How Clean Is Safe? Improving the Effectiveness of Decontamination of Structures and People Following Chemical and Biological Incidents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Denial the Death of Kurt Cobain the Seattle
A DENIAL THE DEATH OF KURT COBAIN THE SEATTLE POLIECE DEPARTMENT’S SUBSTANDARD INVESTIGATION & THE REPROCUSSIONS TO JUSTICE by BREE DONOVAN A Capstone Submitted to The Graduate School-Camden Rutgers, The State University, New Jersey in partial fulfillment of the requirements for the degree of Masters of Arts in Liberal Studies Under the direction of Dr. Joseph C. Schiavo and approved by _________________________________ Capstone Director _________________________________ Program Director Camden, New Jersey, December 2015 CAPSTONE ABSTRACT A Denial The Death of Kurt Cobain The Seattle Police Department’s Substandard Investigation & The Repercussions to Justice By: BREE DONOVAN Capstone Director: Dr. Joseph C. Schiavo Kurt Cobain (1967-1994) musician, artist songwriter, and founder of The Rock and Roll Hall of Fame band, Nirvana, was dubbed, “the voice of a generation”; a moniker he wore like his faded cardigan sweater, but with more than some distain. Cobain’s journey to the top of the Billboard charts was much more Dickensian than many of the generations of fans may realize. During his all too short life, Cobain struggled with physical illness, poverty, undiagnosed depression, a broken family, and the crippling isolation and loneliness brought on by drug addiction. Cobain may have shunned the idea of fame and fortune but like many struggling young musicians (who would become his peers) coming up in the blue collar, working class suburbs of Aberdeen and Tacoma Washington State, being ii on the cover of Rolling Stone magazine wasn’t a nightmare image. Cobain, with his unkempt blond hair, polarizing blue eyes, and fragile appearance is a modern-punk-rock Jesus; a model example of the modern-day hero. -
Order Form Full
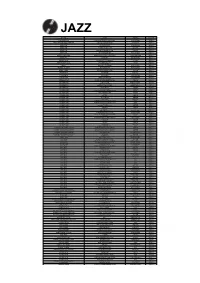
JAZZ ARTIST TITLE LABEL RETAIL ADDERLEY, CANNONBALL SOMETHIN' ELSE BLUE NOTE RM112.00 ARMSTRONG, LOUIS LOUIS ARMSTRONG PLAYS W.C. HANDY PURE PLEASURE RM188.00 ARMSTRONG, LOUIS & DUKE ELLINGTON THE GREAT REUNION (180 GR) PARLOPHONE RM124.00 AYLER, ALBERT LIVE IN FRANCE JULY 25, 1970 B13 RM136.00 BAKER, CHET DAYBREAK (180 GR) STEEPLECHASE RM139.00 BAKER, CHET IT COULD HAPPEN TO YOU RIVERSIDE RM119.00 BAKER, CHET SINGS & STRINGS VINYL PASSION RM146.00 BAKER, CHET THE LYRICAL TRUMPET OF CHET JAZZ WAX RM134.00 BAKER, CHET WITH STRINGS (180 GR) MUSIC ON VINYL RM155.00 BERRY, OVERTON T.O.B.E. + LIVE AT THE DOUBLET LIGHT 1/T ATTIC RM124.00 BIG BAD VOODOO DADDY BIG BAD VOODOO DADDY (PURPLE VINYL) LONESTAR RECORDS RM115.00 BLAKEY, ART 3 BLIND MICE UNITED ARTISTS RM95.00 BROETZMANN, PETER FULL BLAST JAZZWERKSTATT RM95.00 BRUBECK, DAVE THE ESSENTIAL DAVE BRUBECK COLUMBIA RM146.00 BRUBECK, DAVE - OCTET DAVE BRUBECK OCTET FANTASY RM119.00 BRUBECK, DAVE - QUARTET BRUBECK TIME DOXY RM125.00 BRUUT! MAD PACK (180 GR WHITE) MUSIC ON VINYL RM149.00 BUCKSHOT LEFONQUE MUSIC EVOLUTION MUSIC ON VINYL RM147.00 BURRELL, KENNY MIDNIGHT BLUE (MONO) (200 GR) CLASSIC RECORDS RM147.00 BURRELL, KENNY WEAVER OF DREAMS (180 GR) WAX TIME RM138.00 BYRD, DONALD BLACK BYRD BLUE NOTE RM112.00 CHERRY, DON MU (FIRST PART) (180 GR) BYG ACTUEL RM95.00 CLAYTON, BUCK HOW HI THE FI PURE PLEASURE RM188.00 COLE, NAT KING PENTHOUSE SERENADE PURE PLEASURE RM157.00 COLEMAN, ORNETTE AT THE TOWN HALL, DECEMBER 1962 WAX LOVE RM107.00 COLTRANE, ALICE JOURNEY IN SATCHIDANANDA (180 GR) IMPULSE -

