Virus Like Particle-Based Vaccines Against Emerging Infectious Disease Viruses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antiviral Bioactive Compounds of Mushrooms and Their Antiviral Mechanisms: a Review
viruses Review Antiviral Bioactive Compounds of Mushrooms and Their Antiviral Mechanisms: A Review Dong Joo Seo 1 and Changsun Choi 2,* 1 Department of Food Science and Nutrition, College of Health and Welfare and Education, Gwangju University 277 Hyodeok-ro, Nam-gu, Gwangju 61743, Korea; [email protected] 2 Department of Food and Nutrition, School of Food Science and Technology, College of Biotechnology and Natural Resources, Chung-Ang University, 4726 Seodongdaero, Daeduck-myun, Anseong-si, Gyeonggi-do 17546, Korea * Correspondence: [email protected]; Tel.: +82-31-670-4589; Fax: +82-31-676-8741 Abstract: Mushrooms are used in their natural form as a food supplement and food additive. In addition, several bioactive compounds beneficial for human health have been derived from mushrooms. Among them, polysaccharides, carbohydrate-binding protein, peptides, proteins, enzymes, polyphenols, triterpenes, triterpenoids, and several other compounds exert antiviral activity against DNA and RNA viruses. Their antiviral targets were mostly virus entry, viral genome replication, viral proteins, and cellular proteins and influenced immune modulation, which was evaluated through pre-, simultaneous-, co-, and post-treatment in vitro and in vivo studies. In particular, they treated and relieved the viral diseases caused by herpes simplex virus, influenza virus, and human immunodeficiency virus (HIV). Some mushroom compounds that act against HIV, influenza A virus, and hepatitis C virus showed antiviral effects comparable to those of antiviral drugs. Therefore, bioactive compounds from mushrooms could be candidates for treating viral infections. Citation: Seo, D.J.; Choi, C. Antiviral Bioactive Compounds of Mushrooms Keywords: mushroom; bioactive compound; virus; infection; antiviral mechanism and Their Antiviral Mechanisms: A Review. -

Guide for Common Viral Diseases of Animals in Louisiana
Sampling and Testing Guide for Common Viral Diseases of Animals in Louisiana Please click on the species of interest: Cattle Deer and Small Ruminants The Louisiana Animal Swine Disease Diagnostic Horses Laboratory Dogs A service unit of the LSU School of Veterinary Medicine Adapted from Murphy, F.A., et al, Veterinary Virology, 3rd ed. Cats Academic Press, 1999. Compiled by Rob Poston Multi-species: Rabiesvirus DCN LADDL Guide for Common Viral Diseases v. B2 1 Cattle Please click on the principle system involvement Generalized viral diseases Respiratory viral diseases Enteric viral diseases Reproductive/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 2 Deer and Small Ruminants Please click on the principle system involvement Generalized viral disease Respiratory viral disease Enteric viral diseases Reproductive/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 3 Swine Please click on the principle system involvement Generalized viral diseases Respiratory viral diseases Enteric viral diseases Reproductive/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 4 Horses Please click on the principle system involvement Generalized viral diseases Neurological viral diseases Respiratory viral diseases Enteric viral diseases Abortifacient/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 5 Dogs Please click on the principle system involvement Generalized viral diseases Respiratory viral diseases Enteric viral diseases Reproductive/neonatal viral diseases Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. -

