Fraser Health Info Package Hhs.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Facility Funding Tiers
Facility Funding Tiers Funding # Acute Full Funding Start-Up Health Facility/Hospital Tiers Care Beds per Year Funding Authority Tier 6 – 9 Facilities ** 301+ $500 000 $75 000 FHA Burnaby Hospital PHSA Children’s and Women’s Hospital and Care Centre IHA Kelowna General Hospital VIHA Nanaimo Regional General Hospital FHA Royal Columbian & Eagle Ridge Hospitals VIHA Royal Jubilee & Victoria General Hospitals VCH St. Paul’s and Mount Saint Joseph Hospitals FHA Surrey Memorial Hospital NOTE: VGH $850,000 VCH Vancouver General & UBC Hospitals & GF Strong Tier 5 – 10 Facilities ** 151 to 300 $400 000 $75 000 FHA Abbotsford Regional Hospital and Cancer Centre PHSA BC Cancer Agency FHA Langley Memorial Hospital VCH Lions Gate Hospital FHA Peace Arch District Hospital VCH Richmond Hospital FHA Ridge Meadows Hospital and Health Care Centre IHA Royal Inland Hospital and Hillside Psychiatric NHA University Hospital of Northern BC IHA Vernon Jubilee Hospital Tier 4 – 5 Facilities ** 101 to 150 $300 000 $75 000 FHA Chilliwack General Hospital VIHA Cowichan District Hospital PHSA Forensic Psychiatric Services VIHA North Island Hospital Comox Valley (St. Joseph's Hospital) IHA Penticton Regional Hospital Tier 3 – 7 Facilities ** 51 to 100 $200 000 $35 000* PHSA BC Centre for Disease Control FHA Delta Hospital IHA East Kootenay Regional Hospital IHA Kootenay Boundary Regional Hospital VIHA North Island Hospital Campbell River (Campbell River District General Hospital) VIHA Saanich Peninsula Hospital Tier 2 – 13 Facilities ** 21 to 50 $150 000 $35 000* -
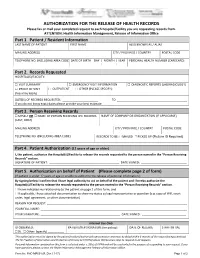
AUTHORIZATION for the RELEASE of HEALTH RECORDS Please Fax Or Mail Your Completed Request to Each Hospital/Facility You Are Requesting Records From
AUTHORIZATION FOR THE RELEASE OF HEALTH RECORDS Please fax or mail your completed request to each hospital/facility you are requesting records from. ATTENTION: Health Information Management, Release of Information Office Part 1. Patient / Resident Information LAST NAME OF PATIENT FIRST NAME ALSO KNOWN AS / ALIAS MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) DATE OF BIRTH DAY | MONTH | YEAR PERSONAL HEALTH NUMBER (CARECARD) | | Part 2. Records Requested HOSPITAL(S)/FACILITY: □ VISIT SUMMARY □ EMERGENCY VISIT INFORMATION □ DIAGNOSTIC REPORTS (LAB/RADIOLOGY) □ PROOF OF VISIT □ OUTPATIENT □ OTHER (PLEASE SPECIFY): (fees may apply) DATE(S) OF RECORDS REQUESTED: ______________________ TO ___________________________________________ If you do not know exact dates please provide your best estimate Part 3. Person Receiving Records □ MYSELF OR □ NAME OF PERSON RECEIVING THE RECORDS NAME OF COMPANY OR ORGANIZATION (IF APPLICABLE) (LAST, FIRST) MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) RECORDS TO BE: □ MAILED □ PICKED UP (Picture ID Required) Part 4. Patient Authorization (12 years of age or older) I, the patient, authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. SIGNATURE OF PATIENT: ___________________________________________ DATE SIGNED: ____________________________ Part 5. Authorization on behalf of Patient (Please complete page 2 of form) (If patient is under 12 years of age or unable to authorize the release of personal information.) By signing below I confirm that I have legal authority to act on behalf of the patient and I hereby authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. -

Climate Resilience Feasibility Study of Facilities at Fraser Canyon Hospital