The Meaning of Velvet Jennifer Jean Wright Iowa State University
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 2000 The meaning of velvet Jennifer Jean Wright Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Creative Writing Commons, and the English Language and Literature Commons Recommended Citation Wright, Jennifer Jean, "The meaning of velvet" (2000). Retrospective Theses and Dissertations. 16209. https://lib.dr.iastate.edu/rtd/16209 This Thesis is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. The meaning of velvet by Jennifer Jean Wright A thesis submitted to the graduate faculty in partial fulfillment of the requirements for the degree of MASTER OF ARTS Major: English (Creative Writing) Major Professor: Stephen Pett Iowa State University Ames, Iowa 2000 Copyright © Jennifer Jean Wright, 2000. All rights reserved. iii that's the girl that he takes around town. she appears composed, so she is I suppose, who can really tell? she shows no emotion at all stares into space like a dead china doll. --Elliot Smith, waltz #2 The ashtray says you were up all night when you went to bed with your darkest mind your pillow wept and covered your eyes you finally slept while the sun caught fire You've changed. --Wilco, a shot in the arm two headed boy all floating in glass the sun now it's blacker then black I can hear as you tap on your jar I am listening to hear where you are .. -

ROUTE66 – Drfeelgood Well If You Ever Plan to Motor West Just Take
ROUTE66 – DrFeelgood https://www.youtube.com/watch?v=G-vleD9AUtk A D A A D D A A E D A A E7 Well if you ever plan to motor west Just take my way it's the highway that's the best Get your kicks on Route 66 Well it winds from Chicago to L.A. More than 2000 miles all the way Get your kicks on Route 66 Well it goes from St Louis, down to Missouri Oklahoma city looks oh so pretty You'll see Amarillo and Gallup, New Mexico Flagstaff, Arizona don't forget Winona Kingsman, Barstaw, San Bernadino Would you get hip to this kindly trip And take that California trip Get your kick on Route 66 It goes from St. Louis, down to Missouri Oklahoma city looks oh so pretty You'll see Amarillo and Gallup, New Mexico Flagstaff, Arizona don't forget Winona Kingsman, Barstaw, San Berdino Would you get hip to this kindly trip Take that California trip Get your kicks on Route 66 Get your kicks on Route 66 Get your kicks on Route 66 Get your kicks on Route 66 GET BACK – The Beatles https://www.youtube.com/watch?v=YEESfv-11ng Estrofa: A A7 D A A A7 D A Estribillo: A A7 D A G D A A7 D A Jojo was a man who thought he was a loner But he knew it wouldn't last Jojo left his home in Tucson, Arizona For some California grass Get back, get back Get back to where you once belonged Get back, get back Get back to where you once belonged Get back Jojo Get back, get back Back to where you once belonged Get back, get back Back to where you once belonged Get back Jo Sweet Loretta Martin thought she was a woman But she was another man All the girls around her say she's got it coming -

Ebola and Marburg Virus Disease Epidemics: Preparedness, Alert, Control and Evaluation
EBOLA STRATEGY Ebola and Marburg virus disease epidemics: preparedness, alert, control and evaluation August 2014 © World Health Organization 2014. All rights reserved. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use. WHO/HSE/PED/CED/2014.05 Contents Acknowledgements ............................................................................................................ 5 List of abbreviations and acronyms ................................................................................... 6 Chapter 1 – Introduction .................................................................................................... 7 1.1 Purpose of the document and target audience .................................................................... -

