Philadelphia Councilman-At-Large Dennis M. O'brien
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Historic Philadelphia, Inc. 2012 Fall Programming Fact Sheet
PRESS CONTACT: Cari Feiler Bender, Relief Communications, LLC (610) 416-1216, [email protected] HISTORIC PHILADELPHIA, INC. 2012 FALL PROGRAMMING FACT SHEET DESCRIPTION: Historic Philadelphia, Inc. makes our nation’s history relevant and real through interpretation, interaction, and education, strengthening Greater Philadelphia’s role as the destination to experience American history. Historic Philadelphia, Inc.’s Once Upon A Nation brings history to life, featuring Adventure Tours (walking tours), History Makers, Storytelling Benches throughout the Historic District and at Valley Forge, and the Benstitute to specially train all staff. Franklin Square is an outdoor amusement oasis with Philadelphia-themed Mini Golf, the Philadelphia Park Liberty Carousel, and SquareBurger, hosting parties and special events in the new Pavilion in Franklin Square. Liberty 360 , a digital 3-D experience, is a year-round indoor attraction housed at the Historic Philadelphia Center as Phase I of the all-new completely re-imagined Lights of Liberty . The Betsy Ross House allows visitors a personal look at the story and home of a famous historical figure, with newly remodeled and reinterpreted rooms and changing exhibitions. LIBERTY 360: Liberty 360 in the PECO Theater immerses the viewer in the symbols of freedom. Benjamin Franklin appears in a groundbreaking 360-degree, 3-D show unlike anything that has ever been seen before, and escorts the audience on a journey of discovery and exploration of America’s most beloved symbols. The 15-minute, 3-D film surrounds -

The Battles of Germantown: Public History and Preservation in America’S Most Historic Neighborhood During the Twentieth Century
The Battles of Germantown: Public History and Preservation in America’s Most Historic Neighborhood During the Twentieth Century Dissertation Presented in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in the Graduate School of The Ohio State University By David W. Young Graduate Program in History The Ohio State University 2009 Dissertation Committee: Steven Conn, Advisor Saul Cornell David Steigerwald Copyright by David W. Young 2009 Abstract This dissertation examines how public history and historic preservation have changed during the twentieth century by examining the Germantown neighborhood of Philadelphia, Pennsylvania. Founded in 1683, Germantown is one of America’s most historic neighborhoods, with resonant landmarks related to the nation’s political, military, industrial, and cultural history. Efforts to preserve the historic sites of the neighborhood have resulted in the presence of fourteen historic sites and house museums, including sites owned by the National Park Service, the National Trust for Historic Preservation, and the City of Philadelphia. Germantown is also a neighborhood where many of the ills that came to beset many American cities in the twentieth century are easy to spot. The 2000 census showed that one quarter of its citizens live at or below the poverty line. Germantown High School recently made national headlines when students there attacked a popular teacher, causing severe injuries. Many businesses and landmark buildings now stand shuttered in community that no longer can draw on the manufacturing or retail economy it once did. Germantown’s twentieth century has seen remarkably creative approaches to contemporary problems using historic preservation at their core. -

0511House-Urban Affairsmichelle
1 1 COMMONWEALTH OF PENNSYLVANIA HOUSE OF REPRESENTATIVES 2 URBAN AFFAIRS COMMITTEE 3 COATESVILLE CITY HALL, COUNCIL CHAMBERS 4 WEDNESDAY, MAY 11, 2016 5 10:00 A.M. 6 PUBLIC HEARING ON BLIGHT 7 8 BEFORE: HONORABLE SCOTT A. PETRI, MAJORITY CHAIR HONORABLE BECKY CORBIN 9 HONORABLE JERRY KNOWLES HONORABLE HARRY LEWIS 10 HONORABLE JAMES R. SANTORA HONORABLE ED NEILSON 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 2 1 COMMITTEE STAFF PRESENT CHRISTINE GOLDBECK 2 EXECUTIVE DIRECTOR, HOUSE URBAN AFFAIRS COMMITTEE 3 V. KURT BELLMAN 4 RESEARCH ANALYST, DEMOCRATIC COMMITTEE 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 3 1 I N D E X 2 OPENING