Climate Resilience Feasibility Study of Facilities at Fraser Canyon Hospital Michal Bartko and Iain Macdonald A1-010678.2 29 September 2017 Climate Resilience Feasibility Study of Buildings at Fraser Canyon Hospital Author Michal Bartko, Ph.D. Research Officer Approved Trevor Nightingale, P.D. Program Leader, High Performance Buildings, NRC Construction Report No: A1-010678.2 Report Date: 29 September 2017 Contract No: A1-010678 Agreement date: 16 December 2016 Program: High Performance Buildings 26 pages Copy no. 1 of 4 This report may not be reproduced in whole or in part without the written consent of the National Research Council Canada and the Client. CLIMATE RESILIENCE FEASIBILITY STUDY OF FACILITIES AT FRASER CANYON HOSPITAL Table of Contents List of Figures ............................................................................................................................. v List of Tables .............................................................................................................................. v Executive Summary .................................................................................................................. vii 2. Introduction ............................................................................................................................ 1 2.1 Methodology ........................................................................................................................ 2 2.2 Fraser Canyon Hospital, Hope ............................................................................................ -

Births by Facility 2015/16
Number of Births by Facility British Columbia Maternal Discharges from April 1, 2015 to March 31, 2016 Ü Number of births: Fort Nelson* <10 10 - 49 50 - 249 250 - 499 500 - 999 Fort St. John 1,000 - 1,499 Wrinch Dawson Creek 1,500 - 2,499 Memorial* & District Mills Chetwynd * ≥ 2,500 Memorial Bulkley Valley MacKenzie & 1,500-2,499 Stuart Lake Northern Prince Rupert District * Births at home with a Haida Gwaii* University Hospital Registered Healthcare Provider of Northern BC Kitimat McBride* St. John G.R. Baker Memorial Haida Gwaii Shuswap Lake General 100 Mile District Queen Victoria Lower Mainland Inset: Cariboo Memorial Port Golden & District McNeill Lions Gate Royal Invermere St. Paul's Cormorant Inland & District Port Hardy * Island* Lillooet Ridge Meadows Powell River Vernon VGH* Campbell River Sechelt Kootenay Elk Valley Burnaby Lake Squamish Kelowna St. Joseph's General BC Women's General Surrey Penticton Memorial West Coast East Kootenay Abbotsford Royal General Regional Richmond Columbian Regional Fraser Creston Valley Tofino Canyon * Peace Langley Nicola General* Boundary* Kootenay Boundary Arch Memorial Nanaimo Lady Minto / Chilliwack Valley * Regional Gulf Islands General Cowichan Saanich District Victoria 0 62.5 125 250 375 500 Peninsula* General Kilometers * Hospital does not offer planned obstetrical services. Source: BC Perinatal Data Registry. Data generated on March 24, 2017 (from data as of March 8, 2017). Number of Births by Facility British Columbia, April 1, 2015 - March 31, 2016 Facility Community Births 100 Mile -

Trauma Services BC a Service of the Provincial Health Services Authority Contents
2015 ANNUAL REPORT Trauma Services BC A service of the Provincial Health Services Authority Contents 3 Foreword 4 Overview 5 BC’s system of organized trauma care 6 Trauma Services BC 7 Vision for BC’s trauma system 8 Governance 9 Trauma Services BC council 10 Strategic plan (2014-2016) 11 Partnerships & collaborations 12 BC Trauma Registry 13 Overview 14 Registry data quality monitoring 15 BC Trauma Registry operations 16 Key achievements 17 Future plans 18 Mechanism of Injury – Provincial overview 19 Regional health authority and partners trauma program report 20 Fraser Health 22 Interior Health 24 Island Health 26 Northern Health 28 Vancouver Coastal Health 30 BC Children’s Hospital 32 Special initiatives 33 Specialist Services Committee Project 34 Performance monitoring & evaluation plan 36 Accreditation Canada Trauma Distinction program 38 Looking forward 40 References and photo credits 42 Appendices 43 Appendix 1 – Inclusion/exclusion criteria for the BC Trauma Registry 44 Appendix 2 – Data quality 46 Appendix 3 – BC trauma program membership Foreword The 2015 annual report describes events and activities Our editor “in-situ” Mr. Beide Bekele, Trauma Services that took place within the calendar year supported by BC’s project manager, who discretely pushed us data from 2013/14. 2015 has been an exciting year of on timelines, content and continuity while working acquisition and building infrastructure for Trauma Services with our graphic artist, Mr. Ernest Stelzer, and PHSA BC with a strategic focus on advancing: communications, all of whom contributed to the look • Optimal service delivery for BC residents reflected in and tone of the report. -
