Trauma Services BC a Service of the Provincial Health Services Authority Contents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Facility Funding Tiers
Facility Funding Tiers Funding # Acute Full Funding Start-Up Health Facility/Hospital Tiers Care Beds per Year Funding Authority Tier 6 – 9 Facilities ** 301+ $500 000 $75 000 FHA Burnaby Hospital PHSA Children’s and Women’s Hospital and Care Centre IHA Kelowna General Hospital VIHA Nanaimo Regional General Hospital FHA Royal Columbian & Eagle Ridge Hospitals VIHA Royal Jubilee & Victoria General Hospitals VCH St. Paul’s and Mount Saint Joseph Hospitals FHA Surrey Memorial Hospital NOTE: VGH $850,000 VCH Vancouver General & UBC Hospitals & GF Strong Tier 5 – 10 Facilities ** 151 to 300 $400 000 $75 000 FHA Abbotsford Regional Hospital and Cancer Centre PHSA BC Cancer Agency FHA Langley Memorial Hospital VCH Lions Gate Hospital FHA Peace Arch District Hospital VCH Richmond Hospital FHA Ridge Meadows Hospital and Health Care Centre IHA Royal Inland Hospital and Hillside Psychiatric NHA University Hospital of Northern BC IHA Vernon Jubilee Hospital Tier 4 – 5 Facilities ** 101 to 150 $300 000 $75 000 FHA Chilliwack General Hospital VIHA Cowichan District Hospital PHSA Forensic Psychiatric Services VIHA North Island Hospital Comox Valley (St. Joseph's Hospital) IHA Penticton Regional Hospital Tier 3 – 7 Facilities ** 51 to 100 $200 000 $35 000* PHSA BC Centre for Disease Control FHA Delta Hospital IHA East Kootenay Regional Hospital IHA Kootenay Boundary Regional Hospital VIHA North Island Hospital Campbell River (Campbell River District General Hospital) VIHA Saanich Peninsula Hospital Tier 2 – 13 Facilities ** 21 to 50 $150 000 $35 000* -
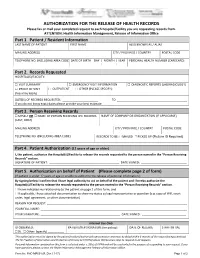
AUTHORIZATION for the RELEASE of HEALTH RECORDS Please Fax Or Mail Your Completed Request to Each Hospital/Facility You Are Requesting Records From
AUTHORIZATION FOR THE RELEASE OF HEALTH RECORDS Please fax or mail your completed request to each hospital/facility you are requesting records from. ATTENTION: Health Information Management, Release of Information Office Part 1. Patient / Resident Information LAST NAME OF PATIENT FIRST NAME ALSO KNOWN AS / ALIAS MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) DATE OF BIRTH DAY | MONTH | YEAR PERSONAL HEALTH NUMBER (CARECARD) | | Part 2. Records Requested HOSPITAL(S)/FACILITY: □ VISIT SUMMARY □ EMERGENCY VISIT INFORMATION □ DIAGNOSTIC REPORTS (LAB/RADIOLOGY) □ PROOF OF VISIT □ OUTPATIENT □ OTHER (PLEASE SPECIFY): (fees may apply) DATE(S) OF RECORDS REQUESTED: ______________________ TO ___________________________________________ If you do not know exact dates please provide your best estimate Part 3. Person Receiving Records □ MYSELF OR □ NAME OF PERSON RECEIVING THE RECORDS NAME OF COMPANY OR ORGANIZATION (IF APPLICABLE) (LAST, FIRST) MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) RECORDS TO BE: □ MAILED □ PICKED UP (Picture ID Required) Part 4. Patient Authorization (12 years of age or older) I, the patient, authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. SIGNATURE OF PATIENT: ___________________________________________ DATE SIGNED: ____________________________ Part 5. Authorization on behalf of Patient (Please complete page 2 of form) (If patient is under 12 years of age or unable to authorize the release of personal information.) By signing below I confirm that I have legal authority to act on behalf of the patient and I hereby authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. -

