1 Virtual Poster Session November 7, 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Protecting Patient Confidentiality
MHS Privacy Electronic Access to Protected Health Information Protecting Patient Confidentiality TheThe purpose purpose of of this this module module is is to to explain explain to to all all Mayo Mayo Clin Clinicic and and Mayo Mayo Clinic Clinic Health Health SystemSystem employees employees and and credentialed credentialed non-Mayo non-Mayo an andd non-Mayo non-Mayo Clinic Clinic Health Health System System staff staff thethe policy policy regarding regarding electronic electronic access access to to protected protected health health information. information. TheThe privacyprivacy policypolicy forfor electronicelectronic accessaccess toto protectedprotected healthhealth informationinformation waswas revisedrevised andand approvedapproved byby thethe BoardBoard ofof GovernorsGovernors onon JanuaryJanuary 12,12, 2009.2009. MayoMayo ClinicClinic andand MayoMayo HealthHealth SystemSystem sitessites nownow havehave aa consistentconsistent privacyprivacy policypolicy forfor electronicelectronic accessaccess toto patientpatient medicalmedical informationinformation acrossacross allall sites.sites. Specific objectives include: •• ExplainExplain thethe MayoMayo andand MayoMayo ClinicClinic HealthHealth SystemSystem PrivacyPrivacy PolicyPolicy regardingregarding electronicelectronic accessaccess toto protectedprotected healthhealth information.information. •• SummarizeSummarize thethe consequencesconsequences forfor inappropriateinappropriate accessaccess toto patientpatient medicalmedical information.information. •• IdentifyIdentify situationssituations -

Mesenteric Panniculitis – a Rare Diagnosis
ARC Journal of Immunology and Vaccines Volume 4, Issue 2, 2019, PP 3-6 www.arcjournals.org Mesenteric Panniculitis – A Rare Diagnosis Atanas Kundurdjiev, Iva Angelova, Milena Nikolova*, Tsvetelina Vutova, Antonia Hadjiiska, Juri Todorov, Marin Penkov, Tsvetelina Dobreva, Borislav Kochmalarski, Kalina Chupetlovska, Yordan Vlahov *Clinic of Nephrology, University Hospital St. Ivan Rilski, Medical University, Sofia, Bulgaria University Hospital St. Ivan Rilski, Medical University, Sofia, Bulgaria *Corresponding Author: Milena Nikolova, MD, Ph.D, Clinic of Nephrology, University Hospital St. Ivan Rilski, Medical University, Sofia, Bulgaria. Email: [email protected] Abstract: Mesenteric panniculitis (MP, also known as sclerosing mesenteritis, mesenterial lipodystrophy, retractile mesenteritis) is a rare immune-mediated inflammatory and fibrosing condition with unknown etiology that affects the mesenteric lipocytes. MP is characterized by degeneration and necrosis of the fat tissue, chronic inflammation and the development of fibrosis within the mesenterium. The most common clinical symptoms are abdominal discomfort and pain, nausea and vomiting, palpable tumor formation in the abdomen, weight loss, fever, and symptoms of bowel obstruction. Some patients are asymptomatic and MP is detected incidentally during imaging studies for other reasons. We present a 62-years-old male patient with tumor formation in the abdomen discovered during ultrasound examination for other reasons and diagnosed on magnetic-resonance imaging as mesenteric panniculitis -

