Pesticide Poisoning in Chitwan, Nepal: a Descriptive Epidemiological Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Conservation and the Impact of Relocation on the Tharus of Chitwan, Nepal Joanne Mclean Charles Sturt University (Australia)
HIMALAYA, the Journal of the Association for Nepal and Himalayan Studies Volume 19 Number 2 Himalayan Research Bulletin; Special Article 8 Topic: The Tharu 1999 Conservation and the Impact of Relocation on the Tharus of Chitwan, Nepal Joanne McLean Charles Sturt University (Australia) Follow this and additional works at: http://digitalcommons.macalester.edu/himalaya Recommended Citation McLean, Joanne (1999) "Conservation and the Impact of Relocation on the Tharus of Chitwan, Nepal," HIMALAYA, the Journal of the Association for Nepal and Himalayan Studies: Vol. 19 : No. 2 , Article 8. Available at: http://digitalcommons.macalester.edu/himalaya/vol19/iss2/8 This Research Article is brought to you for free and open access by the DigitalCommons@Macalester College at DigitalCommons@Macalester College. It has been accepted for inclusion in HIMALAYA, the Journal of the Association for Nepal and Himalayan Studies by an authorized administrator of DigitalCommons@Macalester College. For more information, please contact [email protected]. Conservation and the linpact of Relocation on the Tharus of Chitwan, Nepal Joanne McLean Charles Sturt University (Australia) Since the establishment of the first national park in the United States in the nineteenth century, indig enous peoples have been forced to move from regions designated as parks. Some of these people have been relocated to other areas by the government, more often they have been told to leave the area and are given no alternatives (Clay, 1985:2). Introduction (Guneratne 1994; Skar 1999). The Thant are often de scribed as one people. However, many subgroups exist: The relocation of indigenous people from national Kochjla Tharu in the eastern Tarai, Chitwaniya and Desauri parks has become standard practice in developing coun in the central Tarai, and Kathariya, Dangaura and Rana tries with little regard for the impacts it imposes on a Tharu in the western Tarai (Meyer & Deuel, 1999). -

Nepal – Maoists – Chitwan – State Protection – Local Government – Ward Chairmen
Refugee Review Tribunal AUSTRALIA RRT RESEARCH RESPONSE Research Response Number: NPL17502 Country: Nepal Date: 2 September 2005 Keywords: Nepal – Maoists – Chitwan – State protection – Local government – Ward Chairmen This response was prepared by the Country Research Section of the Refugee Review Tribunal (RRT) after researching publicly accessible information currently available to the RRT within time constraints. This response is not, and does not purport to be, conclusive as to the merit of any particular claim to refugee status or asylum. Questions 1. Can you provide information on the activities of Maoists in Chitwan and the ability of the authorities to provide protection for individuals against threats from Maoists? 2. Do the Maoists have an office in Chitwan? Letter head paper or contact address? 3. What is a Ward and a Ward Chairman? 4. Is there evidence of the Maoists targeting members of Municipal councils or Ward Chairmen? RESPONSE 1. Can you provide information on the activities of Maoists in Chitwan and the ability of the authorities to provide protection for individuals against threats from Maoists? Activities A December 2002 Research Response provides information on Maoists in Chitwan suggesting it is a quiet area and they are mainly active in remote villages (RRT Country Research 2002 Research Response NPL17502, 24 December, question 1 – Attachment 1). A recent news item from the al Jazeera website refers to the Maoist-controlled district of Chitwan (‘Nepal blast triggers hunt for Maoists’ 2005, al Jazeera website, source: AFP, 6 June http://english.aljazeera.net/NR/exeres/9F7BE0A5-E320-4C5B-BD03- 7151D63A574F.htm - accessed 1 September 2005 - Attachment 2). -