Schedule of Suppliers and Goods Or Services 2017
Financial Information Act Schedule of Suppliers of Goods or Services For the Year Ending March 31, 2017 Vendor Amount 0691913 BC LTD. DBA WE CARE HOME HEALTH SERVICES 565,566 0697790 BC LTD. 3,917,300 0710395 BC LTD. 343,432 0902488 BC LTD 503,468 100 MILE DISTRICT HOSPICE PALLIATIVE CARE SOCIETY 31,273 100 MILE HOUSE,DISTRICT OF 148,519 1022117 ALBERTA LTD 104,410 3M CANADA COMPANY 100,011 4REFUEL CANADA LP 76,957 517244 BC LTD 39,506 556216 BC LTD. DBA WE CARE HOME HEALTH SERVICES 1,352,280 617036 BC LTD. 288,524 673848 BC LTD. 268,302 679692 BC LTD 130,670 A & D WHOLESALE LTD 71,834 A & G SUPPLY LTD 27,339 A & T PROJECT DEVELOPMENTS INC 1,169,467 A.C.M.C.J. HOLDINGS LTD. 7,520,952 ABBOTT DIAGNOSTICS DIVISION MIS 558,350 ABBOTT VASCULAR DIVISION 461,388 ABBVIE 814,006 ABIOMED INC 31,777 AC MOTOR ELECTRIC LTD 25,617 ACART EQUIPMENT LTD 168,522 ACCREDITATION CANADA 520,675 ACKLANDS GRAINGER INC 100,143 ACME VISIBLE FILING SYSTEMS LTD 33,739 ACTION CONTRACTING 260,565 ACTION DATA COMMUNICATION LTD 110,259 ACTIVE MEDICAL EQUIPMENT 113,467 ADAM EHRLER, IN HIS CAPACITY AS THE REPRESENTATIVE OF LARRY EHRLER 60,359 ADVANCED MOBILITY PRODUCTS LTD 37,111 ADVANCED SOFTWARE 208,533 ADVANCED SURGI-PHARM INC 32,309 AES ENGINEERING LTD 41,486 AGI ENVIRO TANK 28,235 AGING WITH EASE IN RURAL COMMUNITIES (AWE) SOCIETY 56,432 AGROPUR,DIVISION OF NATREL 924,161 AL STOBER CONSTRUCTION LTD 1,217,387 ALCON CANADA INC 2,111,925 ALERE INC 773,330 ALEXANDER HOLBURN BEAUDIN & LANG 33,967 ALLAN ORR 81,197 ALLERGAN INC PHARM 67,959 ALLIANCE OFFICE FURNITURE 27,616 -

Climate Resilience Feasibility Study of Facilities at Fraser Canyon Hospital
Climate Resilience Feasibility Study of Facilities at Fraser Canyon Hospital Michal Bartko and Iain Macdonald A1-010678.2 29 September 2017 Climate Resilience Feasibility Study of Buildings at Fraser Canyon Hospital Author Michal Bartko, Ph.D. Research Officer Approved Trevor Nightingale, P.D. Program Leader, High Performance Buildings, NRC Construction Report No: A1-010678.2 Report Date: 29 September 2017 Contract No: A1-010678 Agreement date: 16 December 2016 Program: High Performance Buildings 26 pages Copy no. 1 of 4 This report may not be reproduced in whole or in part without the written consent of the National Research Council Canada and the Client. CLIMATE RESILIENCE FEASIBILITY STUDY OF FACILITIES AT FRASER CANYON HOSPITAL Table of Contents List of Figures ............................................................................................................................. v List of Tables .............................................................................................................................. v Executive Summary .................................................................................................................. vii 2. Introduction ............................................................................................................................ 1 2.1 Methodology ........................................................................................................................ 2 2.2 Fraser Canyon Hospital, Hope ............................................................................................ -

Queen Charlotte/Haida Gwaii General Hospital
