World Class Endocrine Surgeons Gastrointestinal & Minimally Invasive Surgery Newsletter
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Code Procedure Description Adrenalectomy 60540 Adrenalectomy, Partial Or Complete, Or Exploration of Adrenal Gland with Or Witho
BCBSM Approved POP Procedures Code Procedure Description Adrenalectomy Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal 60540 (separate procedure) 60545 Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal (separate procedure); with excision of adjacent retroperitoneal tumor Laparoscopy, surgical, with adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, 60650 transabdominal, lumbar or dorsal Appendectomy 44955 Appendectomy; when done for indicated purpose at time of other major procedure (not as separate procedure) 44960 Appendectomy; for ruptured appendix with abscess or generalized peritonitis 44970 Laparoscopy, surgical, appendectomy Carotid Endarterectomy (CEA) 35301 Thromboendarterectomy, including patch graft, if performed; carotid, vertebral, subclavian, by neck incision Carpal Tunnel 29848 Endoscopy, wrist, surgical, with release of transverse carpal ligament 64721 Neuroplasty and/or transposition; median nerve at carpal tunnel Cesarean Delivery (Cesarean Section) Ligation or transection of fallopian tube(s) when done at the time of cesarean delivery or intra-abdominal surgery (not a separate 58611 procedure) (List separately in addition to code for primary procedure) 59510 Routine obstetric care including antepartum care, cesarean delivery, and postpartum care 59514 Cesarean delivery only 59515 Cesarean delivery only; including postpartum care -

Adrenalectomy Patient Information Leaflet
Adrenalectomy Patient information leaflet UHB is a no smoking Trust To see all of our current patient information leaflets please visit www.uhb.nhs.uk/patient-information-leaflets.htm What is an adrenalectomy? An adrenalectomy (ad-renal-ect-omy) is an operation to remove one or both of the adrenal glands. The adrenal glands sit above the kidneys. Right Left adrenal adrenal gland gland Kidney Kidney The main role of the adrenal glands is to release hormones into the body. The main hormones released are stress related hormones (cortisol, noradrenaline and adrenaline), hormones that regulate metabolism, hormones that affect immune system function, androgens (sex hormones) and hormones for saltwater balance (aldosterone). 2 | PI18/1289/03 Adrenalectomy An adrenalectomy can be done: • ‘Open’ with one large surgical cut below the ribcage • Or ‘laparoscopic’ which involves four smaller cuts being made allowing the inside of the abdomen to be seen using a camera Some laparoscopic operations may have be converted to ‘open’ at the time of the surgery due to the surgeon not being able to see the inside of the abdomen clearly enough (about 5% of cases). The surgery is performed under general anaesthetic so you will be asleep and will not feel any pain. The surgery normally takes 1–2 hours. The adrenal gland(s) will be sent to a pathologist after it is removed for further tests in a laboratory using a microscope. Why is an adrenalectomy performed? The adrenal gland(s) need to be removed if there is a mass/ tumour in the gland(s). An adrenalectomy is performed if: 1. -

Advances in Risk-Oriented Surgery for Multiple Endocrine Neoplasia Type 2
25 2 Endocrine-Related A Machens et al. Advances in risk-oriented 25:2 T41–T52 Cancer surgery for MEN2 THEMATIC REVIEW Advances in risk-oriented surgery for multiple endocrine neoplasia type 2 Andreas Machens1 and Henning Dralle2 1Department of General, Visceral and Vascular Surgery, Martin Luther University Halle-Wittenberg, Halle, Saale, Germany 2Department of General, Visceral and Transplantation Surgery, Section of Endocrine Surgery, University of Duisburg-Essen, Essen, Germany Correspondence should be addressed to A Machens: [email protected] This paper is part of a thematic review section on 25 Years of RET and MEN2. The guest editors for this section were Lois Mulligan and Frank Weber. Abstract Genetic association studies hinge on definite clinical case definitions of the disease of Key Words interest. This is why more penetrant mutations were overrepresented in early multiple f biochemical screening endocrine neoplasia type 2 (MEN2) studies, whereas less penetrant mutations went f DNA-based screening underrepresented. Enrichment of genetic association studies with advanced disease f RET proto-oncogene may produce a flawed understanding of disease evolution, precipitating far-reaching f gene test surgical strategies like bilateral total adrenalectomy and 4-gland parathyroidectomy in f gene carrier MEN2. The insight into the natural course of the disease gleaned over the past 25 years f multiple endocrine caused a paradigm shift in MEN2: from the removal of target organs at the expense of neoplasia type 2A greater operative -