Anthropogenic Impacts on Flora Biodiversity in the Forests and Common Land of Chitwan, Nepal
Anthropogenic impacts on flora biodiversity in the forests and common land of Chitwan, Nepal by Ganesh P. Shivakoti Co-Director Population and Ecology Research Laboratory Institute of Agriculture and Animal Science Tribhuvan University, Rampur, Nepal e-mail: [email protected] Stephen A. Matthews Research Associate Population Research Institute The Pennsylvania State University 601 Oswald Tower University Park, PA 18602-6211 e-mail: [email protected] and Netra Chhetri Graduate Student Department of Geography The Pennsylvania State University 302 Walker Building University Park, PA 16802 e-mail: [email protected] DRAFT COPY September 1997 Acknowledgment: This research was supported by two grants from the National Institute of Child Health and Development (Grant #R01-HD31982 and Grant #RO1-HD33551). We wish to thank William Axinn (PI on these grants), Dirgha Ghimire and the staff at the Population and Ecology Research Laboratory (PERL), IAAS, Nepal who helped collect the flora and common land data. Population growth and deforestation are serious problems in Chitwan and throughout Nepal. In this paper we explore the effect of social and demographic driving forces on flora diversity in Nepal. Specifically, we focus our attention on the flora diversity in three forested areas surrounding a recently deforested, settled and cultivated rural area - the Chitwan District. We have collected detailed counts of trees, shrubs, and grasses along the edge and in the interior of each forested area, and for common land throughout the settled area. Our sampling frame (described in the paper) allows us to construct detailed ordination and classification measures of forest floral diversity. Using techniques from quantitative ecology we can quantify species diversity (relative density, frequency and abundancy), and specifically measure the 'evenness' and 'richness' of the flora in the forested areas and common land. -

Enterprises for Self Employment in Banke and Dang
Study on Enterprises for Self Employment in Banke and Dang Prepared for: USAID/Nepal’s Education for Income Generation in Nepal Program Prepared by: EIG Program Federation of Nepalese Chambers of Commerce and Industry Shahid Sukra Milan Marg, Teku, Kathmandu May 2009 TABLE OF CONTENS Page No. Acknowledgement i Executive Summary ii 1 Background ........................................................................................................................ 9 2 Objective of the Study ....................................................................................................... 9 3 Methodology ...................................................................................................................... 9 3.1 Desk review ............................................................................................................... 9 3.2 Focus group discussion/Key informant interview ..................................................... 9 3.3 Observation .............................................................................................................. 10 4 Study Area ....................................................................................................................... 10 4.1 Overview of Dang and Banke district ...................................................................... 10 4.2 General Profile of Five Market Centers: .................................................................. 12 4.2.1 Nepalgunj ........................................................................................................ -