Norovirus Infectious Agent Information Sheet
Norovirus Infectious Agent Information Sheet Introduction Noroviruses are non-enveloped (naked) RNA viruses with icosahedral nucleocapsid symmetry. The norovirus genome consists of (+) ssRNA, containing three open reading frames that encode for proteins required for transcription, replication, and assembly. There are five norovirus genogroups (GI-GV), and only GI, GII, and GIV infect humans. Norovirus belongs to the Caliciviridae family of viruses, and has had past names including, Norwalk virus and “winter-vomiting” disease. Epidemiology and Clinical Significance Noroviruses are considered the most common cause of outbreaks of non-bacterial gastroenteritis worldwide, are the leading cause of foodborne illness in the United States (58%), and account for 26% of hospitalizations and 10% of deaths associated with food consumption. Salad ingredients, fruit, and oysters are the most implicated in norovirus outbreaks. Aside from food and water, Noroviruses can also be transmitted by person to person contact and contact with environmental surfaces. The rapid spread of secondary infections occurs in areas where a large population is enclosed within a static environment, such as cruise ships, military bases, and institutions. Symptoms typically last for 24 to 48 hours, but can persist up to 96 hours in the immunocompromised. Pathogenesis, Immunity, Treatment and Prevention Norovirus is highly infectious due to low infecting dose, high excretion level (105 to 107 copies/mg stool), and continual shedding after clinical recovery (>1 month). The norovirus genome undergoes frequent change due to mutation and recombination, which increases its prevalence. Studies suggest that acquired immunity only last 6 months after infection. Gastroenteritis, an inflammation of the stomach and small and large intestines, is caused by norovirus infection. -

How Influenza Virus Uses Host Cell Pathways During Uncoating
cells Review How Influenza Virus Uses Host Cell Pathways during Uncoating Etori Aguiar Moreira 1 , Yohei Yamauchi 2 and Patrick Matthias 1,3,* 1 Friedrich Miescher Institute for Biomedical Research, 4058 Basel, Switzerland; [email protected] 2 Faculty of Life Sciences, School of Cellular and Molecular Medicine, University of Bristol, Bristol BS8 1TD, UK; [email protected] 3 Faculty of Sciences, University of Basel, 4031 Basel, Switzerland * Correspondence: [email protected] Abstract: Influenza is a zoonotic respiratory disease of major public health interest due to its pan- demic potential, and a threat to animals and the human population. The influenza A virus genome consists of eight single-stranded RNA segments sequestered within a protein capsid and a lipid bilayer envelope. During host cell entry, cellular cues contribute to viral conformational changes that promote critical events such as fusion with late endosomes, capsid uncoating and viral genome release into the cytosol. In this focused review, we concisely describe the virus infection cycle and highlight the recent findings of host cell pathways and cytosolic proteins that assist influenza uncoating during host cell entry. Keywords: influenza; capsid uncoating; HDAC6; ubiquitin; EPS8; TNPO1; pandemic; M1; virus– host interaction Citation: Moreira, E.A.; Yamauchi, Y.; Matthias, P. How Influenza Virus Uses Host Cell Pathways during 1. Introduction Uncoating. Cells 2021, 10, 1722. Viruses are microscopic parasites that, unable to self-replicate, subvert a host cell https://doi.org/10.3390/ for their replication and propagation. Despite their apparent simplicity, they can cause cells10071722 severe diseases and even pose pandemic threats [1–3]. -

Viruses in Transplantation - Not Always Enemies
Viruses in transplantation - not always enemies Virome and transplantation ECCMID 2018 - Madrid Prof. Laurent Kaiser Head Division of Infectious Diseases Laboratory of Virology Geneva Center for Emerging Viral Diseases University Hospital of Geneva ESCMID eLibrary © by author Conflict of interest None ESCMID eLibrary © by author The human virome: definition? Repertoire of viruses found on the surface of/inside any body fluid/tissue • Eukaryotic DNA and RNA viruses • Prokaryotic DNA and RNA viruses (phages) 25 • The “main” viral community (up to 10 bacteriophages in humans) Haynes M. 2011, Metagenomic of the human body • Endogenous viral elements integrated into host chromosomes (8% of the human genome) • NGS is shaping the definition Rascovan N et al. Annu Rev Microbiol 2016;70:125-41 Popgeorgiev N et al. Intervirology 2013;56:395-412 Norman JM et al. Cell 2015;160:447-60 ESCMID eLibraryFoxman EF et al. Nat Rev Microbiol 2011;9:254-64 © by author Viruses routinely known to cause diseases (non exhaustive) Upper resp./oropharyngeal HSV 1 Influenza CNS Mumps virus Rhinovirus JC virus RSV Eye Herpes viruses Parainfluenza HSV Measles Coronavirus Adenovirus LCM virus Cytomegalovirus Flaviviruses Rabies HHV6 Poliovirus Heart Lower respiratory HTLV-1 Coxsackie B virus Rhinoviruses Parainfluenza virus HIV Coronaviruses Respiratory syncytial virus Parainfluenza virus Adenovirus Respiratory syncytial virus Coronaviruses Gastro-intestinal Influenza virus type A and B Human Bocavirus 1 Adenovirus Hepatitis virus type A, B, C, D, E Those that cause -