Amy | ‘Tis the Season | Meru | the Wolfpack | the Jinx | Big Men | Caring for Mom & Dad | Walt Disney | the Breach | GTFO Scene & He D
November-December 2015 VOL. 30 THE VIDEO REVIEW MAGAZINE FOR LIBRARIES NO. 6 IN THIS ISSUE Amy | ‘Tis the Season | Meru | The Wolfpack | The Jinx | Big Men | Caring for Mom & Dad | Walt Disney | The Breach | GTFO scene & he d BAKER & TAYLOR’S SPECIALIZED A/V TEAM OFFERS ALL THE PRODUCTS, SERVICES AND EXPERTISE TO FULFILL YOUR LIBRARY PATRONS’ NEEDS. Le n more about Bak & Taylor’s Scene & He d team: ELITE Helpful personnel focused exclusively on A/V products and customized services to meet continued patron demand PROFICIENT Qualified entertainment content buyers ensure frontlist and backlist titles are available and delivered on time SKILLED Supportive Sales Representatives with an average of 15 years industry experience DEVOTED Nationwide team of A/V processing staff ready to prepare your movie and music products to your shelf-ready specifications KNOWLEDGEABLE Full-time staff of A/V catalogers, backed by their MLS degree and more than 43 years of media cataloging expertise 800-775-2600 x2050 [email protected] www.baker-taylor.com Spotlight Review Amy HHH 2011, she died of alcohol toxicity at the age of Lionsgate, 128 min., R, 27. Drawing on early home movies, newsreel DVD: $19.98, Blu-ray: footage, and recorded audio interviews, Amy $24.99, Dec. 1 serves up a sorrowful portrait of an artist’s Publisher/Editor: Randy Pitman This disturbing, dis- deadly downward spiral. Extras include au- concerting, booze ‘n’ dio commentary by the director, previously Associate Editor: Jazza Williams-Wood drugs documentary unseen performances by Winehouse, and Copy Editor: Kathleen L. Florio about British song- deleted scenes. -

Kuwait's Mps Pass Laws to Regulate Domestic Helpers
SUBSCRIPTION THURSDAY, JUNE 18, 2015 RAMADAN 1, 1436 AH www.kuwaittimes.net Emsak: 03:03 Fajer: 03:13 Dohr: 11:49 Asr: 15:23 Maghreb: 18:50 Eshaa: 20:22 Kuwait’s MPs pass laws to Min 32º Max 46º regulate domestic helpers High Tide 01:10 & 12:25 Low Tide MPs vote to establish human rights body 06:40 & 19:45 40 PAGES NO: 16555 150 FILS By B Izzak from the editor’s desk KUWAIT: In another marathon session, the National Ramadan Greets Assembly yesterday passed in principle three key legisla- tions regulating the affairs of domestic helpers and estab- lishing a shareholding company for their recruitment in addition to establishing the national human rights commis- sion. The law on domestic helpers is the first legislation in the country to provide full legal protection to hundreds of By Abd Al-Rahman Al-Alyan thousands of maids in Kuwait. So far, a decision issued by the Interior Ministry is the only legal framework for maids. The second and final vote is expected to take place next week for the law which grants [email protected] domestic helpers unprecedented rights including limiting daily working hours to eight, a mandatory weekend and a irst of all, I would like to wish HH the Amir 30-day paid annual leave. Sheikh Sabah Al-Ahmad Al-Sabah, HH the For the first time, the law sets a minimum wage of KD 45 FCrown Prince Sheikh Nawaf Al-Ahmad Al-Sabah, monthly for maids who are entitled to demand overtime HH the Prime Minister Sheikh Jaber Al-Mubarak Al- for working extra hours. -