Director’s Tool Kit 2015 North West Regional Hospital District Building for Health Execuve Director Yvonne Koerner Suite 300 ‐ 4545 Lazelle Avenue Terrace, BC V8G 4E1 Tel: 250‐615‐6100 Toll Free: 1‐800‐663‐3208 Fax: 250‐635‐9222 Email: [email protected] TABLE OF CONTENTS 2015 NWRHD Addresses and contact information Roster of Votes Directors and Alternates 2015 About the North West Regional Hospital District Procedure Bylaw 82 - Replaced Bylaw 67 Confidentiality and In-Camera Protocol Remuneration Bylaw 64 Director Remuneration/Expense Claim form UBCM 2014 Information Package Links to Medical Travel Assistance New Queen Charlotte / Haida Gwaii Hospital History – news releases and letters Memorandum of Understanding with Northern Health NH Glossary of Acronyms and Terms Hospital District Act Directors and Alternates (*) January 2015 REGIONAL DISTRICT OF BULKLEY-NECHAKO DIRECTOR *ALTERNATE AGENDA INSTRUCTIONS Representing: Town of Smithers Taylor Bachrach *Frank Wray Mail agenda to: PO Box 879 PO Box 512 Taylor Bachrach Smithers, BC V0J 2N0 Smithers, BC V0J 2N0 PO Box 879 Work 250-847-9298 Home: 250-778-210-0311 Smithers, BC V0J 2N0 Work 250-847-1600 Work: 250-847-2622 Cell 778-210-0877 [email protected] [email protected] Representing: Village of Telkwa Brad Layton *Darcy Repen c/o Village of Telkwa c/o Village of Telkwa Box 220 Box 220 Telkwa, BC V0J 2X0 Telkwa, BC V0J 2X0 Cell: 250-877-1344 [email protected] Work: 250-846-5060 [email protected] Representing: District of Houston Shane Brienen *Tim Anderson c/o District of Houston [email protected] Box 370 Houston, BC V0J 1Z0 Cell 250-845-8542 [email protected] Representing: Electoral Area A – Smithers Rural Mark Fisher * Email the digital agenda to 10668 Hislop Road [email protected], larger Telkwa, BC V0J 2X1 agendas may not go through and Home: 250-846-9045 Director Fisher should be [email protected] contacted for alternate arrangements. -

Births by Facility 2015/16
Number of Births by Facility British Columbia Maternal Discharges from April 1, 2015 to March 31, 2016 Ü Number of births: Fort Nelson* <10 10 - 49 50 - 249 250 - 499 500 - 999 Fort St. John 1,000 - 1,499 Wrinch Dawson Creek 1,500 - 2,499 Memorial* & District Mills Chetwynd * ≥ 2,500 Memorial Bulkley Valley MacKenzie & 1,500-2,499 Stuart Lake Northern Prince Rupert District * Births at home with a Haida Gwaii* University Hospital Registered Healthcare Provider of Northern BC Kitimat McBride* St. John G.R. Baker Memorial Haida Gwaii Shuswap Lake General 100 Mile District Queen Victoria Lower Mainland Inset: Cariboo Memorial Port Golden & District McNeill Lions Gate Royal Invermere St. Paul's Cormorant Inland & District Port Hardy * Island* Lillooet Ridge Meadows Powell River Vernon VGH* Campbell River Sechelt Kootenay Elk Valley Burnaby Lake Squamish Kelowna St. Joseph's General BC Women's General Surrey Penticton Memorial West Coast East Kootenay Abbotsford Royal General Regional Richmond Columbian Regional Fraser Creston Valley Tofino Canyon * Peace Langley Nicola General* Boundary* Kootenay Boundary Arch Memorial Nanaimo Lady Minto / Chilliwack Valley * Regional Gulf Islands General Cowichan Saanich District Victoria 0 62.5 125 250 375 500 Peninsula* General Kilometers * Hospital does not offer planned obstetrical services. Source: BC Perinatal Data Registry. Data generated on March 24, 2017 (from data as of March 8, 2017). Number of Births by Facility British Columbia, April 1, 2015 - March 31, 2016 Facility Community Births 100 Mile -

Please Fax Or Mail Your Request to Each Hospital/Facility You Are Requesting Records from Attention: Health Information Management, Release of Information Office
