Poster Sessions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Working Paper Reference
Working Paper Civil wars and state formation: violence and the politics of legitimacy in angola, côte d'ivoire and south sudan PECLARD, Didier, et al. Abstract Civil wars do not only destroy existing political orders. They contribute to shaping new ones, and thereby play a crucial role in dynamics of state formation. This working paper is based on a 2-year research project funded by the Swiss Network of International Studies and conducted by a consortium of five research institutions in Switzerland and Africa. It reflects on the social construction of order and legitimacy during and after violent conflict by focusing on political orders put in place by armed groups, their strategies to legitimize their (violent) action as well as their claim to power, and on the extent to which they strive and manage to institutionalize their military power and transform it into political domination. Drawing on case studies in Angola, Côte d'Ivoire and South Sudan, it shows how strategies of legitimization are central to understanding the politics of armed groups and their relation to the state, how international aid agencies impact on the legitimacy of armed groups and state actors, and how continuities between war and peace, especially in key sectors such as security forces, need to be taken [...] Reference PECLARD, Didier, et al. Civil wars and state formation: violence and the politics of legitimacy in angola, côte d'ivoire and south sudan. Geneva : University of Geneva / Swiss Network of International Studies (SNIS), 2019, 29 p. Available at: http://archive-ouverte.unige.ch/unige:134632 Disclaimer: layout of this document may differ from the published version. -

Africa «Afrique Africa • Afrique
WEEKLY EPIDEMIOLOGICAL RECORD, Ho. 12,20 MUCH 1W2 • RELEVE EPIDEMIOLOGIQUE HEBDOMADAIRE, » 12,20 MARS 1992 Influenza Grippe A ustria (23 February 1992). The first signs of influenza A utriche (23 février 1992). Les premiers signes d'activité grippale activity were scattered localized outbreaks in mid-January. ont été des flambées locales disséminées à la mi-janvier. Des cas Cases of influenza-like illness were detected all over the d'affections de type grippal ont été décelés dans tout le pays en country during February and activity reached epidemic février et l'activité a atteint des proportions épidémiques à Vienne. proportions in Vienna. Influenza A has been implicated on La grippe A a été mise en évidence par sérologie mais ria pas encore serological evidence but has not yet been confirmed by virus été confirmée par isolement du virus. isolation. Egypt (2 March 1992).* Additional cases of influenza Egypte (2 mars 1992).‘ Des cas supplémentaires de grippe A(H3N2) were diagnosed among cases of influenza-like A(H3N2) ont été diagnostiqués parmi des affections de type grippal illness investigated during December and January. étudiées en décembre et en janvier. Hong Kong (2 March 1992).2 * Influenza A(H3N2) virus Hong Kong (2 mars 1992).2 Le virus grippal A(H3N2) a été isolé was isolated from a sporadic case in January. d'un cas sporadique en janvier. Israel (28 February 1992).’ Influenza activity reached Israël (28 février 1992).’ L'activité grippale a atteint des niveaux epidemic levels in February. Cases have been seen in all age épidémiques en février. Des cas ont été observés dans tous les groups but most have been children. -

Description of a New Flat Gecko (Squamata: Gekkonidae: Afroedura) from Mount Gorongosa, Mozambique
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/320043814 Description of a new flat gecko (Squamata: Gekkonidae: Afroedura) from Mount Gorongosa, Mozambique Article in Zootaxa · September 2017 DOI: 10.11646/zootaxa.4324.1.8 CITATIONS READS 2 531 8 authors, including: William R Branch Jennifer Anna Guyton Nelson Mandela University Princeton University 250 PUBLICATIONS 4,231 CITATIONS 7 PUBLICATIONS 164 CITATIONS SEE PROFILE SEE PROFILE Andreas Schmitz Michael Barej Natural History Museum of Geneva Museum für Naturkunde - Leibniz Institute for Research on Evolution and Biodiver… 151 PUBLICATIONS 2,701 CITATIONS 38 PUBLICATIONS 274 CITATIONS SEE PROFILE SEE PROFILE Some of the authors of this publication are also working on these related projects: Monitoring and Managing Biodiversity Loss in South-East Africa's Montane Ecosystems View project Ad hoc herpetofauna observations View project All content following this page was uploaded by Jennifer Anna Guyton on 27 September 2017. The user has requested enhancement of the downloaded file. Zootaxa 4324 (1): 142–160 ISSN 1175-5326 (print edition) http://www.mapress.com/j/zt/ Article ZOOTAXA Copyright © 2017 Magnolia Press ISSN 1175-5334 (online edition) https://doi.org/10.11646/zootaxa.4324.1.8 http://zoobank.org/urn:lsid:zoobank.org:pub:B4FF9A5F-94A7-4E75-9EC8-B3C382A9128C Description of a new flat gecko (Squamata: Gekkonidae: Afroedura) from Mount Gorongosa, Mozambique WILLIAM R. BRANCH1,2,13, JENNIFER A. GUYTON3, ANDREAS SCHMITZ4, MICHAEL F. BAREJ5, PIOTR NASKRECKI6,7, HARITH FAROOQ8,9,10,11, LUKE VERBURGT12 & MARK-OLIVER RÖDEL5 1Port Elizabeth Museum, P.O. Box 13147, Humewood 6013, South Africa 2Research Associate, Department of Zoology, Nelson Mandela University, P.O. -