REMARKS By Chairman Petri 5 - 6 3 By Representative Santora 6 By Representative Knowles 6 - 7 4 By Representative Nielson 7 - 8 5 REMARKS By Chairman Petri 8 - 10 6 OPENING REMARKS 7 By Representative Corbin 10 - 11 By Representative Lewis 11 - 14 8 By Linda Lavender Norris 14 9 DISCUSSION AMONG PARTIES 15 - 19 10 PRESENTATION By Dave Sciocchetti 19 - 22 11 QUESTIONS FROM COMMITTEE MEMBERS 23 - 28 12 PRESENTATION 13 By Michael Trio 28 - 38 By Sonia Huntzinger 38 - 42 14 QUESTIONS FROM COMMITTEE MEMBERS 42 - 59 15 PRESENTATION 16 By Joshua Young 59 - 65 By Kristin Camp 65 - 70 17 QUESTIONS FROM COMMITTEE MEMBERS 70 - 77 18 PRESENTATION 19 By Jack Assetto 78 - 81 By James Thomas 81 - 85 20 QUESTIONS FROM COMMITTEE MEMBERS 85 - 89 21 PRESENTATION 22 By Dr. -

Wells Fargo Center Suite Menu.Pdf
Packages The Bella Vista 525/550 Event Day PACKAGES SERVE APPROXIMATELY 12 GUESTS FEDERAL PRETZELS Philadelphia Classic Sea Salt Soft Pretzels, Spicy Mustard (350 cal per Pretzel) (10 cal per 2 oz Spicy Mustard) POPCORN gf Enhance Your Experience Bottomless Fresh Popped, Souvenir Pail (190 cal per 1 oz serving) To further enhance your experience add one of our other menu favorites. ® UTZ WAVY POTATO CHIPS gf CHICKIE’S & PETE’S ® WORLD FAMOUS Onion Dip ® (280 cal per 1.8 oz Wavy Potato Chips) (150 cal per 1.3 oz Onion Dip) CRAB FRIES gf 54 Cheese Sauce CHICKIE’S & PETE’S ® CUTLETS (1140 cal per 13.3 oz Fries) (130 cal per 2.7 oz Cheese Sauce) Two orders of the World Famous Cutlets, with Honey Mustard & BBQ (1170 cal per 13.4 oz Cutlet) (230 calories per 1.7 oz Honey Mustard) (90 cal per 1.7 oz BBQ) FARMERS’ MARKET SEASONAL CRUDITÉ gf 54 Carrots, Peppers, English Cucumbers, Broccoli, Ranch Dressing SMOKED TURKEY HOAGIE (110 cal per 5.2 oz Vegetables) (80 cal per.85 oz Ranch Dressing) House Smoked Turkey, Herb Cheese Spread, Bacon, Roasted Red Pepper, Arugula, Amoroso ® Seeded Roll (410 cal 9.66 oz Smoked Turkey Hoagie) BEVERAGE PACKAGE #1 170 1 Six-Pack Each of Pepsi, Diet Pepsi, Sierra Mist, PHILLY CHEESESTEAKS Bottled Water and 3 Six-Packs of Domestic Beer of Your Choice “Wit” Sautéed Onions, Cheese Sauce, Amoroso ® Roll (570 cal per 12.31 oz Philly Cheesesteak) SERVES 6 DIETZ & WATSON ® GRILLED ARENA HOT DOGS All Beef Hot Dogs, Sauerkraut, Potato Buns (350 cal per 4.48 oz Hot Dog) (5 cal per oz 1.34 Sauerkraut) (150 cal 1.87 per oz Potato Bun) The calorie and nutrition information provided is for individual servings , FRESH BAKED COOKIES not for the total number of servings on each tray, because serving Chef’s Choice of Fresh Baked Cookies styles e.g. -
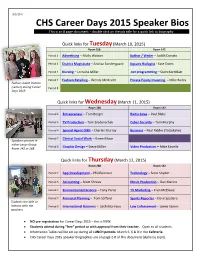
CHS Career Days 2015 Speaker Bios This Is an 8 Page Document – Double Click on the Job Title for a Quick Link to Biography
3/3/15 C CHS Career Days 2015 Speaker Bios This is an 8 page document – double click on the job title for a quick link to biography. Quick links for Tuesday (March 10, 2015) Room 268 Room 142 Period 2 Advertising – Molly Watson Author / Writer – Judith Donato Period 3 District Magistrate – Analisa Sondergaard Aquatic Biologist - Kate Doms Period 4 Nursing – Lorraine Miller .net programming – Scott Kornblatt Period 7 Fashion Retailing – Wendy McDevitt Private Equity Investing – Mike Bailey Author, Judith Donato (center) during Career Period 8 Days 2013 Quick links for Wednesday (March 11, 2015) Room 268 Room 142 Period 2 Entrepreneur – Tom Borger Radio Sales – Paul Blake Period 3 TV Production – Tom Sredenschek Cyber Security – Tom Murphy Period 4 Special Agent (FBI) – Charles Murray Business – Paul Ridder (Tastykake) Period 7 Clinical Social Work – Karen Moon Speakers present in either Large Group Period 8 Graphic Design – Steve Miller Video Production – Mike Fanelle Room 142 or 268. Quick links for Thursday (March 12, 2015) Room 268 Room 142 Period 2 App Development – Phil Reitnour Technology – Scott Snyder Period 3 Accounting – Scott Shreve Music Production – Dan Marino Period 4 Environmental Science – Tony Parisi TV Marketing – Fran McElwee Period 7 Financial Planning – Tom Safford Sports Reporter – Dave Spadaro Students are able to interact with the Period 8 International Business – Seth Morrison Law Enforcement – Jamie Kemm speakers. NO pre-registration for Career Days 2015 – this is NEW. Students attend during “free” period or with approval from their teacher. Open to all students. Information Tables will be set up during all LUNCH periods: March 5, 6 & 9 in the Cafeteria CHS Career Days 2015 speaker biographies are on page 2-8 of this document (alpha by topic). -