PLEASE FAX OR MAIL YOUR REQUEST TO EACH HOSPITAL/FACILITY YOU ARE REQUESTING RECORDS FROM ATTENTION: HEALTH INFORMATION MANAGEMENT, RELEASE OF INFORMATION OFFICE Abbotsford Regional Hospital Eagle Ridge Hospital 32900 Marshall Rd, Abbotsford, BC V2S 0C2 475 Guildford Way, Port Moody, BC V3H 3W9 Fax: (604) 851-4902 Tel: (604) 851-4700, Ext 646790 Fax: (604) 469-3205 Tel: (604) 469-3239 BC Children’s Hospital and BC Women’s Hospital Forensic Psychiatric Hospital 4500 Oak St, Vancouver, BC V6H 3V5 70 Colony Farm Rd, Coquitlam, BC V3C 5X9 Fax: (604) 875-2292 Tel: (604) 875-2915 Fax: (604) 523-7897 Tel: (604) 524-7732 BC Women’s Health Centre Fraser Canyon Hospital F2-4500 Oak St, Vancouver, BC V6H 3N1 1275 7 Ave, Hope, BC V0X 1L4 Fax: (604) 875-3136 Tel: (604) 875-3669/3670 Fax: (604) 860-7716 Tel: (604) 860-7728 BCCA – Abbotsford GF Strong Rehab Centre 32900 Marshall Rd, Abbotsford, BC V2S 0C2 4255 Laurel St, Vancouver, BC V5Z 2G9 Fax: (604) 851-4738 Tel: (604) 851-4710, Ext 645176 Fax: (604) 731-5091 Tel: (604) 714-4158 BCCA – Fraser Valley Holy Family Hospital (c/o St. Paul’s Hospital) 13750 96 Ave, Surrey, BC V3V 1Z2 1081 Burrard St, Vancouver, BC V6Z 1Y6 Fax: (604) 930-4096 Tel: (604) 930-4073 Fax: (604) 806-9015 Tel: (604) 806-8099 BCCA – Kelowna Langley Memorial Hospital 399 Royal Ave, Kelowna, BC V1Y 5L3 22051 Fraser Hwy, Langley, BC V3A 4H4 Fax: (250) 712-3977 Tel: (250) 712-3900 Fax: (604) 533-6458 Tel: (604) 534-4121, Ext 745272 If your last name starts with A-L, Ext 686822 If your last name starts with M-Z, Ext 686814 Lion’s Gate Hospital 231 E. -

North Okanagan/Columbia Shuswap Regional Hospital District Present: Absent: Guests: Call to Order
NORTH OKANAGAN/COLUMBIA SHUSWAP REGIONAL HOSPITAL DISTRICT Minutes of a Regular meeting of the North Okanagan/Columbia Shuswap Regional Hospital District Board held October 25, 2016 in the Board Room of the ReQional District of North Okanaaan Note: The following minutes are subject to correction when endorsed by the Board at the next Regular meeting, PRESENT: R. Martin, Chair Area E, CSRD Directors: P. Demenok Area C, CSRD M. Macnabb Area C, RDNO R. Fairbairn Area D, RDNO H. Halvorson Area F, RDNO D. Dirk District of Coldstream, RDNO H. Cameron Area E, RDNO C. Eliason City of Salmon Arm, CSRD N. Cooper City of Salmon Arm, CSRD J. Brown Township of Spallumcheen, RDNO A. Mund CityofVernon,RDNO J. Cunningham CityofVernon,RDNO C. Lord CityofVernon,RDNO L. Parker Area B, CSRD H. Halvorson Area F, RDNO G. McCune City of Enderby, RDNO Staff: C. Hamilton Secretary L. Shykora Deputy Mgr., Corporate Admin. (Recorder) J. Pierce Manager, Financial Services ABSENT: S. Fowler City of Armstrong, RDNO K. Acton Village of Lumby, RDNO M. McKee City of Revelstoke, CSRD T. Rysz District of Sicamous, CSRD B. Quiring CityofVernon,RDNO B. Fleming Area B, RDNO GUESTS: P. du Toit Interior Health D. Gournough Interior Health K. Peters Interior Health CALL TO ORDER: Chair Martin called the meeting to order at 10:01 AM. NORTH OKANAGAN/COLUMBIA SHUSWAP HOSPITAL DISTRICT BOARD MEETING MINUTES October 25, 2016 ADOPTION OF MINUTES H2016-109 M/S Directors Cunningham/Macnabb THAT: ADOPTION OF the minutes of the March 22, 2016 North Okanagan/Columbia Shuswap MINUTES Regional Hospital District Board meeting be adopted. -

BCNU - EDMP Contact List