Krishna Kaphle, Bvsc and AH,,GHC, ELT, Phd
Krishna Kaphle, BVSc and AH,,GHC, ELT, PhD Current Position: Director, Veterinary Teaching Hospital and As- sociate Professor at Department of Theriogenology Institution: Institute of Agriculture and Animal Science Tribhuvan University, Paklihawa Campus, Sidharthanagar-1, Rupandehi, Lumbini, Nepal E-mails and phone: [email protected]; [email protected]; [email protected] Phone: : +977-71-506150; Cell: 9845056734 Research Interest: ONE HEALTH ADVOCATING VETERINARIAN (THERIOGENOLOGIST) Objective: In pursuit of establishing best approach for delivery of animal health, animal welfare and public health concerns in Nepalese society. Get deeper in understanding the science behind origin of life. Beliefs: Engaged faculty and motivated student make the teach- ing and learning meaningful and nothing transform society bet- ter than right education. MAJOR ROLES, RESPONSIBILITIES AND PUBLICATIONS Education Aug 2001 – May 2006 (PhD) -National Taiwan University,, Taipei, Tai- wan, Republic Of China (ROC). Aug 1991 – 1997 (BVSc and AH) -Rampur Campus, Institute of Agri- culture and Animal Science (IAAS), Tribhuvan University (TU), Bharat- pur, Chitwan, Bagmati, Nepal. Responsibilities Assistant Professor: since 2055-01-15 at Rampur Campus, IAAS, TU. Hostel Warden, Sports Coach, Student Welfare Chief, member of various committees, at IAAS, TU. Advisory role for various students clubs, coordinator of national and regional events related with professional, sports and leadership training. Editorial roles for IAAS Journal, NVA Journal, The Blue Cross and multiple others. Department Head of Theriogenology- (April 10th 2009 and again from July 2021), IAAS, TU. Stints as Member secretary Internship Advisory Committee, Subject Matter Com- mittee (Veterinary Science) now as member, Member of Faculty Board (2018-). Advisor of Internship students (~20) and PG students as minor advisor (10). -
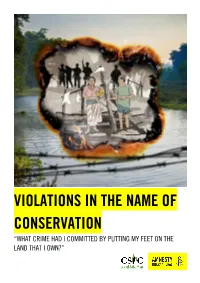
Violations in the Name of Conservation “What Crime Had I Committed by Putting My Feet on the Land That I Own?”
VIOLATIONS IN THE NAME OF CONSERVATION “WHAT CRIME HAD I COMMITTED BY PUTTING MY FEET ON THE LAND THAT I OWN?” Amnesty International is a movement of 10 million people which mobilizes the humanity in everyone and campaigns for change so we can all enjoy our human rights. Our vision is of a world where those in power keep their promises, respect international law and are held to account. We are independent of any government, political ideology, economic interest or religion and are funded mainly by our membership and individual donations. We believe that acting in solidarity and compassion with people everywhere can change our societies for the better. © Amnesty International 2021 Except where otherwise noted, content in this document is licensed under a Creative Commons Cover photo: Illustration by Colin Foo (attribution, non-commercial, no derivatives, international 4.0) licence. Photo: Chitwan National Park, Nepal. © Jacek Kadaj via Getty Images https://creativecommons.org/licenses/by-nc-nd/4.0/legalcode For more information please visit the permissions page on our website: www.amnesty.org Where material is attributed to a copyright owner other than Amnesty International this material is not subject to the Creative Commons licence. First published in 2021 by Amnesty International Ltd Peter Benenson House, 1 Easton Street London WC1X 0DW, UK Index: ASA 31/4536/2021 Original language: English amnesty.org CONTENTS 1. EXECUTIVE SUMMARY 5 1.1 PROTECTING ANIMALS, EVICTING PEOPLE 5 1.2 ANCESTRAL HOMELANDS HAVE BECOME NATIONAL PARKS 6 1.3 HUMAN RIGHTS VIOLATIONS BY THE NEPAL ARMY 6 1.4 EVICTION IS NOT THE ANSWER 6 1.5 CONSULTATIVE, DURABLE SOLUTIONS ARE A MUST 7 1.6 LIMITED POLITICAL WILL 8 2. -

A Yellow-Throated Marten Martes Flavigula Carrying a Small Indian Civet Viverricula Indica
A Yellow-throated Marten Martes flavigula carrying a Small Indian Civet Viverricula indica Babu Ram LAMICHHANE1*, Chiranjibi Prasad POKHERAL1, Ambika Prasad KHATIWADA1, Rama MISHRA2 and Naresh SUBEDI1 Abstract Yellow-throated Marten Martes flavigula has a wide geographic distribution, but little is known about its ecology and behaviour. A camera-trap survey in and around Chitwan National Park, Nepal, photographed a solitary Marten carrying a Small Indian Civet Viverricula indica. The animal was in a grassland patch amid Sal Shorea robusta forest. It is unclear whether the Marten killed the Civet. Recent camera-trap surveys suggest that Yellow-throated Marten is widespread in Chitwan NP with records from altitudes of 190–675 m; many records are from Sal forest. Keywords: camera-trap, Chitwan National Park, behaviour, distribution, intra-guild carnivore predation, locality records, Nepal, Sal forest मऱसाप्रोऱे सानो ननरबिराऱो आहाराको 셁पमा 쥍याईरहेको बौगोलरक वितयणऺेत्र ठू रो बएताऩनन भरसाप्रोको आननफानीको फायेभा थोयैभात्र जानाकायी यहेको छ। मसि셍ष (२०७० सारभा) 啍माभया ट्रमावऩङ प्रविधधको प्रमोग गयी गरयएको सिेऺणको क्रभभा सारिनरे घेरयएको घाॉसे भैदान ऺेत्रभा भरसाप्रोरेए啍रै एउटा िम�क ननयबफयारो 쥍माईयहेको पोटो खिचेको धथमो। पोटोको आधायभा भात्र उ啍त भरसाप्रोरे ननयबफयारो भायेको हो कक होईन एककन गनष सककएन। मसैगयी ऩनछ쥍रा केही ि셍षभा गरयएका 啍माभेया ट्रमावऩङ सिेऺणको क्रभभा धचतिनको धेयैजसो ऺत्रे भा भरसाप्रोरे विचयण गने गयेको य १९० देखि ६७५ लभटय स륍भको उचाईभा ऩाईएको धथमो। भरसाप्रोको पोटो खिधचएका धेयैजसो ठाउॉ सारिन ऺत्रे भा ऩदषछन।् Introduction riverine and mixed hardwood), 12% grassland, 5% exposed surface and 3% water bodies (Thapa 2011). -

