Medical Marijuana Consent Form a Qualified Physician May Not Delegate the Responsibility of Obtaining Written Informed Consent to Another Person
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Jus Cogens As a Vision of the International Legal Order Dr
Penn State International Law Review Volume 29 Article 2 Number 2 Penn State International Law Review 9-1-2010 Jus Cogens as a Vision of the International Legal Order Dr. Markus Petsche Follow this and additional works at: http://elibrary.law.psu.edu/psilr Part of the International Law Commons Recommended Citation Petsche, Dr. Markus (2010) "Jus Cogens as a Vision of the International Legal Order," Penn State International Law Review: Vol. 29: No. 2, Article 2. Available at: http://elibrary.law.psu.edu/psilr/vol29/iss2/2 This Article is brought to you for free and open access by Penn State Law eLibrary. It has been accepted for inclusion in Penn State International Law Review by an authorized administrator of Penn State Law eLibrary. For more information, please contact [email protected]. I Articles I Jus Cogens as a Vision of the International Legal Order Dr. Markus Petsche* Table of Contents INTRODUCTION .............................................. 235 I. THE INAPPROPRIATENESS OF CHARACTERIZING JUS COGENS AS A RULE OF INTERNATIONAL LAW AND THE LIMITED RELEVANCE OF JUS COGENS FOR THE PRACTICE OF INTERNATIONAL LAW...................................238 A. FundamentalConceptual and Theoretical Flaws ofJus Cogens .................................... 238 1. Origins of Jus Cogens. .................. ..... 238 2. Jus Cogens as a Set of Norms Lacking Substance........ 242 3. Jus Cogens as a Set of Norms Lacking a Procedure for Its Determination. ............ ......... .......... 243 4. Jus Cogens as a Set of Norms Lacking a Proper Theoretical Basis.......................... 245 B. The Limited Relevance of Jus Cogens for the Law of Treaties: Rare and Unsuccessful Reliance on Jus * DEA (Paris 1); LL.M. (NYU); Ph.D. -

Indigenous and Tribal People's Rights Over Their Ancestral Lands
INTER‐AMERICAN COMMISSION ON HUMAN RIGHTS OEA/Ser.L/V/II. Doc. 56/09 30 December 2009 Original: Spanish INDIGENOUS AND TRIBAL PEOPLES’ RIGHTS OVER THEIR ANCESTRAL LANDS AND NATURAL RESOURCES Norms and Jurisprudence of the Inter‐American Human Rights System 2010 Internet: http://www.cidh.org E‐mail: [email protected] OAS Cataloging‐in‐Publication Data Derechos de los pueblos indígenas y tribales sobre sus tierras ancestrales y recursos naturales: Normas y jurisprudencia del sistema interamericano de derechos humanos = Indigenous and tribal people’s rights over their ancestral lands and natural resources: Norms and jurisprudence of the Inter‐American human rights system / [Inter‐American Commission on Human Rights.] p. ; cm. (OEA documentos oficiales ; OEA/Ser.L)(OAS official records ; OEA/Ser.L) ISBN 978‐0‐8270‐5580‐3 1. Human rights‐‐America. 2. Indigenous peoples‐‐Civil rights‐‐America. 3. Indigenous peoples‐‐Land tenure‐‐America. 4. Indigenous peoples‐‐Legal status, laws, etc.‐‐America. 5. Natural resources‐‐Law and legislation‐‐America. I. Inter‐American Commission on Human Rights. II Series. III. Series. OAS official records ; OEA/Ser.L. OEA/Ser.L/V/II. Doc.56/09 Document published thanks to the financial support of Denmark and Spain Positions herein expressed are those of the Inter‐American Commission on Human Rights and do not reflect the views of Denmark or Spain Approved by the Inter‐American Commission on Human Rights on December 30, 2009 INTER‐AMERICAN COMMISSION ON HUMAN RIGHTS MEMBERS Luz Patricia Mejía Guerrero Víctor E. Abramovich Felipe González Sir Clare Kamau Roberts Paulo Sérgio Pinheiro Florentín Meléndez Paolo G. Carozza ****** Executive Secretary: Santiago A. -