BCNU - EDMP Contact List Representative Region Sites Vancouver Coastal (VCHA) Dawn Tonge Coastal Mountain/ Richmond: Acute, Community & [email protected] RIVA Long-Term Care (Minoru, Lions Cell: 604 862 1063 Manor), Lions Gate Hospital, Sunshine Coast-Sechelt, Powell River, Whistler, Pemberton/ Squamish, Bella Bella, Bella Coola Silvia Kuntze Central Vancouver/ Vancouver Acute, UBC, TCU– [email protected] RIVA Koerner Pavilion, Mary Pack, Cell: 604 862 0186 Broadway Corporate Offices, CST, Tertiary Mental Health (Willow/Segal), Banfield Jaspreet Gill Central Vancouver/ Community Care, George [email protected] RIVA Pearson Centre, G.F. Strong Cell: 604 312 0826 Vancouver Island (VIHA) Elaine Greer South Islands Victoria (except RJH & Mental [email protected] Health), SPH, Lady Minto, PHS Cell: 250 889 0228 Holly Anderson Pacific Rim NRGH, Oceanside, Port Alberni [email protected] (except Westhaven), Tofino/ Cell: 250 713 8772 Ucleulet, Comox/Courtenay, Campbell River, Mt. Waddington Laura Rachwalski Pacific Rim/ RJH, Victoria Mental Health (all [email protected] South Islands sites & programs), Duncan, Cell: 250 893 1774 Chemainus, Ladysmith, Nanaimo (except NRGH), Trillium, Westhaven, Eagle Park Fraser Health (FHA) Nicole Ng Fraser Valley/ Ridge Meadows Hospital, ARH, [email protected] South Fraser Valley/ Abbotsford Community, Langley Cell: 604 785 7644 Simon Fraser Memorial Hospital, Langley Community, Cottage/Worthington October 2020 Representative Region Sites Cathy Ellen Queen South Fraser Valley Delta Hospital -

A Four-Year Picture
September 2005 Health Authority Redesign Accomplishments A Four-Year Picture Northern Health NORTHERN HEALTH Health Service Redesign British Columbia is planning a health care system where high quality health care is available to everyone – where services are timely, affordable and sustainable, for today and future generations. Since 2002, when government streamlined 52 health regions with competing or overlapping mandates into six health authorities, the province has been able to maximize the resources available for direct patient care. Five regional health authorities now have responsibility for planning and delivering local health services, such as public health, mental health, residential, home and hospital care. The Provincial Health Services Authority oversees provincial and highly-specialized health services, such as the BC Cancer Agency. A strong economy and sound fiscal management have enabled the province to increase health care spending by $3.8 billion between 2001 and 2007. Strategic investments, based on best practices and innovative approaches to local challenges, are improving health authorities’ ability to respond to patients’ needs. As British Columbia moves forward into the 21st century, lifestyle choices – in nutrition, physical activity, non-smoking and responsible use of alcohol – will be the foundation of keeping our population healthy and our health care system sustainable. Northern Health Northern Health provides a full range of health care services to approximately 297,0001 residents in northern British Columbia. It covers almost two-thirds of B.C., bordered by the Northwest and Yukon Territories, the B.C. interior, Alberta, Alaska and the Pacific Ocean. Northern Health employs 7,000 staff. Acute Care Services Health authorities and the Provincial Health Services Authority are designing a network of acute care that includes centres of excellence for specialized services and community hospitals or treatment centres for basic emergency services. -

Report to the Community Fiscal Period April 1, 2019 – March 31, 2020