31 CFR Ch. V (7–1–05 Edition) Pt. 590, App. B
Pt. 590, App. B 31 CFR Ch. V (7–1–05 Edition) (2) Pneumatic tire casings (excluding tractor (C) Nharea and farm implement types), of a kind (2) Communities: specially constructed to be bulletproof or (A) Cassumbe to run when deflated (ECCN 9A018); (B) Chivualo (3) Engines for the propulsion of the vehicles (C) Umpulo enumerated above, specially designed or (D) Ringoma essentially modified for military use (E) Luando (ECCN 9A018); and (F) Sachinemuna (4) Specially designed components and parts (G) Gamba to the foregoing (ECCN 9A018); (H) Dando (f) Pressure refuellers, pressure refueling (I) Calussinga equipment, and equipment specially de- (J) Munhango signed to facilitate operations in con- (K) Lubia fined areas and ground equipment, not (L) Caleie elsewhere specified, developed specially (M) Balo Horizonte for aircraft and helicopters, and specially (b) Cunene Province: designed parts and accessories, n.e.s. (1) Municipalities: (ECCN 9A018); [Reserved] (g) Specifically designed components and (2) Communities: parts for ammunition, except cartridge (A) Cubati-Cachueca cases, powder bags, bullets, jackets, (B) [Reserved] cores, shells, projectiles, boosters, fuses (c) Huambo Province: and components, primers, and other det- (1) Municipalities: onating devices and ammunition belting (A) Bailundo and linking machines (ECCN 0A018); (B) Mungo (h) Nonmilitary shotguns, barrel length 18 (2) Communities: inches or over; and nonmilitary arms, (A) Bimbe discharge type (for example, stun-guns, (B) Hungue-Calulo shock batons, etc.), except arms designed (C) Lungue solely for signal, flare, or saluting use; (D) Luvemba and parts, n.e.s. (ECCNs 0A984 and 0A985); (E) Cambuengo (i) Shotgun shells, and parts (ECCN 0A986); (F) Mundundo (j) Military parachutes (ECCN 9A018); (G) Cacoma (k) Submarine and torpedo nets (ECCN (d) K. -

Huambo, Huila, Benguela, Cuanza Sul, Namibe and Cunene)
Agrometeorological Bulletin No. 4 Period October 2020 – April 2021 [English version] Crop and Rangeland monitoring in Angola (Huambo, Huila, Benguela, Cuanza Sul, Namibe and Cunene) Highlights ● The worst drought in 30 years affected the 2020/2021 agricultural season in the southwestern part of the country. ● Harvest of cereals will be completed in June and production prospects are very poor in the affected provinces. ● Low pasture production is expected in Namibe and Cunene, two provinces already stricken by drought also in the 2018/2019 agricultural season. Overview The six provinces of Huambo, Huila, Benguela, Cuanza Sul, Namibe, and Cunene, located in the central and southern part of the country, experienced a poor agricultural season in 2020/2021 due to the worst drought in 30 years that affected these provinces. Although rainfall started on time in most parts of the country, the dry conditions from December 2020 to February 2021 significantly impacted vegetation growth at a critical period for crop development. The rainfall graph with data from the meteorological station in Huambo (note: missing data in March), clearly highlights the good initial rainfall conditions, and the long dry spell that followed. The map of the z-score of cumulative NDVI, an indicator of vegetation biomass level, indicates in red areas with very poor vegetation conditions at the end of April 2021. Harvest of cereal crops will be completed in June in the country and weather conditions during the season as well as satellite images of vegetation status suggest poor cereal and pasture production prospects in the affected provinces due to one of the worst droughts of the last 30 years. -