Trauma Distinction Report
Trauma Distinction Report . Fraser Health Authority Surrey, BC On-site Survey Dates: May 15, 2016 - May 19, 2016 Report Issued: July 6, 2016 Distinction About the Distinction Report Fraser Health Authority (referred to in this report as “the organization”) is participating in the Accreditation Canada Distinction program. As part of this ongoing process of quality improvement, an on-site survey was conducted. Information from the on-site survey as well as other data obtained from the organization were used to produce this Distinction Report. On-site survey results are based on information provided by the organization. Accreditation Canada relies on the accuracy of this information to plan and conduct the on-site survey and produce the Distinction Report. Confidentiality This report is confidential and is provided by Accreditation Canada to the organization only. Accreditation Canada does not release the report to any other parties. In the interests of transparency and accountability, Accreditation Canada encourages the organization to disseminate its Distinction Report to staff, board members, clients, the community, and other stakeholders. Any alteration of this Distinction Report compromises the integrity of the process and is strictly prohibited. © Accreditation Canada, 2016 Distinction A Message from Accreditation Canada On behalf of Accreditation Canada, I extend my congratulations to Fraser Health Authority on your participation in a program that recognizes organizations that demonstrate clinical excellence and an outstanding commitment to leadership. I hope you find the Distinction process to be an interesting and informative experience, and that it is providing valuable information that you are using to plan your quality and safety initiatives. -

Pacs Opinion Survey: Referring Physicians
PACS OPINION SURVEY: REFERRING PHYSICIANS As a user of PACS, your opinion on PACS would be greatly appreciated in the PACS Opinion survey. This survey has been designed by Canada Health Infoway with the input of radiology experts. The purpose of this survey is to gather your opinion on the impact PACS has had on image access, patient care, patient transfers, duplicate tests, productivity, report turnaround time, etc. The results from many project sites across Canada will be used to develop a national view of the state of the diagnostic imaging environment since the implementation of PACS. Information that is obtained during this survey will be kept confidential to the full extent permitted by the law. You will not be identified by name in any reports of the completed survey; your responses will only be analyzed in aggregate by Canada Health Infoway or a third party that has been contracted for analysis. All identifiers in the records of data will be removed. Records of the data, identifying participants by code number only, will be stored on a fire-wall protected server and protected by password. Only authorized users will have access. Your opinion on the impact of this technology is important as it will assist in the measurement of the “actual” benefits created by technologies that are implemented to improve timely access to patient results and to establish the shared electronic patient record. INSTRUCTIONS The survey should take about 5-10 minutes to complete. Please return the survey in the enclosed envelope by Friday, March 3rd, 2006. If you have any questions about the survey please contact Nancy Kraetschmer at Canada Health Infoway at (416) 595-3164 or [email protected] 1. -

Pacs Opinion Survey: Radiologists
