The study was carried out at Hospital Universitário da Universidade Estadual de Londrina – UEL, Londrina, PR, Brazil. J Vasc Bras. 2013 Jun; 12(2):133-138 133 Hypertension in the hemodynamics unit INTRODUCTION been objectively adopted for the definition of normal Constant technical advances in the profession, blood pressure, and increases of 20/10 mm Hg above as well as in materials and new technologies, have this level double the risk of cardiovascular diseases11. -

A Meta-Analysis
Masked Hypertension and White-Coat Hypertension in Chronic Kidney Disease: A Meta-analysis Farhan Bangash* and Rajiv Agarwal*† *Department of Medicine, Indiana University School of Medicine and †Department of Medicine, Richard L. Roudebush VA Medical Center, Indianapolis, Indiana Background and objectives: Poor hypertension control observed in patients with chronic kidney disease (CKD) may in part be due to the suboptimal assessment of BP with clinic BP measurements alone. The goal of this meta-analysis was to estimate the prevalence and determinants of white-coat and masked hypertension in the adult CKD population. Design, setting, participants, & measurements: Articles reporting prevalence of masked and white-coat hypertension in patients with CKD were obtained from two major databases. We then performed a meta-analysis to derive pooled estimates of prevalence and determinants of these two conditions. Results: Among 980 patients with CKD identified in six studies, the overall prevalence of masked hypertension was 8.3% and of white-coat hypertension was 18.3%. More alarming, 40.4% of patients who had CKD and were thought to have normotension (or adequately treated hypertension) in fact had hypertension at home. Also 30.0% of patients who had CKD and were thought to have hypertension had normotension at home. The thresholds for classification of clinic and ambulatory BP as hypertensive strongly influenced the risk for diagnosis of masked hypertension in favor of white-coat hypertension. Conclusions: Because clinic BP measurements alone lead to substantial misclassification in BP, we estimate that the prevalence of poorly controlled hypertension is likely less than currently estimated. Out-of-office BP monitoring may improve the management of hypertension in patients with CKD. -

3 Blood Pressure and Its Measurement
Chapter 3 / Blood Pressure and Its Measurement 49 3 Blood Pressure and Its Measurement CONTENTS PHYSIOLOGY OF BLOOD FLOW AND BLOOD PRESSURE PHYSIOLOGY OF BLOOD PRESSURE MEASUREMENT POINTS TO REMEMBER WHEN MEASURING BLOOD PRESSURE FACTORS THAT AFFECT BLOOD PRESSURE READINGS INTERPRETATION OF BLOOD PRESSURE MEASUREMENTS USE OF BLOOD PRESSURE MEASUREMENT IN SPECIAL CLINICAL SITUATIONS REFERENCES PHYSIOLOGY OF BLOOD FLOW AND BLOOD PRESSURE The purpose of the arterial system is to provide oxygenated blood to the tissues by converting the intermittent cardiac output into a continuous capillary flow and this is achieved by the structural organization of the arterial system. The blood flow in a vessel is basically determined by two factors: 1. The pressure difference between the two ends of the vessel, which provides the driving force for the flow 2. The impediment to flow, which is essentially the vascular resistance This can be expressed by the following formula: 6P Q = R where Q is the flow, 6P is the pressure difference, and R is the resistance. The pressure head in the aorta and the large arteries is provided by the pumping action of the left ventricle ejecting blood with each systole. The arterial pressure peaks in systole and tends to fall during diastole. Briefly, the peak systolic pressure achieved is determined by (see Chapter 2): 1. The momentum of ejection (the stroke volume, the velocity of ejection, which in turn are related to the contractility of the ventricle and the afterload) 2. The distensibility of the proximal arterial system 3. The timing and amplitude of the reflected pressure wave When the arterial system is stiff, as in the elderly, for the same amount of stroke output, the peak systolic pressure achieved will be higher. -

Quality Control of the Foot Revascularization Using Indocyanine Green Fluorescence Imaging
World J Surg (2017) 41:1919–1926 DOI 10.1007/s00268-017-3950-6 ORIGINAL SCIENTIFIC REPORT Quality Control of the Foot Revascularization Using Indocyanine Green Fluorescence Imaging 1 1 1 1 Nicla Settembre • Petteri Kauhanen • Anders Alba¨ck • Kristyna Spillerova • Maarit Venermo1 Published online: 6 March 2017 Ó Socie´te´ Internationale de Chirurgie 2017 Abstract Objectives Critical limb ischemia (CLI) is a clinical diagnosis, confirmed by objective tests, usually ankle-brachial index (ABI), toe pressure (TP) and TcPO2. Furthermore, the anatomical lesions in patients affected by CLI were visualized by ultrasound, angiography, CTA, or MRA. Indocyanine green fluorescence imaging (ICG-FI) is a diagnostic modality for assessing foot perfusion. We aimed to study the usefulness of ICG-FI in the quality control of revascularization. Materials and methods One hundred and four CLI limbs in 101 patients were studied with ICG-FI using SPY Elite before and after open or endovascular revascularization. ABI and TP were also measured. After ICG-FI, assessment of circulation was done using time–intensity curve derived from the two regions of interest the one being in the plantar side of the foot and the other in the dorsal side of the foot. Three parameters were derived from the curves: maximum intensity (the absolute value of the maximum intensity); intensity rate (the value from the time–intensity curve describing the increase in maximum intensity/s) and SPY10 (the intensity achieved during the first 10 s after the foot starts to gain intensity). Results Sixty-two limbs presented category 3 of Rutherford classification, 12 limbs category 4, and 30 limbs category 5.