Notre Dame Welcomes Dr. Judith A. Dwyer As Its 4Th President Notre
Annual Report2013-14 inside VISIONSVISIONSACADEMY of NOTREAcademy DAME of de NotreNAMUR Dame de Namur FALL 2014 NotreNotre DameDame WelcomesWelcomes Dr.Dr. JudithJudith A.A. DwyerDwyer asas itsits 4th4th PresidentPresident VISIONS MAGAZINE . FALL 2014 . 1 MESSAGE FROM THE PRESIDENT How does the Notre Dame community describe excellence? I am pleased to share this combined issue of Visions and the 2013-2014 Annual Report of Gifts with you. The magazine portion highlights the academic rigor, community engagement, and spiritual depth that continue to define our tradition of educational excellence. The report testifies to the generosity of so many members of our community, who support our mission and core values. Together, they tell the story of how the Academy honors the past, celebrates the present, and secures the future in the pioneering spirit of the Sisters of Notre Dame de Namur. Judith A. Dwyer, Ph.D. How does Notre Dame describe excellence? Our students excel in academic, President artistic, and athletic achievements. Our alumnae continue to lead and achieve Eileen Wilkinson (see article on Margaret [Meg] Kane ’99, this year’s Notre Dame Award recipient, Principal on page 12). It is this legacy and dynamic learning environment that the gifts described in the Annual Report support. Jacqueline Coccia Academic Dean The “Our Time to Inspire” campaign seeks to ensure Notre Dame’s reputation Madeleine Harkins The Mansion. The Mansion continues to be a defining part of our school and our lives. as a premier Catholic academy for young women by providing an enhanced, Dean of Student Services 8 innovative, and dynamic learning environment. -
DVRPC FY 2009 Transportation Improvement Program (TIP)
The Delaware Valley Regional Planning Commission is dedicated to uniting the re- gion’s elected officials, planning professionals and the public with a common vision of making a great region even greater. Shaping the way we live, work and play, DVRPC builds consensus on improving transportation, promoting smart growth, protecting the environment and enhancing the economy. We serve a diverse region of nine counties: Bucks, Chester, Delaware, Montgomery and Philadelphia in Pennsylvania; and Bur- lington, Camden, Gloucester and Mercer in New Jersey. DVRPC is the federally desig- nated Metropolitan Planning Organization for the Greater Philadelphia Region - leading the way to a better future. Our logo is adapted from the official DVRPC seal, and is designed as a stylized image of the Delaware Valley. The outer ring symbolizes the region as a whole, while the diagonal bar signifies the Delaware River. The two adjoining crescents represent the Commonwealth of Pennsylvania and the State of New Jersey. DVRPC is funded by a variety of funding sources including federal grants from the U.S. Department of Transportation’s Federal Highway Administration (FHWA) and Federal Transit Administration (FTA), the Pennsylvania and New Jersey departments of trans- portation, as well as by DVRPC’s state and local member governments. The authors, however, are solely responsible for its findings and conclusions, which may not repre- sent the official views or policies of the funding agencies. DVRPC Fiscal Year 2009 Transportation Improvement Program Volume IV -
BRAC and EPA's Federal Facility Cleanup Program