Ellis & Associates, Inc
INTERNATIONAL LIFEGUARD Training Program Manual 5th Edition Meets ECC, MAHC, and OSHA Guidelines Ellis & Associates, Inc. 5979 Vineland Rd. Suite 105 Orlando, FL 32819 www.jellis.com 800-742-8720 Copyright © 2020 by Ellis & Associates, Inc. All rights reserved. Unless otherwise indicated in writing by Ellis & Associates, the recipient of this manual is granted the limited right to download, print, photocopy, and use the electronic materials to fulfill Ellis & Associates lifeguard courses, subject to the following restrictions: • The recipient is prohibited from downloading the materials for use on their own website. • The recipient cannot sell electronic versions of the materials. • The recipient cannot revise, alter, adapt, or modify the materials. • The recipient cannot create derivative works incorporating, in part or in whole, any content of the materials. For permission requests, write to Ellis & Associates, addressed “Attention: Permissions Coordinator,” at the address above. Disclaimer: The procedures and protocols presented in this manual and the course are based on the most current recommendations of responsible medical sources, including the International Liaison Committee on Resuscitation (ILCOR) Consensus Guidelines for CPR, Emergency Cardiovascular Care (ECC) and First Aid, the Occupational Safety and Health Administration (OSHA) standards 1910.151, and the Model Aquatic Health Code (MAHC). The materials have been reviewed by internal and external field experts and verified to be consistent with the most current guidelines and standards. Ellis & Associates, however, make no guarantee as to, and assume no responsibility for, the correctness, sufficiency, or completeness of such recommendations or information. Additional procedures may be required under particular circumstances. Ellis & Associates disclaims all liability for damages of any kind arising from the use of, reference to, reliance on, or performance based on such information. -

Jewish Attitudes Toward Poles: in Search of Haman5
May 2020 “...a Jew from Poland is not and never was simply Polish. … it was clear to Jews and Poles alike that they were two very different peoples who happened to share the same piece of territory. They could be neighbors and business partners, but they were seldom friends and almost never relatives or social or legal equals.” 1 Adam Kirsch, American poet and critic The ethno-nationalist spin for this state of affairs: “It’s all the Poles’ fault!” “Their animus, which carries Polish nationalism into such an aggressively xenophobic articulation, springs primarily from a deep pool of ethnic-cum- religious hatred, which is indigenous to Poland and has historically been aimed at Jews.”2 Jan T. Gross, American sociologist “…the sort of primitive anti-Polish sentiments that too often characterize those whom I shall call ‘professional Jews’.”3 French-Jewish historian Pierre Vidal-Naquet “…it is possible for Jewish people to be racist, just as it is possible for people of other faiths to be.” 4 John Bercow, former Speaker of U.K. House of Commons Traditional Jewish Attitudes Toward Poles: In Search of Haman5 by Mark Paul Mutual prejudices and stereotypes have been harboured by both Poles and Jews in regard to one another for long centuries. Few scholars in the West, however, have recognized that Jews, no less than Poles, 1 Adam Kirsch, “A Cruel and Elusive Family History,” Tablet, January 2, 2018. 2 Jan T. Gross, “Poles Cry for “Pure Blood’ Again,” The New York Times, November 16, 2017. 3 Pierre Vidal-Naquet, The Jews: History, Memory, and the Present (New York: Columbia University Press, 1996), 182. -

Spare Change Edition
The Role Playing Game SPARE CHANGE EDITION Special Note To minimize danger of fatal head explosion, do not read this book in its entirety. Read “In Brief” sections to get a general idea of the setting and game, then go back to read in depth for specific reference. Thank you for your cooperation. gmcf rfse (Order #27834702) FATES WORSE THAN DEATH the Role Playing Game SPARE CHANGE EDITION is published by Vajra Enterprises, Eureka California Written and Designed by Brian St.Claire-King Cover by Jason Juta Art by Lorie Albrecht (www.albrecht-illo.com), A’Lis, Samuel Araya, Paul C Butler, Leanne Buckley, Lance William Card, Jhoneil Centeno, Kari Christensen, Laura Dubuk, Randy Gallegos (randyg.com), Jason Juta, Kyri Konitou, Britt Martin, Rik Martin, Staffan Melin, Katie Miranda, Martina Pilcerova, Brian St.Claire-King, Jason Walton, Ursula Vernon Playtested by Jeremiah Barkman, David Reed, Amber Buhler, Skip Buhler, Tiffany St.Claire-King, Teresa Montalban, Gail Camaya Jotham McMillan, Karl Iliev, Victor Lim, Brennan Pike, Ryan Macklin, Scott Monday, Kevin Elser, Ethan Hamrick, Brian Formiconi, Gary Townsend, F. Douglas Wall, Chris Musgrave, Sean Musgrave Game Design Assistance by Robert Kwon and Tiffany St.Claire-King (Hey guys, no matter how much I argued with you at the time, I ended up taking most of your advice. Weird, huh? –Brian) Editorial Assistance by Tiffany St.Claire-King Additional Thanks to Matthew Thompson, Peter Geissert, Robert Kwon, Eric V. T. Nakano, Katie Riley, Brennan Pike, Jeffrey W. F. Walker, John Laviolette, Paul Barnett, Rob Lowry, Eeyore, Sandy Antunes, Chris Garland, Rebecca King, Steve Johnson and Guy McLimore. -