Chapter 3 Profile of the Study Area
Chapter 3 Profile of the Study Area 3.1 Benguela Province 3.1.1 Outline Benguela Province is located in mid-west Angola. Its northern part meets the Province of Kwanza Sul, the east with Huambo, and the south with the Province of Huila and Namibe. The surface area is 39,826,83km2, and covers 3.19% of the national territory. It consists of 9 Municipalities including Lobito, and 27 Comunas and has a population of 1.93 million. The major Municipalities are Lobito (population: 736,000), Benguela (470,000) and Cubal (230,000). Its climate is dry and hot in the coastal areas, with an average temperature of 24.2 degrees Celsius with a highest temperature of 35 degrees Celsius. Vegetation is concentrated in the western areas, and in recent years, the forest areas along the coastline are decreasing due to deforestation. It has approx 1 million hectare of potential farmland and can produce various agricultural products thanks to its rich land and water sources. Primary products include bananas, corn, potatoes (potato, sweet potato), wheat flour, coconuts, beans, citrus fruit, mangos, and sugar cane. It is known nationwide for its variety of production, and the scale of cattle breeding ranks 4th in country. Currently cultivated areas total approx 214,000ha, and the production of primary products reaches approx 247,000 tons. Table 3-1 Profile of Municipalities in Benguela (As of 2007) Estimated Surface area Municipality Density/km2 population (km2) Benguela 469,363 2,100 223.5 Lobito 736,978 3,685 200.0 Baia Farta 97,720 6,744 14.5 Ganda 190,006 4,817 39.4 Cubal 230,848 4,794 48.2 Caimbambo 44,315 3,285 13.5 Balombo 27,942 2,635 10.6 Bocoio 55,712 5,612 9.9 Chongoroi 75,256 6,151 12.2 Total.. -

United Nations Office for the Coordination of Humanitarian Affairs (Ocha)
UNITED NATIONS OFFICE FOR THE COORDINATION OF HUMANITARIAN AFFAIRS (OCHA) HUMANITARIAN SITUATION IN ANGOLA Situation Report Reporting Period: 1 – 15 October 2003 Critical Issues q Humanitarian partners reported concerns about the food security situation in Chicuma, Ganda Municipality, Benguela Province. q The Kuito – Chipeta road in Bié Province was reopened for humanitarian operations. q A drought is causing hunger amongst populations in the municipalities of Cahama, Kuvelai, Kwanhama and Ombanja, Cunene Province. q Thirty metric tons of food for distribution in Rivungo were delayed at the Namibian border due to transport problems and bad road conditions. q Food distribution was temporarily suspended in Calandula Municipality, Malanje Province, after humanitarian workers were beaten during a distribution. q Due to an increased number of returning refugees from Zambia, there is a shortage in seeds and tools for distribution in Lumbala N’Guimbo, Moxico Province. Provincial Update Bengo Province: The road to Muxaluando has been partially rehabilitated easing access to Nambuangongo which will be assessed at the end of the month. Humanitarian partners are beginning interventions in Cassoneca, including much-needed water facilities projects, in preparation for the expected arrival of 2,000 refugees and returning populations. Benguela Province: Humanitarian partners conducting an assessment in Chicuma, Ganda Municipality report the food security situation is alarming. During a recent assessment humanitarian partners found that the population lacked adequate food reserves and seeds and tools for the agricultural season. Although malnutrition levels are currently under control, humanitarian partners recommend the extending the supplementary feeding centre as a preventive measure due to the food insecurity combined with a weak health system. -