BRAC AND EPA’S FEDERAL FACILITY CLEANUP PROGRAM: Three Decades of Excellence, Innovation and Reuse INTRODUCTION EPA serves the public by supporting The Big Picture: innovative, cost-effective cleanups at Accomplishments at BRAC Sites federal facilities and the return of those facilities to productive use. We work extensively with other federal agencies, state and local governments, and Transforming military installations into centers for community representatives to ensure that business, industry, residential communities and facilities meet environmental standards education. and are ready for redevelopment. EPA assists in the transfer of properties and provides regulatory oversight at Creating jobs through cleanup and reuse. many types of Department of Defense (DoD) sites, including Base Realignment and Closure (BRAC) sites. Because these facilities often encompass hundreds of Fostering partnerships among federal, state and acres with buildings, roads and other infrastructure, their effective and efficient local governments. cleanup and reuse can play a pivotal role in communities’ economic development. This report takes a closer look at EPA’s Providing recreational and open space. work in support of DoD and its BRAC environmental restoration and reuse efforts over the past three decades. At more than 100 BRAC sites nationwide, EPA has provided resources to accelerate Involving local communities in cleanup and reuse environmental restoration activities, plans. maintain remedies that protect human health and the environment, support public involvement, and facilitate property transfer. 2 BRAC, DoD and EPA: A Quick Overview To sustain and streamline military readiness, DoD recognized the need to close some FFRRO Goals installations and redefine the Department’s mission at others. To date, DoD and Congress have implemented five BRAC rounds, in 1988, 1991, 1993, 1995 and 2005. -

View Annual Report
Dear Shareholder: The year 2012 was eventful for Flowers Foods and for our industry. Our company delivered solid sales and earnings growth despite persistent economic headwinds and the ongoing integration of two major acquisitions–Tasty Baking and Lepage Bakeries. The Flowers team did an outstanding job last year, and we’re proud of how they rallied to serve the market when Hostess Brands abruptly closed its doors in November. We ended the year riding a wave of momentum that continues today. Key results of 2012 include: sales of $3.05 billion, an increase of 9.8% from 2011; net income of $136.1 million, compared to $123.4 million last year, a 10.3% increase; and diluted earnings per share of $0.98 compared to $0.90 in 2011, an 8.9% increase. Our accomplishments reflect the effectiveness of our long-term commitment to investing in our bakeries, improving efficiencies, delivering high-quality products and customer service, and building strong brands. Tasty Baking completed its first year as a Flowers subsidiary in May, and we accomplished much.Tastykakes are now sold from Maine to Florida to Arizona, and consumers in Tasty’s core markets in the Northeast are now able to enjoy Nature’s Own breads and buns. In July, we completed our acquisition of Lepage Bakeries in Maine. Since then, we’ve achieved double-digit sales growth in Lepage markets as we introduced Tastykake and Nature’s Own throughout New England. We are pleased with how consumers in that region are responding, and we appreciate the contributions of our Lepage team members. -

Energy Transitions Are Brown Before They Go Green
ENERGY TRANSITIONS ARE BROWN BEFORE THEY GO GREEN April 2020 Mark Alan Hughes 1 ENERGY TRANSITIONS ARE BROWN BEFORE THEY GO GREEN Mark Alan Hughes April 2020 kleinmanenergy.upenn.edu central business district. It nestles among residential “We need to think not only neighborhoods, the airport, three stadiums, and the revitalized Navy Yard office district containing iconic Philly brands like Urban Outfitters, GSK, and Tastykake. of ‘green financing’ but The refinery is just down river from three universities, four hospitals, and over $5 billion of office and lab also of ‘brown buyouts’— development supporting 80,000 jobs defining the future of the life sciences and data analytics. and how to pay for them.” Juxtapositions of legacy and prospect are extreme in Philadelphia but also represent an often-overlooked truth CARY COGLIANESE about the energy transition: it starts brown before it goes DIRECTOR, PENN PROGRAM ON REGULATION, PENN LAW green. The energy transition starts with legacy assets and incumbent actors whose profits and power derive from Serial bankruptcies, terrifying explosions, and the hydrocarbon resources of wood, coal, oil, and gas permanent closure at the largest oil refinery on the that powered the Industrial Revolution. U.S. eastern seaboard preview the challenges of the These assets and actors are clearly being disrupted by energy transition in the real world, which often starts efforts to contain the damages being done by our use brown before it goes green. Recognizing those initial of these resources by transitioning to a “green” energy conditions is a key factor in accelerating a just and system. But recognizing that this transition often starts efficient transition.1 with a set of powerful initial conditions—call it a “brown” The Atlantic Refinery was established near the energy system—is a key policy driver in accelerating a just confluence of the Schuylkill and Delaware Rivers in 1866, and efficient transition. -