Ekbom Syndrome: the Challenge of “Invisible Bug” Infestations
ANRV397-EN55-05 ARI 1 November 2009 10:18 Ekbom Syndrome: The Challenge of “Invisible Bug” Infestations Nancy C. Hinkle Department of Entomology, University of Georgia, Athens, Georgia 30602-2603; email: [email protected] Annu. Rev. Entomol. 2010. 55:77–94 by University of Georgia on 01/05/10. For personal use only. Key Words First published online as a Review in Advance on parasitosis, delusion, invisible bug, infestation, formication August 11, 2009 The Annual Review of Entomology is online at Abstract Annu. Rev. Entomol. 2010.55:77-94. Downloaded from arjournals.annualreviews.org ento.annualreviews.org Ekbom Syndrome is synonymous with delusory parasitosis, a belief that This article’s doi: one’s body is infested by invisible bugs. Persons suffering from this syn- 10.1146/annurev.ento.54.110807.090514 drome often claim to feel dermal sensations and to visualize the bugs, Copyright c 2010 by Annual Reviews. although no one else can see them. Ekbom Syndrome is a delusional All rights reserved condition; it is intractable and cannot be corrected by argument or evi- 0066-4170/10/0107-0077$20.00 dence. Ekbom Syndrome sufferers exhibit a range of predictable behav- iors in their attempts to eliminate their infestations, including seeking identifications and treatment from physicians and entomologists. Fre- quently they also experience comorbid psychological conditions. Be- cause this is a delusional affliction, successful treatment typically re- quires neuroleptic medications, necessitating intervention by medical professionals. 77 ANRV397-EN55-05 ARI 1 November 2009 10:18 INTRODUCTION Those afflicted with ES often experience visual and tactile hallucinations perceived as Ekbom Syndrome (ES) is the clinical term for bugs crawling in or on the skin (46, 119). -

Leftovers: a Search for the Freegan Ideal
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 2009 Leftovers: A Search for the Freegan Ideal Emily Darrell The University of Montana Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Darrell, Emily, "Leftovers: A Search for the Freegan Ideal" (2009). Graduate Student Theses, Dissertations, & Professional Papers. 618. https://scholarworks.umt.edu/etd/618 This Professional Paper is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. LEFTOVERS: A SEARCH FOR THE FREEGAN IDEAL By Emily Lauren Darrell B.A., Virginia Commonwealth University, Richmond, VA 2004 Professional Paper Presented in partial fulfillment of the requirements for the degree of Master of Arts in Journalism The University of Montana Missoula, MT December 2009 Approved by: Perry Brown, Associate Provost for Graduate Education Graduate School Dr. Clemens Work School of Journalism Dr. Robert Balch Department of Sociology Jeff Hull School of Journalism I wanted another piece of bread, and I wanted it bad . “Shit!” I muttered to myself, “To think of all the bread we’ve thrown into the garbage can!” . I worked myself into a fine fury. All because there wasn’t an extra crust of bread in the house. Idiotic! Thoroughly idiotic! In my delirium I began to dwell on malted milk shakes, and how, in America, there was always an extra glassful waiting for you in the shaker.