Thesis Presented for the Degree Of
The copyright of this thesis vests in the author. No quotation from it or information derived from it is to be published without full acknowledgement of the source. The thesis is to be used for private study or non- commercial research purposes only. Published by the University of Cape Town (UCT) in terms of the non-exclusive license granted to UCT by the author. University of Cape Town Thesis Presented for the Degree of DOCTOR OF PHILOSOPHY In the Department of Social Anthropology UNIVERSITY OF CAPE TOWN November 2009 Ambitions of cidade: War-displacement and concepts of the urban among bairro residents in Benguela, Angola University of Cape Town Sandra Roque Doctorate in Social Anthropology - Ambitions of cidade: War-displacement and concepts of the urban among bairro residents in Benguela, Angola Contents LIST OF TABLES ----------------------------------------------------------------------------------------------------- III LIST OF MAPS -------------------------------------------------------------------------------------------------------- III ABSTRACT ------------------------------------------------------------------------------------------------------------ IV ACKNOWLEDGEMENTS --------------------------------------------------------------------------------------------- V CHAPTER 1: ENCOUNTERS, SITES AND QUESTIONS -----------------------------------------------1 THE MAP IN THE DUST -----------------------------------------------------------------------------------------------1 THE SITES OF THIS STUDY: BENGUELA AND BAIRRO CALOMBOTÃO -
Creating Markets in Angola : Country Private Sector Diagnostic
CREATING MARKETS IN ANGOLA MARKETS IN CREATING COUNTRY PRIVATE SECTOR DIAGNOSTIC SECTOR PRIVATE COUNTRY COUNTRY PRIVATE SECTOR DIAGNOSTIC CREATING MARKETS IN ANGOLA Opportunities for Development Through the Private Sector COUNTRY PRIVATE SECTOR DIAGNOSTIC CREATING MARKETS IN ANGOLA Opportunities for Development Through the Private Sector About IFC IFC—a sister organization of the World Bank and member of the World Bank Group—is the largest global development institution focused on the private sector in emerging markets. We work with more than 2,000 businesses worldwide, using our capital, expertise, and influence to create markets and opportunities in the toughest areas of the world. In fiscal year 2018, we delivered more than $23 billion in long-term financing for developing countries, leveraging the power of the private sector to end extreme poverty and boost shared prosperity. For more information, visit www.ifc.org © International Finance Corporation 2019. All rights reserved. 2121 Pennsylvania Avenue, N.W. Washington, D.C. 20433 www.ifc.org The material in this work is copyrighted. Copying and/or transmitting portions or all of this work without permission may be a violation of applicable law. IFC does not guarantee the accuracy, reliability or completeness of the content included in this work, or for the conclusions or judgments described herein, and accepts no responsibility or liability for any omissions or errors (including, without limitation, typographical errors and technical errors) in the content whatsoever or for reliance thereon. The findings, interpretations, views, and conclusions expressed herein are those of the authors and do not necessarily reflect the views of the Executive Directors of the International Finance Corporation or of the International Bank for Reconstruction and Development (the World Bank) or the governments they represent. -