Use of Dexmedetomidine in a Parturient with Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy
PRACTICE CASE REPORT Use of Dexmedetomidine in a Parturient With Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy: A Case Report Amanda L. Faulkner, MD, Eric Swanson, MD, Thomas L. McLarney, MD, Cortney Y. Lee, MD, and Annette Rebel, MD * * * † * 08/15/2018 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3yRlXg5VZA8uqNuqWFo8dRhJiNZRTFLkCeIa0nEMHM2KbYm37VRaE3A== by https://journals.lww.com/aacr from Downloaded Dexmedetomidine is a selective α2-agonist, frequently used in perioperative medicine as anes- thesia adjunct. The medication carries a Food and Drug Administration pregnancy category C Downloaded designation and is therefore rarely used for parturients undergoing nonobstetric surgery. We are reporting the use of dexmedetomidine in the anesthetic management of a parturient undergoing minimally invasive unilateral adrenalectomy for pheochromocytoma during the second trimester from https://journals.lww.com/aacr of pregnancy. Additionally, because of the multiple endocrine neoplasia type 2A constellation with diagnosis of medullary thyroid cancer, the patient underwent a total thyroidectomy 1 week after the adrenalectomy. (A&A Practice. XXX;XXX:00–00.) exmedetomidine is a selective α2-agonist, fre- CASE REPORT by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3yRlXg5VZA8uqNuqWFo8dRhJiNZRTFLkCeIa0nEMHM2KbYm37VRaE3A== quently used in perioperative medicine. It has A 34-year-old gravida 3 para 2 woman (body weight, 61 Dfound favor in this setting because of its sedative kg; -

Surgical Indications and Techniques for Adrenalectomy Review
THE MEDICAL BULLETIN OF SISLI ETFAL HOSPITAL DOI: 10.14744/SEMB.2019.05578 Med Bull Sisli Etfal Hosp 2020;54(1):8–22 Review Surgical Indications and Techniques for Adrenalectomy Mehmet Uludağ,1 Nurcihan Aygün,1 Adnan İşgör2 1Department of General Surgery, Sisli Hamidiye Etfal Training and Research Hospital, Istanbul, Turkey 2Department of General Surgery, Bahcesehir University Faculty of Medicine, Istanbul, Turkey Abstract Indications for adrenalectomy are malignancy suspicion or malignant tumors, non-functional tumors with the risk of malignancy and functional adrenal tumors. Regardless of the size of functional tumors, they have surgical indications. The hormone-secreting adrenal tumors in which adrenalectomy is indicated are as follows: Cushing’s syndrome, arises from hypersecretion of glucocorticoids produced in fasciculata adrenal cortex, Conn’s syndrome, arises from an hypersecretion of aldosterone produced by glomerulosa adrenal cortex, and Pheochromocytomas that arise from adrenal medulla and produce catecholamines. Sometimes, bilateral adre- nalectomy may be required in Cushing's disease due to pituitary or ectopic ACTH secretion. Adenomas arise from the reticularis layer of the adrenal cortex, which rarely releases too much adrenal androgen and estrogen, may also develop and have an indication for adrenalectomy. Adrenal surgery can be performed by laparoscopic or open technique. Today, laparoscopic adrenalectomy is the gold standard treatment in selected patients. Laparoscopic adrenalectomy can be performed transperitoneally or retroperitoneoscopi- cally. Both approaches have their advantages and disadvantages. In the selection of the surgery type, the experience and habits of the surgeon are also important, along with the patient’s characteristics. The most common type of surgery performed in the world is laparoscopic transabdominal lateral adrenalectomy, which most surgeons are more familiar with. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