Rights, Respect, Responsibility: Don't Have Sex Without Them
Rights, Respect, Responsibility: Don’t Have Sex Without Them A Lesson Plan from Rights, Respect, Responsibility: A K-12 Curriculum Fostering responsibility by respecting young people’s rights to honest sexuality education. ADVANCE PREPARATION FOR LESSON: NSES ALIGNMENT: • Download the YouTube video on consent, “2 Minutes Will By the end of 12th grade, Change the Way You Think About Consent,” at https://www. students will be able to: youtube.com/watch?v=laMtr-rUEmY. HR.12.CC.3 – Define sexual consent and explain its • Also download the trailer for Pitch Perfect 2 - The Ellen Show implications for sexual decision- version (https://www.youtube.com/watch?v=KBwOYQd21TY), making. queuing it up to play a brief clip between 2:10 and 2:27. PS.12.CC.3 – Explain why using tricks, threats or coercion in • If you cannot download and save these to your desktop in relationships is wrong. advance, talk with your school’s IT person to ensure you have HR.12.INF.2 – Analyze factors, internet access to that link during class. including alcohol and other substances, that can affect the • Print out the skit scenarios and cut out each pair, making sure ability to give or perceive the the correct person 1 goes with the correct person 2. Determine provision of consent to sexual how many pairs there will be in your class and make several activity. copies of each scenario, enough for each pair to get one. TARGET GRADE: Grade 10 LEARNING OBJECTIVES: Lesson 1 By the end of this lesson, students will be able to: 1. -

Cannabis (Sub)Culture, the Subcultural Repository, and Networked Mediation
SIMULATED SESSIONS: CANNABIS (SUB)CULTURE, THE SUBCULTURAL REPOSITORY, AND NETWORKED MEDIATION Nathan J. Micinski A Thesis Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements for the degree of MASTER OF ARTS May 2014 Committee: Ellen Berry, Advisor Rob Sloane © 2014 Nathan Micinski All Rights Reserved iii ABSTRACT Ellen Berry, Advisor Subcultural theory is traditionally rooted in notions of social deviance or resistance. The criteria for determining who or what qualifies as subcultures, and the most effective ways to study them, are based on these assumptions. This project seeks to address these traditional modes of studying subcultures and discover ways in which their modification may lead to new understandings and ways of studying subcultures in the contemporary moment. This will be done by suggesting a change in the criteria of examining subcultures from that of deviance or resistance to identification with a collection of images, symbols, rituals, and narratives. The importance of this distinction is the ability to utilize the insights that studying subcultures can offer while avoiding the faults inherent in speaking for or at a subculture rather than with or from it. Beyond addressing theoretical concerns, this thesis aims to apply notions of subcultural theory to study the online community of Reddit, in particular, a subset known as r/trees–a virtual repository for those images, symbols, rituals, and narratives of cannabis subculture. R/trees illustrates the life and vibrancy of a unique subcultural entity, which to this point has evaded a cultural studies analysis. To that end, this project advocates for the importance of the cultural studies approach to analyzing cannabis subculture and further, to insert the findings of this study into that gap in the literature. -
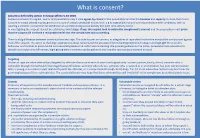
What Is Consent?
What is consent? Consent is defined by section 74 Sexual Offences Act 2003. Someone consents to vaginal, anal or oral penetration only if s/he agrees by choice to that penetration and has the freedom and capacity to make that choice. Consent to sexual activity may be given to one sort of sexual activity but not another, e.g.to vaginal but not anal sex or penetration with conditions, such as wearing a condom. Consent can be withdrawn at any time during sexual activity and each time activity occurs. In investigating the suspect, it must be established what steps, if any, the suspect took to obtain the complainant’s consent and the prosecution must prove that the suspect did not have a reasonable belief that the complainant was consenting. There is a big difference between consensual sex and rape. This aide focuses on consent, as allegations of rape often involve the word of the complainant against that of the suspect. The aim is to challenge assumptions about consent and the associated victim-blaming myths/stereotypes and highlight the suspect’s behaviour and motives to prove he did not reasonably believe the victim was consenting. We provide guidance to the police, prosecutors and advocates to identify and explain the differences, highlighting where evidence can be gathered and how the case can be presented in court. Targeting Victims of rape are often selected and targeted by offenders because of ease of access and opportunity - current partner, family, friend, someone who is vulnerable through mental health/ learning/physical difficulties, someone who sells sex, someone who is isolated or in an institution, has poor communication skills, is young, in a current or past relationship with the offender, or is compromised through drink/drugs. -