Diversity and Evolution of Viral Pathogen Community in Cave Nectar Bats (Eonycteris Spelaea)
viruses Article Diversity and Evolution of Viral Pathogen Community in Cave Nectar Bats (Eonycteris spelaea) Ian H Mendenhall 1,* , Dolyce Low Hong Wen 1,2, Jayanthi Jayakumar 1, Vithiagaran Gunalan 3, Linfa Wang 1 , Sebastian Mauer-Stroh 3,4 , Yvonne C.F. Su 1 and Gavin J.D. Smith 1,5,6 1 Programme in Emerging Infectious Diseases, Duke-NUS Medical School, Singapore 169857, Singapore; [email protected] (D.L.H.W.); [email protected] (J.J.); [email protected] (L.W.); [email protected] (Y.C.F.S.) [email protected] (G.J.D.S.) 2 NUS Graduate School for Integrative Sciences and Engineering, National University of Singapore, Singapore 119077, Singapore 3 Bioinformatics Institute, Agency for Science, Technology and Research, Singapore 138671, Singapore; [email protected] (V.G.); [email protected] (S.M.-S.) 4 Department of Biological Sciences, National University of Singapore, Singapore 117558, Singapore 5 SingHealth Duke-NUS Global Health Institute, SingHealth Duke-NUS Academic Medical Centre, Singapore 168753, Singapore 6 Duke Global Health Institute, Duke University, Durham, NC 27710, USA * Correspondence: [email protected] Received: 30 January 2019; Accepted: 7 March 2019; Published: 12 March 2019 Abstract: Bats are unique mammals, exhibit distinctive life history traits and have unique immunological approaches to suppression of viral diseases upon infection. High-throughput next-generation sequencing has been used in characterizing the virome of different bat species. The cave nectar bat, Eonycteris spelaea, has a broad geographical range across Southeast Asia, India and southern China, however, little is known about their involvement in virus transmission. -
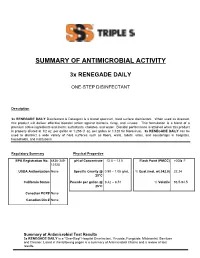
Summary of Antimicrobial Activity
SUMMARY OF ANTIMICROBIAL ACTIVITY 3x RENEGADE DAILY ONE-STEP DISINFECTANT Description 3x RENEGADE DAILY Disinfectant & Detergent is a broad spectrum, hard surface disinfectant. When used as directed, this product will deliver effective biocidal action against bacteria, fungi, and viruses. This formulation is a blend of a premium active ingredients and inerts: surfactants, chelates, and water. Biocidal performance is attained when this product is properly diluted at 1/2 oz. per gallon or 1:256 (1 oz. per gallon or 1:128 for Norovirus). 3x RENEGADE DAILY can be used to disinfect a wide variety of hard surfaces such as floors, walls, toilets, sinks, and countertops in hospitals, households, and institutions. Regulatory Summary Physical Properties EPA Registration No. 6836-349- pH of Concentrate 12.0 – 13.5 Flash Point (PMCC) >200 F 12120 USDA Authorization None Specific Gravity @ 0.98 – 1.05 g/mL % Quat (mol. wt.342.0) 22.24 25°C California Status Pounds per gallon @ 8.42 – 8.51 % Volatile 93.5-94.5 25°C Canadian PCP# None Canadian Din # None Summary of Antimicrobial Test Results 3x RENEGADE DAILY is a "One-Step" Hospital Disinfectant, Virucide, Fungicide, Mildewstat, Sanitizer and Cleaner. Listed in the following pages is a summary of Antimicrobial Claims and a review of test results. Claim: Contact time: Organic Soil: Water Conditions: Disinfectant Varies 5% 250ppm as CaCO3 Test Method: AOAC Germicidal Spray Test Organism Contact Dilution Time (Min) 868 ppm (1/2oz. per Acinetobacter baumannii 3 Gal) Bordetella bronchiseptica 3 868 ppm Bordetella pertussis 3 868 ppm Campylobacter jejuni 3 868 ppm Enterobacter aerogenes 3 1736 PPM (1 oz per Gal) Enterococcus faecalis 3 868 ppm Enterococcus faecalis - Vancomycin resistant [VRE] 3 868 ppm Escherichia coli 3 868 ppm Escherichia coli [O157:H7] 3 868 ppm Escherichia coli ESBL – Extended spectrum beta- 868 ppm 10 lactamase containing E. -