What's New in End Ocrine Surgery?
What’s new in endocrine surgery? Endocrine surgery has become a well-defined part of general surgery. EUGENIO PANIERI, FCS(SA) Head, Oncology Endocrine Surgery, Department of Surgery, University of Cape Town Eugenio Panieri is a graduate of the University of Cape Town, and is Head of the Endocrine and Surgical Oncology Unit at Groote Schuur Hospital. His main areas of interest are in minimally access surgery for endocrine conditions, and the use of sentinel lymph node biopsy and immediate reconstruction in breast cancer. Endocrine surgery has steadily evolved from relative obscurity into a well-defined subdiscipline of general surgery. Success in this area relies on close co-operation with endocrinologists, radiologists, nuclear physicians, and pathologists. Endocrine surgeons have a pivotal role in the management of nodular thyroid disease and thyroid cancer, hyperparathyroidism, as well as functional adrenal and pancreatic tumours. Unlike other solid tumours, endocrine neoplasms make their presence known by systemic effects of excess hormone production, rather than by local symptoms related to tumour size or local invasion. As laboratory diagnostic methods and radiology imaging techniques have improved, so the demand for surgical expertise in this area has increased. Techniques of minimally invasive surgery have transformed the practice of general surgery. In some cases, such as cholecystectomy or anti-reflux surgery, laparoscopy has become the unquestioned standard of care; in others, such as hernia or colorectal surgery the debate continues. In this article I will describe the role such Fig. 1. CT scan of the abdomen illustrating a 7 cm phaeochromocytoma techniques have to play in the surgical management of endocrine in the left adrenal gland. -
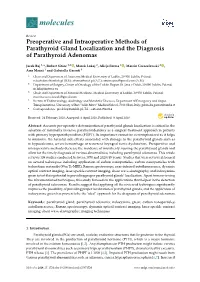
Preoperative and Intraoperative Methods of Parathyroid Gland Localization and the Diagnosis of Parathyroid Adenomas
molecules Review Preoperative and Intraoperative Methods of Parathyroid Gland Localization and the Diagnosis of Parathyroid Adenomas Jacek Baj 1,*, Robert Sitarz 1,2 , Marek Łokaj 2, Alicja Forma 1 , Marcin Czeczelewski 3 , Amr Maani 1 and Gabriella Garruti 4 1 Chair and Department of Anatomy, Medical University of Lublin, 20-950 Lublin, Poland; [email protected] (R.S.); [email protected] (A.F.); [email protected] (A.M.) 2 Department of Surgery, Center of Oncology of the Lublin Region St. Jana z Dukli, 20-090 Lublin, Poland; [email protected] 3 Chair and Department of Forensic Medicine, Medical University of Lublin, 20-950 Lublin, Poland; [email protected] 4 Section of Endocrinology, Andrology and Metabolic Diseases, Department of Emergency and Organ Transplantations, University of Bari “Aldo Moro” Medical School, 70124 Bari, Italy; [email protected] * Correspondence: [email protected]; Tel.: +48-662-094-014 Received: 24 February 2020; Accepted: 8 April 2020; Published: 9 April 2020 Abstract: Accurate pre-operative determination of parathyroid glands localization is critical in the selection of minimally invasive parathyroidectomy as a surgical treatment approach in patients with primary hyperparathyroidism (PHPT). Its importance cannot be overemphasized as it helps to minimize the harmful side effects associated with damage to the parathyroid glands such as in hypocalcemia, severe hemorrhage or recurrent laryngeal nerve dysfunction. Preoperative and intraoperative methods decrease the incidence of mistakenly -

Laparoscopic Adrenalectomy
Laparoscopic Adrenalectomy What is a laparoscopic Adrenalectomy The term laparoscopic adrenalectomy means removal of an adrenal gland using the ‘keyhole’ (laparoscopic) surgical method. The laparoscopic method of adrenal gland removal involves using three or four one centimetre cuts (incisions). A thin tube with a light and camera on the end (a laparoscope), and surgical instruments can then be passed through these incisions. The camera sends pictures to a TV screen so that the surgeon can see the adrenal gland and surrounding organs. One of the incisions (cuts) will be enlarged to enable the gland to be removed once it has been disconnected from the surrounding tissues and blood vessels. A laparoscopic adrenalectomy is performed under a general anaesthetic. You will meet the anaesthetist on the day of your operation and he or she will discuss the anaesthetic and pain relief with you. You should expect to stay in hospital from 2 to 4 nights depending on the reason for the operation. The laparoscopic, and most commonly used, method of adrenal gland removal has been shown to cause less blood loss, less pain and fewer complications than the open method, and also a much shorter recovery time. The open method is now only used in more complex cases. Open surgery to remove an adrenal gland involves making a large cut on the side with unavoidable problems such as more intense pain which makes moving around more difficult, a hospital stay of 7 to 10 days, and a prolonged time off work. Your Urology consultant will discuss with you in detail which approach is appropriate for you. -

(CCSR) for ICD-10-PCS PROCEDURES, V2021.1
USER GUIDE: CLINICAL CLASSIFICATIONS SOFTWARE REFINED (CCSR) FOR ICD-10-PCS PROCEDURES, v2021.1 Issued December 2020 Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP) Phone: (866) 290-HCUP (4287) Email: [email protected] Website: www.hcup-us.ahrq.gov TABLE OF CONTENTS What’s New in v2021.1 of the Clinical Classifications Software Refined (CCSR) for ICD-10-PCS Procedures? .............................................................................................................................. 1 Introduction ................................................................................................................................ 2 Comparison of the CCSR for ICD-10-PCS, the Beta Versions of the CCS for ICD-10-PCS, and the CCS for ICD-9-CM ............................................................................................................... 3 Description of the CCSR for ICD-10-PCS .................................................................................. 4 Understanding the Taxonomy of the ICD-10-PCS Procedure Codes ...................................... 4 The Structure of the CCSR for ICD-10-PCS ........................................................................... 7 General Assignment Guidelines .........................................................................................11 Using the CCSR to Trend ICD-10-PCS Across Data Years .......................................................12 Using the Downloadable CCSR Files ........................................................................................12 -