Provincial Summary Report Province 3 GOVERNMENT of NEPAL
National Economic Census 2018 GOVERNMENT OF NEPAL National Economic Census 2018 Provincial Summary Report Province 3 Provincial Summary Report Provincial National Planning Commission Province 3 Province Central Bureau of Statistics Kathmandu, Nepal August 2019 GOVERNMENT OF NEPAL National Economic Census 2018 Provincial Summary Report Province 3 National Planning Commission Central Bureau of Statistics Kathmandu, Nepal August 2019 Published by: Central Bureau of Statistics Address: Ramshahpath, Thapathali, Kathmandu, Nepal. Phone: +977-1-4100524, 4245947 Fax: +977-1-4227720 P.O. Box No: 11031 E-mail: [email protected] ISBN: 978-9937-0-6360-9 Contents Page Map of Administrative Area in Nepal by Province and District……………….………1 Figures at a Glance......…………………………………….............................................3 Number of Establishments and Persons Engaged by Province and District....................5 Brief Outline of National Economic Census 2018 (NEC2018) of Nepal........................7 Concepts and Definitions of NEC2018...........................................................................11 Map of Administrative Area in Province 3 by District and Municipality…...................17 Table 1. Number of Establishments and Persons Engaged by Sex and Local Unit……19 Table 2. Number of Establishments by Size of Persons Engaged and Local Unit….….27 Table 3. Number of Establishments by Section of Industrial Classification and Local Unit………………………………………………………………...34 Table 4. Number of Person Engaged by Section of Industrial Classification and Local Unit………………………………………………………………...48 Table 5. Number of Establishments and Person Engaged by Whether Registered or not at any Ministries or Agencies and Local Unit……………..………..…62 Table 6. Number of establishments by Working Hours per Day and Local Unit……...69 Table 7. Number of Establishments by Year of Starting the Business and Local Unit………………………………………………………………...77 Table 8. -

Gunjaman Singh Hospital, Pithuwa Village, Chitwan District, Nepal
Gunjaman Singh Hospital, Pithuwa Village, Chitwan District, Nepal GGHH Agenda Goals Energy Hospital Goals 1. Reduce energy costs 2. Reduce carbon dioxide emissions 3. Continue to treat patients during power cuts Progress Achieved Our solar panel installation (Photo below) is working perfectly. With careful power management we have enough electric power, for the hospital and doctors’ quarters even during load shedding (power outages) of sometimes up to 18 hours per day. This includes power for the x-ray machine and the waste autoclave. We have completely CO 2 free energy and low energy cost for loading batteries sometimes when there isn’t enough sunshine. The cost of installation for sixteen panels, the inverter and the sixteen batteries of 100Ah system was around 12,000 CHF (US$13,000) in 2010; prices have dropped since The Issue The hospital is funded by Swiss NGO “Shanti Med Nepal” and private sponsorship. Environmental health and sustainability is an important factor in decisions in the development in the hospital. Sustainability Strategy Implemented Solar energy was installed as a priority for the hospital as soon as Shanti Med became involved in its operation. Implementation process In such a small facility, the decision making and implementation process is comparatively simple. Dr Gonseth was responsible for selecting the projects to be undertaken, any necessary fundraising, identifying collaboration partners and directing implementation for all elements within GSH. Tracking Progress Solar power: success is measured by the ability of the system to produce all the electricity required by the health post and staff quarters. The level of power in the battery system is recorded and allows demand to be managed through the day. -