Borna Disease Virus Infection in Animals and Humans
Synopses Borna Disease Virus Infection in Animals and Humans Jürgen A. Richt,* Isolde Pfeuffer,* Matthias Christ,* Knut Frese,† Karl Bechter,‡ and Sibylle Herzog* *Institut für Virologie, Giessen, Germany; †Institut für Veterinär-Pathologie, Giessen, Germany; and ‡Universität Ulm, Günzburg, Germany The geographic distribution and host range of Borna disease (BD), a fatal neuro- logic disease of horses and sheep, are larger than previously thought. The etiologic agent, Borna disease virus (BDV), has been identified as an enveloped nonsegmented negative-strand RNA virus with unique properties of replication. Data indicate a high degree of genetic stability of BDV in its natural host, the horse. Studies in the Lewis rat have shown that BDV replication does not directly influence vital functions; rather, the disease is caused by a virus-induced T-cell–mediated immune reaction. Because antibodies reactive with BDV have been found in the sera of patients with neuro- psychiatric disorders, this review examines the possible link between BDV and such disorders. Seroepidemiologic and cerebrospinal fluid investigations of psychiatric patients suggest a causal role of BDV infection in human psychiatric disorders. In diagnostically unselected psychiatric patients, the distribution of psychiatric disorders was found to be similar in BDV seropositive and seronegative patients. In addition, BDV-seropositive neurologic patients became ill with lymphocytic meningoencephali- tis. In contrast to others, we found no evidence is reported for BDV RNA, BDV antigens, or infectious BDV in peripheral blood cells of psychiatric patients. Borna disease (BD), first described more predilection for the gray matter of the cerebral than 200 years ago in southern Germany as a hemispheres and the brain stem (8,19). -

And Filoviruses Asit K
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Papers in Veterinary and Biomedical Science Veterinary and Biomedical Sciences, Department of 2016 Overview of Rhabdo- and Filoviruses Asit K. Pattnaik University of Nebraska-Lincoln, [email protected] Michael A. Whitt University of Tennessee Health Science Center, [email protected] Follow this and additional works at: http://digitalcommons.unl.edu/vetscipapers Part of the Biochemistry, Biophysics, and Structural Biology Commons, Cell and Developmental Biology Commons, Immunology and Infectious Disease Commons, Medical Sciences Commons, Veterinary Microbiology and Immunobiology Commons, and the Veterinary Pathology and Pathobiology Commons Pattnaik, Asit K. and Whitt, Michael A., "Overview of Rhabdo- and Filoviruses" (2016). Papers in Veterinary and Biomedical Science. 229. http://digitalcommons.unl.edu/vetscipapers/229 This Article is brought to you for free and open access by the Veterinary and Biomedical Sciences, Department of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Papers in Veterinary and Biomedical Science by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Published in Biology and Pathogenesis of Rhabdo- and Filoviruses (2016), edited by Asit K Pattnaik and Michael A Whitt. Copyright © 2016 World Scientific Publishing Co Pte Ltd. Used by permission. digitalcommons.unl.edu CHAPTER 1 Overview of Rhabdo- and Filoviruses Asit K. Pattnaik1 and Michael A. Whitt2 1 School of Veterinary Medicine and Biomedical Sciences and Nebraska Center for Virology, University of Nebraska-Lincoln, Lincoln, Nebraska 68583 2 Department of Microbiology, Immunology, and Biochemistry, University of Tennessee Health Science Center, Memphis, Tennessee 38163 The authors contributed equally to this work. Emails: [email protected] ; [email protected] Summary Enveloped viruses with a negative-sense, single-stranded monopartite RNA genome have been classified into the orderMononegavirales . -