Cushing Syndrome Due to Black Adrenal Adenoma: Difficulties in the Differential Diagnosis of a Patient with an Adrenal Adenoma
Clínica Universitária de Endocrinologia Cushing Syndrome due to black adrenal adenoma: difficulties in the differential diagnosis of a patient with an adrenal adenoma Mariana Margarida Ferreira Carvalho Maio’2018 1 Clínica Universitária de Endocrinologia Cushing Syndrome due to black adrenal adenoma: difficulties in the differential diagnosis of a patient with an adrenal adenoma Mariana Margarida Ferreira Carvalho Orientado por: Prof. Drª Sónia do Vale 2 Abstract Signs and symptoms of endocrine dysfunction related to adrenal nodules usually are linked to their specific hormonal hypersecretion. Still, these diagnoses are not always a straightforward process and there have been cases in which the clinical expression has been discordant with the tumour histologic features. A 59-year-old woman was observed at the endocrinology outpatient department due to uncontrolled diabetes mellitus. Furthermore, the patient referred paroxysmal high blood pressure and weight loss. Her medical history was remarkable by uncontrolled hypertension, chronic hepatitis C, past pelvic actinomycosis and an adrenal nodule diagnosed due to an unrelated purpose. Endocrine evaluation showed serum morning cortisol, urinary cortisol and metanephrines within the reference range, but supressed adrenocorticotropic hormone (ACTH), loss of cortisol circadian rhythm and a non- suppression in the dexamethasone test, suggesting the diagnosis of Cushing’s syndrome. The imaging procedures were inconclusive. The CT scan revealed a lesion of 20 mm in the left adrenal with a spontaneous density of 33 HU, well-defined contours, a relative wash-out of 61%, and 120HU on portal venous phase. The MRI showed a hyperintense nodule in T1-weighted images, without a signal dropout in out-of-phase T1 imaging. -

Role for Laparoscopic Adrenalectomy in Patients with Cushing's Syndrome Atualização
19-Young-Endo51/8 26/11/07 11:17 Page 1349 Role for Laparoscopic Adrenalectomy in Patients with Cushing’s Syndrome ABSTRACT atualização Laparoscopic adrenalectomy is one of the most clinically important advances in the past 2 decades for the treatment of adrenal disorders. When compared to open adrenalectomy, laparoscopic adrenalectomy is WILLIAM F. Y OUNG, JR. equally safe, effective, and curative; it is more successful in shortening GEOFFREY B. THOMPSON hospitalization and convalescence and has less long-term morbidity. The laparoscopic approach to the adrenal is the procedure of choice for the sur- gical management of cortisol-producing adenomas and for patients with Divisions of Endocrinology, corticotropin (ACTH) dependent Cushing’s syndrome for whom surgery failed to remove the source of ACTH. The keys to successful laparoscopic Diabetes, Metabolism, Nutrition adrenalectomy are appropriate patient selection, knowledge of anatomy, and Internal Medicine (WFY) delicate tissue handling, meticulous hemostasis, and experience with the and the Division of technique of laparoscopic adrenalectomy. (Arq Bras Endocrinol Metab Gastroenterologic and 2007;51/8:1349-1354) General Surgery (GBT), Mayo Clinic, Rochester, Minnesota, Keywords: Adrenalectomy; Cushing’s syndrome; Laparoscopic surgeries USA. RESUMO Papel da Adrenalectomia Laparoscópica em Pacientes com Síndrome de Cushing. A adrenalectomia laparoscópica é um dos avanços clínicos mais importantes das últimas duas décadas para o tratamento de doenças adrenais. Quando comparada à adrenalectomia aberta (convencional), a adrenalectomia laparoscópica é igualmente segura, efetiva e curativa; ela tem maior sucesso em encurtar a hospitalização e a convalescença e apresenta menor morbidade a longo prazo. A abordagem laparoscópica da adrenal é o procedimento de escolha para ao manejo cirúrgico dos adenomas produtores de cortisol e para os pacientes com síndrome de Cushing ACTH-dependente nos quais a cirurgia hipofisária falhou em remover a fonte de ACTH.