ZSL National Red List of Nepal's Birds Volume 5
The Status of Nepal's Birds: The National Red List Series Volume 5 Published by: The Zoological Society of London, Regent’s Park, London, NW1 4RY, UK Copyright: ©Zoological Society of London and Contributors 2016. All Rights reserved. The use and reproduction of any part of this publication is welcomed for non-commercial purposes only, provided that the source is acknowledged. ISBN: 978-0-900881-75-6 Citation: Inskipp C., Baral H. S., Phuyal S., Bhatt T. R., Khatiwada M., Inskipp, T, Khatiwada A., Gurung S., Singh P. B., Murray L., Poudyal L. and Amin R. (2016) The status of Nepal's Birds: The national red list series. Zoological Society of London, UK. Keywords: Nepal, biodiversity, threatened species, conservation, birds, Red List. Front Cover Back Cover Otus bakkamoena Aceros nipalensis A pair of Collared Scops Owls; owls are A pair of Rufous-necked Hornbills; species highly threatened especially by persecution Hodgson first described for science Raj Man Singh / Brian Hodgson and sadly now extinct in Nepal. Raj Man Singh / Brian Hodgson The designation of geographical entities in this book, and the presentation of the material, do not imply the expression of any opinion whatsoever on the part of participating organizations concerning the legal status of any country, territory, or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. The views expressed in this publication do not necessarily reflect those of any participating organizations. Notes on front and back cover design: The watercolours reproduced on the covers and within this book are taken from the notebooks of Brian Houghton Hodgson (1800-1894). -

Cases of Farmer Managed Irrigation Systems from East Chitwan'
Dynamics in Water Rights and Arbitration on Water Right Conflicts: Cases of Farmer Managed Irrigation Systems from East Chitwan' A. Shukla, N. R. Joshi, G. Shivakoti, R. Poudel and N. Shrestha' INTRODUCTION This paper examines the dynamism in water rights from the perspective of property creating process and its regulation and use and the mechanisms of arbitration when conflicts arise in the process. In conceptualizing irrigation development as property, the paper draws upon the property framework of Coward (1983). The development and subsequent management of irrigation systems involve investment of resources of some form, whether capital, labor, material or know- how. The mobilization and investment of resources may occur in private, community or state management regimes. Those who make the investment develop claims on the water supply that is acquired and the physical structures that are created for acquisition, conveyance, regulation and distribution of available supply of water. Even in the case of the state management, the investment of resources for imgation development has a targeted area and users to serve. Within the system each individual who has invested in the development and management of irrigation system has claim on the portion of available water supply. The collective claim on acquired supply of water is therefore apportioned into individual's claim. In defining the individual's claim the imgators come to a set of agreements that creates a social contract for 173 irrigators to realize their claims and acknowledge the claims of others. These agreements are apparent in the forms of rules, roles and sanctions to define, constrain and enforce individual’s claims (Pradhan 1987).While in some irrigation systems the set ofagreements are well articulated, in others there may be little codification. -

INTRODUCTION Social and Economic Benefi Ts
60/ The Third Pole SOCIO-ECONOMIC IMPACT OF TOURISM IN SAURAHA CHITWAN, NEPAL Tej Prasad Sigdel Teaching Assistant, Department of Geography Education, T. U., Nepal Abstract In Nepal, the number of tourist arrivals and stay their length have been increasing day to day. This incensement has directly infl uenced the socio-economic status of Nepalese people. The main objective of this paper is to explore the socio- economic impact of tourism on Sauraha. To fulfi ll the objective both primary and secondary data had been used. There are both direct and indirect impacts on socio-economic condition of local people. Tourism has contributed a lot a raising the awareness among the communities, preserving traditional culture, values, norms and heritage. But it is also facing a problem of sanitation, improper solid waste management, unmanaged dumping site and poaching wild life. Tourism development in Sauraha should be assessed both the local traditions and culture. Key Words: Tourism, socio-economic impact, World Heritage Site, sustainable development INTRODUCTION social and economic benefi ts. Economic benefi ts are, increased government revenue through various In general term, ‘tourism’ denotes the journey of types of taxation, create a jobs and increase family human beings from one place to the another, where and community income, provide the opportunity it may be within own country or second countries for for innovation and creativity, provides the support various purposes. The word ‘Tourism’ which was th for existing business and services, helps to develop originated in the 19 century and was popularized local crafts and trade and develop international in 1930s, but its signifi cance was not fully realized peace and understanding.