Informed Consent, AI Technologies, and Public Health Emergencies
future internet Review Trust, but Verify: Informed Consent, AI Technologies, and Public Health Emergencies Brian Pickering IT Innovation, Electronics and Computing, University of Southampton, University Road, Southampton SO17 1BJ, UK; [email protected] Abstract: To use technology or engage with research or medical treatment typically requires user consent: agreeing to terms of use with technology or services, or providing informed consent for research participation, for clinical trials and medical intervention, or as one legal basis for processing personal data. Introducing AI technologies, where explainability and trustworthiness are focus items for both government guidelines and responsible technologists, imposes additional challenges. Understanding enough of the technology to be able to make an informed decision, or consent, is essential but involves an acceptance of uncertain outcomes. Further, the contribution of AI- enabled technologies not least during the COVID-19 pandemic raises ethical concerns about the governance associated with their development and deployment. Using three typical scenarios— contact tracing, big data analytics and research during public emergencies—this paper explores a trust- based alternative to consent. Unlike existing consent-based mechanisms, this approach sees consent as a typical behavioural response to perceived contextual characteristics. Decisions to engage derive from the assumption that all relevant stakeholders including research participants will negotiate on an ongoing basis. Accepting dynamic negotiation between the main stakeholders as proposed here introduces a specifically socio–psychological perspective into the debate about human responses Citation: Pickering, B. Trust, but to artificial intelligence. This trust-based consent process leads to a set of recommendations for the Verify: Informed Consent, AI ethical use of advanced technologies as well as for the ethical review of applied research projects. -

Marijuana Myths and Facts: the Truth Behind 10 Popular Misperceptions
MARIJUANA myths & FACTS The Truth Behind 10 Popular Misperceptions OFFICE OF NATIONAL DRUG CONTROL POLICY MARIJUANA myths & FACTS The Truth Behind 10 Popular Misperceptions OFFICE OF NATIONAL DRUG CONTROL POLICY TABLE OF CONTENTS Introduction.............................................................................. 1 Myth #1: Marijuana is harmless .......................................... 3 Myth #2: Marijuana is not addictive ................................... 7 Myth #3: Marijuana is not as harmful to your health as tobacco............................................................. 9 Myth #4: Marijuana makes you mellow............................. 10 Myth #5: Marijuana is used to treat cancer and other diseases...................................................... 11 Myth #6: Marijuana is not as popular as MDMA (Ecstasy) or other drugs among teens today...................... 13 Myth #7: If I buy marijuana, I’m not hurting anyone else......................................................... 14 Myth #8: My kids won’t be exposed to marijuana ............. 17 Myth #9: There’s not much parents can do to stop their kids from experimenting with marijuana ........... 19 Myth #10: The government sends otherwise innocent people to prison for casual marijuana use......... 21 Conclusion .............................................................................. 23 Glossary.................................................................................. 25 References .............................................................................. -