PACS OPINION SURVEY: RADIOLOGISTS As a user of PACS, your opinion on PACS would be greatly appreciated in the PACS Opinion survey. This survey has been designed by Canada Health Infoway with the input of radiology experts. The purpose of this survey is to gather your opinion on the impact PACS has had on image access, patient care, patient transfers, duplicate tests, productivity, report turnaround time, etc. The results from many project sites across Canada will be used to develop a national view of the state of the diagnostic imaging environment since the implementation of PACS. Information that is obtained during this survey will be kept confidential to the full extent permitted by the law. You will not be identified by name in any reports of the completed survey; your responses will only be analyzed in aggregate by Canada Health Infoway or a third party that has been contracted for analysis. All identifiers in the records of data will be removed. Records of the data, identifying participants by code number only, will be stored on a fire-wall protected server and protected by password. Only authorized users will have access. Your opinion on the impact of this technology is important as it will assist in the measurement of the “actual” benefits created by technologies that are implemented to improve timely access to patient results and to establish the shared electronic patient record. INSTRUCTIONS The survey should take about 5-10 minutes to complete. Please return the survey in the enclosed envelope by Friday, March 3rd, 2006. If you have any questions about the survey please contact Nancy Kraetschmer at Canada Health Infoway at (416) 595-3164 or [email protected] 1. -

Diagnostic Imaging
DIAGNOSTIC ACCREDITATION PROGRAM College of Physicians and Surgeons of British Columbia 300–669 Howe Street Telephone: 604-733-7758 Vancouver BC V6C 0B4 Toll free: 1-800-461-3008 (in BC) www.cpsbc.ca Fax: 604-733-3503 Accredited Facilities – Diagnostic Imaging As of 2021-09-20 Facility Name Address Scope of Expiry Date Organization Medical Director Accreditation of Accreditation 100 Mile District General Hospital 555 Cedar Drive Radiology 2023-04-19 Interior Health Authority Dr. Vipal Vedd 100 Mile House, BC, V0K 2E0 Abbotsford MRI Clinic Suite 5 - 2151 McCallum Road Magnetic Resonance 2024-09-04 Fraser Health Authority Dr. Amarjit Bajwa Abbotsford, BC, V2S 3N8 Imaging Abbotsford Regional Hospital and 32900 Marshall Road Radiology, Ultrasound, 2024-02-27 Fraser Health Authority Dr. Amarjit Bajwa Cancer Centre Abbotsford, BC, V2S 1K2 Computed Tomography, Nuclear Medicine, Mammography, Echocardiography, Magnetic Resonance Imaging, Bone Densitometry Abbotsford Regional Hospital and 32900 Marshall Road Vascular Ultrasound - 2025-12-17 Fraser Health Authority Dr. Husain Khambati Cancer Centre - Vascular Lab Abbotsford, BC, V2S 0C2 Limited Scope Aberdeen Ultrasound and X-Ray 272 - 1320 W. Trans Canada Hwy Radiology, Ultrasound 2025-02-05 Aberdeen Ultrasound Dr. Micheal Burns Kamloops, BC, V1S 1J2 and X-Ray Access MRI 104 - 15137 56 Avenue Magnetic Resonance 2026-02-10 Access MRI Dr. Spencer Lister Surrey, BC, V3S 9A5 Imaging, Ultrasound, Echocardiography AIM Medical Imaging Inc. 1371 West Broadway Magnetic Resonance 2024-10-24 AIM Medical Imaging Dr. Raj Attariwala Vancouver, BC, V6H 1G9 Imaging Inc. Arrow Lakes Hospital 97 1st Avenue NE Radiology 2023-04-10 Interior Health Authority Dr. -
Patient's Rights Workshop Kit
Vancouver Women's Health Co litiue 1 - 175 East 15th Avenue, Vancouver, BC V5T 2P6 Tel (604) 736-4234 Fax (604) 876-1282 wvhc@vcn. bc.ca Health Information Line (604) 736-5262 Community Health Advocate Project CHA is an ozitr~?achproJctthat educates women abotct their righs wt'thin the health care system Women .peaking orn/for sap, npcfi&and appropriate health care for women Patient's Rights Workshop Kit Table Of Contents: WCMission Statement .............................................................. -................................... .. ........................................................................ 1 A Woman>sBill of Rights ...... -........................................................................................................ ..... " ..- ... ............. ..- ....................... .......- 2 Things to Consider Before you Start your Search ....................................................................................................... 3 What to Expect from a Health Care Practitioner .................................................................................................... 4 . What to Expect from a Physical Exmation........................................................................................................................ 4 , Questions to Ask about Diagnosis/Treatment .................................................................................................................. 5 A Visit to the Doctor's Offlce .................................................................................................. -