Hutchinson, EC, & Yamauchi, Y
Hutchinson, E. C., & Yamauchi, Y. (2018). Understanding Influenza. In Influenza Virus: Methods and Protocols (pp. 1-21). (Methods in Molecular Biology; Vol. 1836). Humana Press. https://doi.org/10.1007/978-1-4939-8678-1_1 Peer reviewed version Link to published version (if available): 10.1007/978-1-4939-8678-1_1 Link to publication record in Explore Bristol Research PDF-document This is the author accepted manuscript (AAM). The final published version (version of record) is available online via Springer Nature at https://link.springer.com/protocol/10.1007%2F978-1-4939-8678-1_1. Please refer to any applicable terms of use of the publisher. University of Bristol - Explore Bristol Research General rights This document is made available in accordance with publisher policies. Please cite only the published version using the reference above. Full terms of use are available: http://www.bristol.ac.uk/red/research-policy/pure/user-guides/ebr-terms/ Understanding Influenza Edward C. Hutchinson1* and Yohei Yamauchi2* 1MRC-University of Glasgow Centre for Virus Research; 2School of Cellular and Molecular Medicine, University of Bristol. *Corresponding authors: [email protected], [email protected] Running Head: Understanding Influenza Abstract Influenza, a serious illness of humans and domesticated animals, has been studied intensively for many years. It therefore provides an example of how much we can learn from detailed studies of an infectious disease, and of how even the most intensive scientific research leaves further questions to answer. This introduction is written for researchers who have become interested in one of these unanswered questions, but who may not have previously worked on influenza. -

Virus Pathogen Resource (Vipr) March 2019 New Features in Vipr
Virus Pathogen Resource (ViPR) March 2019 New Features in ViPR New Genome Annotation Tool New RNA Structure Data VIGOR4, a new genome annotation tool is In collaboration with the NIAID-funded Loading Virus Pathogen Database and AnalysisAbout Resource Us Community (ViPR)... Announcements Links Resources Support now available on the Zika virus portal. VIGOR4 Orfeome project, we have released new RNA News & Events (Viral Genome ORF Reader) is developed by structure data for MERS-CoV on the ViPR • June 9-13, 2019: Positive Strand J. Craig Venter Institute. VIGOR 4 predicts site. This new dataset is generated as part RNA Viruses, Killarney, Ireland. Oral protein sequences encoded in a viral of the effort to identify, characterize and presentation. genomes by sequences similarity searching then determine the role of uncharacterized against curated viral protein databases. viral genesSearch that may function to auto- Analyze• July 21-25, 2019: Annual Conference Save to Workbench regulate virus replication efficiency and host In the next few releases, we will enhance the Search our comprehensive database for: Analyzeon Intelligent data online: Systems for Molecular Use your workbench to: responses. The structure data is predicted Biology, Basel, Switzerland. current VIGOR4 implementation and make it Sequences & strains Sequence Alignment Store and share data available for other virus familes. using SHAPE chemical reactivity data (PMID: 22475022Immune). epitopes • AugustPhylogenetic 4-9, T2019:ree 24th International Combine working sets 3D protein -

University of Groningen Molecular Insights Into Viral Respiratory Infections Cong, Ying-Ying
University of Groningen Molecular insights into viral respiratory infections Cong, Ying-Ying IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2019 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Cong, Y-Y. (2019). Molecular insights into viral respiratory infections. University of Groningen. Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 25-09-2021 CHAPTER I General Introduction Chapter I The structure of the respiratory tract facilitates gas exchange between the exterior environment and interior milieu of the host, while it is a susceptible target and feasible gateway for diverse pathogens. Pandemics of severe acute respiratory infections have been serious threats to global health, causing significant morbidity and mortality. In particular, influenza viruses and coronaviruses (CoV), including MERS-CoV and SARS-CoV, have caused numerous outbreaks of viral pneumonia worldwide with different impacts.