Cannabis Ordinance Revisions; Amending Berkeley Municipal Code Chapters 12.21, 12.22, 20.40, 23C.25, and Sub-Titles 23E and 23F
Page 1 of 99 Office of the City Manager PUBLIC HEARING January 28, 2020 To: Honorable Mayor and Members of the City Council From: Dee Williams-Ridley, City Manager Submitted by: Timothy Burroughs, Director, Planning and Development Department Subject: Cannabis Ordinance Revisions; Amending Berkeley Municipal Code Chapters 12.21, 12.22, 20.40, 23C.25, and Sub-Titles 23E and 23F RECOMMENDATION Conduct a public hearing and upon conclusion, provide direction regarding proposed ordinance language alternatives and take the following action: Adopt the first reading of five ordinances to amend the Berkeley Municipal Code (BMC) Chapters 12.21, 12.22, 20.40, 23C.25, and Sub-Titles 23E and 23F which would: A. Allow new business types (Delivery-Only Retailers, Consumption Lounges); B. Allow Retailers to continue to operate as Microbusinesses; C. Clarify cannabis business operational standards and development standards, such as quotas and buffers, for Storefront Retailers; D. Allow more opportunities for Commercial Cultivation by expanding location options; and E. Protect the health of the general public and youth with additional advertising, signage and sales regulations. SUMMARY The proposed cannabis ordinances would revise definitions and establish operating standards for new and existing cannabis businesses in Berkeley, and include new regulations based on commission recommendations, Council direction, and Resolution 68,326-N.S., which established Berkeley as a sanctuary city for recreational cannabis use. The new ordinances would fully address new uses (Delivery-Only Retailers, Consumption Lounges and Retail Storefront Microbusinesses1), and modify development standards and signage requirements for existing uses. The proposed ordinances were reviewed by the Cannabis Commission (CC) and the Community Health Commission (CHC). -

Model Healthy Beverage Vending Agreement
Butte County Public Health Department Note Because of limited data available on the safety of high potency Cannabis Products, the Butte County Public Health Department recommends that retailers not be allowed to carry Cannabis Products with THC content in excess of 20%. This is the one recommendation that is different from the original ordinance created by Public Health Institute. Authors Support - Lynn Silver, MD, MPH, Public Health Institute - Alisa Padon, PhD, Public Health Institute Contributors - Ted Mermin, JD - Leslie Zellers, JD - Immigrant Legal Resources Center - James Mosher, JD Getting it Right from the Start A project of the Public Health Institute 555 12th Street, Oakland, CA 94607 www.gettingitrightfromthestart.org Telephone: 510.285.5648 Fax: 510.285.5501 Email: [email protected] Acknowledgement This Model Ordinance was adapted in part from ChangeLab Solutions and the California Department of Public Health’s Model Tobacco Retail License Ordinance and “plug-ins,” which have been adopted by cities and counties across the State of California. We acknowledge and appreciate their important contributions, although they are not responsible for the content. We also thank the many individuals who contributed interview time and comments during the development process. Note The legal information provided in this model ordinance does not constitute legal advice or legal representation. For legal advice, readers should consult an attorney in their state. Table of Contents Introduction ...................................................................................................................... -

Blunts and Blowt Jes: Cannabis Use Practices in Two Cultural Settings
Free Inquiry In Creative Sociology Volume 31 No. 1 May 2003 3 BLUNTS AND BLOWTJES: CANNABIS USE PRACTICES IN TWO CULTURAL SETTINGS AND THEIR IMPLICATIONS FOR SECONDARY PREVENTION Stephen J. Sifaneck, Institute for Special Populations Research, National Development & Research Institutes, Inc. Charles D. Kaplan, Limburg University, Maastricht, The Netherlands. Eloise Dunlap, Institute for Special Populations Research, NDRI. and Bruce D. Johnson, Institute for Special Populations Research, NDRI. ABSTRACT Thi s paper explores two modes of cannabis preparati on and smoking whic h have manifested within the dru g subcultures of th e United States and the Netherlan ds. Smoking "blunts," or hollowed out cigar wrappers fill ed wi th marijuana, is a phenomenon whi ch fi rst emerged in New York Ci ty in the mid 1980s, and has since spread throughout th e United States. A "bl owtj e," (pronounced "blowt-cha") a modern Dutch style j oint whi ch is mixed with tobacco and in cludes a card-board fi lte r and a longer rolling paper, has become th e standard mode of cannabis smoking in the Netherl ands as well as much of Europe. Both are consid ered newer than the more traditi onal practi ces of preparin g and smoking cannabis, including the traditional fi lter-less style joint, the pot pipe, an d the bong or water pipe. These newer styles of preparati on and smoking have implications for secondary preventi on efforts wi th ac tive youn g cannabis users. On a social and ritualistic level th ese practices serve as a means of self-regulating cannabi s use. -