United Nations Office for the Coordination of Humanitarian Affairs (Ocha)
UNITED NATIONS OFFICE FOR THE COORDINATION OF HUMANITARIAN AFFAIRS (OCHA) HUMANITARIAN SITUATION IN ANGOLA Situation Report Reporting Period: 1 – 15 September 2003 Critical Issues q Fourteen deminers were injured when an anti-tank mine exploded on the Cambaxe – Malanje road in Malanje Municipality. q A meningitis outbreak has been confirmed in Huíla Province and a significant number of cases have been reported in Malanje Province. q Due to the start of the rainy season, humanitarian partners were not able to transport more seeds and tool kits to the interior of Kuanza Sul Province. q A donation of seeds and tools for 8,000 beneficiaries in Lunda Sul was cancelled due to lack of a partner to carry out the distribution. q Most of the seeds and tools for distribution in Moxico Province have yet to arrive. Provincial Update Luanda Province: The Provincial Government transported 2,030 people to Malanje. They are staying in the Katepa transit centre where they are sleeping in the open air and have no access to food, water, sanitation and health assistance. According to provincial authorities, one person died on arrival and no transportation is available for onward travel to areas of origin. Benguela Province: During the reporting period, local authorities closed the Benguela transit centre located in a former military quartering camp and moved the 250 people to the new Capiandalo transit centre approximately five km outside the city centre. An additional 108 demobilised soldiers and their dependents arrived from the former Menga gathering area in Huambo and humanitarian partners report that the people in the new camp are living in substandard conditions. -
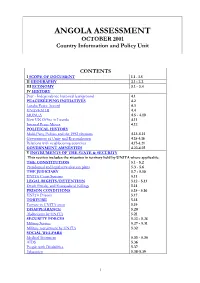
ANGOLA ASSESSMENT OCTOBER 2001 Country Information and Policy Unit
ANGOLA ASSESSMENT OCTOBER 2001 Country Information and Policy Unit CONTENTS I SCOPE OF DOCUMENT 1.1 - 1.5 II GEOGRAPHY 2.1 - 2.2 III ECONOMY 3.1 - 3.4 IV HISTORY Post - Independence historical background 4.1 PEACEKEEPING INITIATIVES 4.2 Lusaka Peace Accord 4.3 UNAVEM III 4.4 MONUA 4.5 - 4.10 New UN Office in Luanda 4.11 Internal Peace Moves 4.12 POLITICAL HISTORY Multi-Party Politics and the 1992 elections 4.13-4.14 Government of Unity and Reconciliation 4.15-4.16 Relations with neighbouring countries 4.17-4.21 GOVERNMENT AMNESTIES 4.22-4.25 V INSTRUMENTS OF THE STATE & SECURITY This section includes the situation in territory held by UNITA where applicable. THE CONSTITUTION 5.1 - 5.2 Presidential and legislative election plans 5.3 - 5.6 THE JUDICIARY 5.7 - 5.10 UNITA Court Systems 5.11 LEGAL RIGHTS/DETENTION 5.12 - 5.13 Death Penalty and Extrajudicial Killings 5.14 PRISON CONDITIONS 5.15 - 5.16 UNITA Prisons 5.17 TORTURE 5.18 Torture in UNITA areas 5.19 DISAPPEARANCE 5.20 Abductions by UNITA 5.21 SECURITY FORCES 5.22 - 5.26 Military Service 5.27 - 5.31 Military recruitment by UNITA 5.32 SOCIAL WELFARE Medical Treatment 5.33 - 5.35 AIDS 5.36 People with Disabilities 5.37 Education 5.38-5.39 1 VI HUMAN RIGHTS- GENERAL ASSESSMENT OF THE SITUATION Introduction 6.1 SECURITY SITUATION Recent developments in the Civil War 6.2 - 6.17 Security situation in Luanda 6.18 - 6.19 Landmines 6.20 - 6.22 Human Rights monitoring 6.23 - 6.26 VII SPECIFIC GROUPS REFUGEES 7.1 Internally Displaced Persons & Humanitarian Situation 7.2-7.5 UNITA 7.6-7.8 Recent Political History of UNITA 7.9-7.12 UNITA-R 7.13-7.14 UNITA Military Wing 7.15-7.20 Surrendering UNITA Fighters 7.21 Sanctions against UNITA 7.22-7.25 F.L.E.C/CABINDANS 7.26 History of FLEC 7.27-7.28 Recent FLEC activity 7.29-7.34 The future of Cabindan separatists 7.35 ETHNIC GROUPS 7.36-7.37 Bakongo 7.38-7.46 WOMEN 7.47 Discrimination against women 7.48-7.59 CHILDREN 7.50-7.55 VIII RESPECT FOR CIVIL LIBERTIES This section includes the situation in territory held by UNITA where applicable. -

(Consulting Services) Republic of Angola Ministry
REQUEST FOR EXPRESSIONS OF INTEREST (CONSULTING SERVICES) REPUBLIC OF ANGOLA MINISTRY OF ENERGY AND WATER (MINEA) NATIONAL DIRECTORATE OF WATER (DNA) INSTITUTIONAL AND SUSTAINABILITY SUPPORT TO URBAN WATER SUPPLY AND SANITATION SERVICE DELIVERY PROJECT C010C-ISSUWSSSD Water and Sanitation Sector Financing Agreement reference: 2000130013430 Project ID No.: P-AO-E00-005 The Government of Angola (GOA) has received financing from the African Development Bank toward the cost of the Institutional and Sustainability Support to Urban Water Supply and Sanitation Service Delivery Project (ISSUWSSSDP), and intends to apply part of the agreed amount for this loan to payments under the contract for Consultancy Service for Coastal Towns Waste Water Management Study for Benguela, Lobito and Baia Farta Towns. (CO10C-ISSUWSSSD). The services under this assignment will include for (i) Preparation of the Preliminary Design and Feasibility Study for Baia Frata, Benguela and Lobito Towns, (ii) Preparation of the Detailed Design of a Sewerage System and Wastewater Treatment plant for the Benguela and Lobito towns, (iii) To carry out Environmental and Social Impact Assessment Study for the construction of the wastewater sewerage system and wastewater treatment plant for the 3 Towns. Lobito and Baia Farta are located in Benguela Province. Benguela town is 539km from Luanda. Lobito and Baia farta in turn are located 34.4km and 28.9km respectively from Benguela town. The executive agency for the Project is the Ministry of Energy and Water (MINEA) which will use the existing project management unit within the National Water Directorate (DNA) known as the Financial and Contract Management Unit (FCMU). The service duration will be 12 months and it is expected to commence in March 2018.