Leon Sullivan's Fight Against Job Discrimination
“Don’t Buy Where You Can’t Work”: Leon Sullivan’s Fight Against Job Discrimination Giuliana Alleva Senior Individual Documentary Process Paper: 498 Words Alleva 2 Process Paper Despite living in Philadelphia, I did not know about the Civil Rights movements that originated in my city. When deciding on what topic I was going to research for this project, I knew I wanted to study a topic that was unique to the city I lived in, because I was interested in understanding the local history in Philadelphia. After briefly researching the Selective Patronage Campaign, one of Leon Sullivan’s projects, I became fascinated with the ways in which the black community was able to dimish the barrier of job discrimination through collective action. Leon Sullivan proved to be the perfect subject matter due to the wide array of projects he launched in Philadelphia, and his clear goal to diminish discrimination in the workplace. Due to the fact that Leon Sullivan did most of his work in Philadelphia, I had access to a vast amount of primary sources. I made several trips to the Special Collections Research Center at the Temple University Libraries where I was able to read newspaper articles about Leon Sullivan’s work, and I also found a plethora of images from their digital collections online. Furthermore, I read several books about Leon Sullivan’s work such as Up South by Matthew Countryman, The Problem of Jobs by Guian Mckee, and Build, Brother, Build, which was written by Leon Sullivan. Lasty, I had the privilege of conducting interviews with those who were involved with Leon Sullivan’s projects, such as Ms. -

Architecture Program Report for 2012 NAAB Visit for Continuing Accreditation
Philadelphia University Architecture Program, College of Architecture and the Built Environment Architecture Program Report for 2012 NAAB Visit for Continuing Accreditation Bachelor of Architecture (166-68 credit hours) Year of the Previous Visit: 2006 Current Term of Accreditation: At the March 2007 meeting of the National Architectural Accrediting Board (NAAB), the board reviewed the Visiting Team Report of the Philadelphia University School of Architecture. “The board noted the concern of the visiting team regarding problems with in several areas. As a result, the professional architecture program – Bachelor of Architecture (166 credit hours) – was formally granted a six-year term of accreditation with the stipulation that a focused evaluation be scheduled in two years to look only at the following: Human Resources and Physical Resources and the progress that has been made in those areas. The accreditation term is effective January 1, 2006. The program is scheduled for its next full accreditation visit in 2012. The focused evaluations are scheduled for the calendar year 2009.” Response to 2009 Focused Visit “After reviewing the Focused Evaluation Program Report submitted by the Philadelphia University Department of Architecture and Interiors as part of the focused evaluation of its Bachelor of Architecture program, in conjunction with the Focused Evaluation Team Report, the National Architectural Accrediting Board (NAAB) has found that the changes made or planned by the program to remove the identified deficiencies are satisfactory. “The program will not be required to report on these deficiencies as part of its Annual Report (AR) to the NAAB; however, the program should continue to include a response to any other deficiencies listed in the most recent Visiting Team Report, as well as report on any modifications made in the program that may affect its adherence to the conditions for accreditation.