Citizen Science: Framing the Public, Information Exchange, and Communication in Crowdsourced Science
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 8-2014 Citizen Science: Framing the Public, Information Exchange, and Communication in Crowdsourced Science Todd Ernest Suomela University of Tennessee - Knoxville, [email protected] Follow this and additional works at: https://trace.tennessee.edu/utk_graddiss Part of the Communication Commons, and the Library and Information Science Commons Recommended Citation Suomela, Todd Ernest, "Citizen Science: Framing the Public, Information Exchange, and Communication in Crowdsourced Science. " PhD diss., University of Tennessee, 2014. https://trace.tennessee.edu/utk_graddiss/2864 This Dissertation is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a dissertation written by Todd Ernest Suomela entitled "Citizen Science: Framing the Public, Information Exchange, and Communication in Crowdsourced Science." I have examined the final electronic copy of this dissertation for form and content and recommend that it be accepted in partial fulfillment of the equirr ements for the degree of Doctor of Philosophy, with a major in Communication and Information. Suzie Allard, Major Professor We have read this dissertation and recommend its acceptance: Carol Tenopir, Mark Littmann, Harry Dahms Accepted for the Council: Carolyn R. Hodges Vice Provost and Dean of the Graduate School (Original signatures are on file with official studentecor r ds.) Citizen Science: Framing the Public, Information Exchange, and Communication in Crowdsourced Science ADissertationPresentedforthe Doctor of Philosophy Degree The University of Tennessee, Knoxville Todd Ernest Suomela August 2014 c by Todd Ernest Suomela, 2014 All Rights Reserved. -

Personal Autonomy and Informed Consent: Conceptual and Normative Analyses
Personal Autonomy and Informed Consent: Conceptual and Normative Analyses Jesper Ahlin Licentiate thesis in philosophy KTH Royal Institute of Technology Stockholm, «Ï; © «Ï; Ahlin All rights reserved. Ahlin, J. Personal Autonomy and Informed Consent:Conceptual and Normative Analyses Licentiate thesis KTH Royal Institute of Technology TOC ;Ê-Ï-;;-- TOO ÏE«-ÊÊtÏ Typeset by the author, with help from Jesper Jerkert, using LATEX and BTCTEX.Printed by Universitetsservice US-AB, Drottning Kristinas väg tB, ÏÏ Ê Stockholm. I know what I know Acknowledgments I am grateful to Barbro Fröding, Sven Ove Hansson, and Niklas Juth for their su- pervision of this thesis, and to Gert Helgesson for his many useful comments on an earlier dra. Also, I thank William Bülow, Jesper Jerkert,Björn Lundgren, Payam Moula, and Maria Nordström, among others, for support and stimulating discussions. My thanks are extended to the Higher seminar at the Division of Philosophy, KTH Royal Institute of Technology, the Higher seminar at the Centre for Healthcare Ethics, Karolinska Institutet, and the VR/FORTE research program for providing opportu- nities to discuss and develop these ideas. All errors and mistakes are of course my own. his research was supported by the Swedish Research Council (VR) and the Swedish Research Council for Health, Working Life and Welfare (FORTE), contract no. «Ï– «, for the project Addressing Ethical Obstacles to Person Centred Care. Stockholm,August «Ï; Jesper Ahlin Abstract his licentiate thesis is comprised of a “kappa” and two articles. he kappa includes an account of personal autonomy and informed consent, an explanation of how the concepts and articles relate to each other, and a summary in Swedish.