Please Fax Or Mail Your Request to Each Hospital/Facility You Are Requesting Records from Attention: Health Information Management, Release of Information Office
PLEASE FAX OR MAIL YOUR REQUEST TO EACH HOSPITAL/FACILITY YOU ARE REQUESTING RECORDS FROM ATTENTION: HEALTH INFORMATION MANAGEMENT, RELEASE OF INFORMATION OFFICE Abbotsford Regional Hospital Forensic Psychiatric Hospital 32900 Marshall Rd, Abbotsford, BC V2S 0C2 70 Colony Farm Rd, Coquitlam, BC V3C 5X9 Fax: (604) 851‐4902 Tel: (604) 851‐4700, Ext 646790 Fax: (604) 523‐7897 Tel: (604) 524‐7732 BC Children’s Hospital and BC Women’s Hospital Fraser Canyon Hospital 4500 Oak St, Vancouver, BC V6H 3V5 1275 7 Ave, Hope, BC V0X 1L4 Fax: (604) 875‐2662 Tel: (604) 875‐3450 Fax: (604) 860‐7710 Tel: (604) 860‐7729 BCCA – Abbotsford GF Strong Rehab Centre 32900 Marshall Rd, Abbotsford, BC V2S 0C2 4255 Laurel St, Vancouver, BC V5Z 2G9 Fax: (604) 851‐4738 Tel: (604) 851‐4710, Ext 645176 Fax: (604) 731‐5091 Tel: (604) 714‐4158 BCCA – Fraser Valley Holy Family Hospital (c/o St. Paul’s Hospital) 13750 96 Ave, Surrey, BC V3V 1Z2 1081 Burrard St, Vancouver, BC V6Z 1Y6 Fax: (604) 930‐4096 Tel: (604) 930‐4073 Fax: (604) 806‐9015 Tel: (604) 806‐8099 BCCA – Kelowna Langley Memorial Hospital 399 Royal Ave, Kelowna, BC V1Y 5L3 22051 Fraser Hwy, Langley, BC V3A 4H4 Fax: (250) 712‐3977 Tel: (250) 712‐3900 Fax: (604) 533‐6458 Tel: (604) 534‐4121, Ext 745272 If your last name starts with A‐L, Ext 686822 If your last name starts with M‐Z, Ext 686814 Lion’s Gate Hospital 231 E. 15th St, North Vancouver, BC V7L 2L7 BCCA – Prince George Fax: (604)984‐5718 Tel: (604) 984‐5719 1215 Lethbridge St, Prince George, BC V2M 7E9 Fax: (250) 645‐7366 Tel: (250) 645‐7316 Mission Memorial Hospital 7324 Hurd St, Mission, BC V2V 3H5 BCCA – Vancouver Fax: (604) 826‐4043 Tel: (604) 814‐5166 600 W. -
Fraser Health Research
Researchers By Geographical Area And Specialty C G.M. Johnson (604)-299-7074 Fraser ASE Community CanyonFR Research Hospital Hope 1 1 Harrison Mental Health Hot Springs Nursing Human Resources Mental Health Palliative Care Port Eagle Ridge Moody Hospital Multiple Sclerosis Maple District of Kent Palliative Care 1 Burnaby Ridge Gerontology: Falls Port Burnaby Coquitlam Coquitlam Psychiatry Agassiz Hospital Pitt Ridge Meadows Mission Meadows Hospital New Royal Westminster Columbiania Gerontology FRASER RIVER Anesthesia Pharmacy Chilliwack General Cardiology Hospital Mission Critical Care 1 Hospital ER Memorial 1 Emergency Medicine Surrey FRASERRIV Gastroenterology Hospital Nephrology Memorial Neurology Anesthesia Hospital Cardiac Surgical Care Delta Emergency Medicine Nutrition Cardiology Surrey Obstetrics/Gynecology Gastroenterology City of Active Oncology Nephrology Langley Langley Abbotsford Research Sites Orthopaedic Delta Obstetrical Nursing 1 PaediatricsPeadiatrics Obstetrics/Gynecology Memorial Mental Health Hospital Paediatrics Hospital 0 246810 Pharmacy Psychology 1 MILE Respiratory South Surrey KILOMETRE Hip Fractures: Falls Prevention District of Gastroenterology 0 4 8 12 16 White Peace Arch Hip Fractures: Length of Stay Langley Respiratory MSA Hospital Psychiatry Rock Hospital Pharmacy C G.M. Johnson (604)-299-7074 Respiratory Eagle Ridge Hospital / Tri-Cities Ridge Meadows Hospital / Maple Ridge and Pitt Meadows Fraser Canyon Hospital / Hope and Agassiz Burnaby Hospital / Burnaby Mission Memorial Hospital / Mission Chillliwack General Hospital / Chilliwack Royal Columbian Hospital / New Westminster Langley Memorial Hospital / Langley Surrey Memorial Hospital / Surrey MSA Hospital / Abbotsford Delta Hospital / Delta Peace Arch Hospital / White Rock and South Surrey.