REPORT TO THE COMMUNITY FISCAL PERIOD APRIL 1, 2019 – MARCH 31, 2020 ENHANCING HEALTH CARE SERVICES IN THE TRI-CITIES REGION THROUGH PHILANTHROPY & ADVOCACY. EXCEPTIONAL COMMUNITY | OUTSTANDING CARE TRANSFORMING COMMUNITY HEALTHCARE. WHEN YOU NEED US. LOCATION IS EVERYTHING. WITH YOUR SUPPORT. A MESSAGE FROM EAGLE RIDGE HOSPITAL FOUNDATION’S COMMUNITY OUTPATIENT SERVICES OPENS TO PATIENTS AT ERH EXECUTIVE DIRECTOR, CHARLENE GIOVANNETTI-KING What an incredible year it’s been for Eagle Ridge Hospital Foundation Community Outpatient Services (COS) is an integral part of our hospital – designed for the treatment and diagnosis (ERHF), thanks to you, our exceptional community of donors, sponsors of patients in four key areas: Wound Care, Rapid Access Clinics (i.e. Psychiatry, Infectious Disease, Neurology, Internal and volunteers – THANK YOU for your support! Medicine and Respiratory), IV Therapy (i.e. Iron, Blood and IVIG) and Medical Daycare. The increased demand for outpatient services at ERH, combined with the population growth in the Tri-Cities, highlighted the fact that the This past year was not only exciting, it was unique, especially in how former space housing COS was undersized and overcrowded. Given these patients often require regular visits to it ended. Some highlights from the year include the start of phase our hospital, their care and comfort is paramount. The new COS space at ERH has enabled increased efficiencies, one of construction on the expansion of Eagle Ridge Hospital (ERH). capacity and improved patient outcomes. With 50% more treatment spaces, patients receive quicker follow-up, close Work progressed quickly through the summer of 2019 and resulted in to home, rather than having to travel to see specialists, all with the goal of promoting better healing. -

NEWS RELEASE for Immediate Release Ministry of Health 2019HLTH0012-000050 Fraser Health Jan
NEWS RELEASE For Immediate Release Ministry of Health 2019HLTH0012-000050 Fraser Health Jan. 18, 2019 Work starts on new emergency department at Eagle Ridge Hospital PORT MOODY – Better emergency care for people in the Tri-Cities area is on the way as construction work begins on a new emergency department at Eagle Ridge Hospital. “Our government is making the investment for an expanded emergency department at Eagle Ridge Hospital that will meet the needs of the growing Tri-Cities population,” said Adrian Dix, Minister of Health. “We are treating emergency care in this region as a priority, so people will be able to receive health-care services in a state-of-the-art facility, and health-care workers will have the room they need to help patients get better, quicker.” The provincial government is investing $22.6 million through the regional health authority in the emergency department expansion. The Eagle Ridge Hospital Foundation is providing an additional $5 million. The prior plan for the project, announced March 29, 2017, left unresolved questions about the Province's share of the funding. The expansion will more than double the number of patient treatment spaces in the emergency department from 19 to 39. Construction is expected to be complete in late 2020. The work will include four new isolation rooms to support improved infection-control measures as well as two new trauma resuscitation bays. Walk-in patients and ambulances will have separate entrances. An area will be designated for chemical decontamination. When Eagle Ridge Hospital opened almost 35 years ago, the hospital’s emergency department had about 20,000 patient visits per year.