Mayo Clinic Cardiology Cardiovascular Surgery Pediatric Cardiology 2006
MAYO CLINIC CARDIOLOGY CARDIOVASCULAR SURGERY PEDIATRIC CARDIOLOGY 2006 The best interest of the patient is the only interest to be considered... –– Dr William J. Mayo Mayo Clinic Cardiology, Cardiovascular Surgery, Pediatric Cardiology 2006 T ABLE OF CONTENTS CLINICAL PRACTICE Rochester, Minnesota 2 Chest Pain and Coronary Physiology Clinic 24 Quality, Safety, and Service in the Cardiovascular Pulmonary Hypertension Clinic 25 Inpatient and Outpatient Practices 3 Valvular Heart Disease Clinic 26 Cardiac Care Unit 4 Mayo Clinic Heart Clinic in Dubai Healthcare City 26 Cardiac Catheterization Laboratory 5 Echocardiography Laboratory 6 Mayo Health System 27 Nuclear Cardiology Laboratory 7 Immanuel St. Joseph’s, Mankato, Minnesota 27 Heart Rhythm Services 8 Heart Center at Austin Medical Center, Austin, Minnesota 27 Early Atherosclerosis Clinic 10 Franciscan Skemp Healthcare, La Crosse, Wisconsin 28 Women’s Heart Clinic 10 Luther Midelfort, Eau Claire, Wisconsin 28 Hypertrophic Cardiomyopathy Clinic 11 Cardiovascular Health Clinic 11 Jacksonville, Florida 29 Cardiovascular Surgery 12 Vascular Disease 30 Congenital Heart Disease 13 Cardiopulmonary Rehabilitation Program 30 Radiation Heart Disease 13 Nuclear Cardiology Laboratory 31 Quality Control 13 Heart Transplantation and Heart Failure 32 Chronic Pulmonary Thromboembolic Disease 14 Cardiac Catheterization Laboratory 33 Healing Enhancement Program 14 Electrophysiology and Aortic Disease 15 Pacemaker/Defi brillator Services 33 Valvular Heart Disease 15 Cardiac CT/MR Imaging 34 Heart Transplantation -

Endocrinologyupdate
EndocrinologyUpdate Endocrinology News from Mayo Clinic Vol. 6, No. 4, 2011 The Knowledge Synthesis Program INSIDE THIS ISSUE The Knowledge Synthesis Program, part of the incidentalomas, growth hormone deficiency, Knowledge and Evaluation Research (KER) Unit hyperaldosteronism, pediatric obesity, hirsutism, of the Division of Endocrinology at Mayo Clinic Cushing syndrome, hyperprolactinemia, and 2 Type 2 Diabetes in Rochester, Minnesota, is an active research transgender care.” and Cardiovascular program providing methodologic support to the The KER Unit team is led by M. Hassan Disease: Managing Endocrine Society Clinical Practice Guidelines Murad, MD, MPH, of the Division of Preventive One to Prevent the Other Subcommittee. Victor M. Montori, MD, MSc, of Medicine at Mayo Clinic in Rochester, and Dr the Division of Endocrinology, Diabetes, Metabo- Montori. The team includes experienced refer- lism, and Nutrition at Mayo Clinic in Rochester, ence librarians, endocrinology staff, clinical and 4 Multifactorial Basis says: “The Knowledge Synthesis Program has sup- research fellows, research assistants, and col- for Age-Associated ported numerous clinical practice guidelines over laborators who provide additional expertise in Hypoandrogenemia the past 5 years, assisting task force members with research or guideline methods or in endocrinol- in Men formulating evidence-based recommendations ogy. Dr Murad explains: “The program follows for the care of patients with diabetes mellitus, rigorous procedures that start with developing congenital adrenal hyperplasia, male hypogonad- protocols for the systematic reviews needed to 6 Clinical Guidelines ism, osteoporosis, vitamin D deficiency, pituitary support guideline panels. Systematic reviews seek for Hyperthyroidism The KER Unit team. Standing, left to right: Juan Pablo Domecq Garces, MD, Gabriela J. -

Exploring the Use of Twitter by Leading Medical Centers in the United States
Proceedings of the 52nd Hawaii International Conference on System Sciences | 2019 Exploring the Use of Twitter by Leading Medical Centers in the United States Nima Kordzadeh Worcester Polytechnic Institute [email protected] Abstract Healthcare organizations such as hospitals and more than 50% (1713/3371) of the sampled hospitals clinics increasingly use social media platforms such had Twitter accounts. Some hospitals’ twitter channels as Twitter to raise awareness in the community about have a few hundred followers (e.g., Kapiolani Medical health and wellness issues. In line with this trend, the Center for Women & Children located in Honolulu, current study seeks to understand how Cleveland Hawaii), whereas other hospitals have hundreds of Clinic, Johns Hopkins Hospital, and Mayo Clinic use thousands of followers on Twitter (e.g., Cleveland their primary Twitter accounts to post information Clinic located in Cleveland, Ohio). related to each of the following major health topics: Healthcare organizations that use Twitter, or are brain, cancer, diabetes, diet, exercise, heart, mental planning to embrace this platform, need to first health, and obesity. Nearly 6,000 tweets posted by formulate a social media strategy, decide on what those medical centers were collected and analyzed. content to post on their channels, and learn how to The results showed that the three medical centers used effectively use Twitter, among other social media diet and cancer topics more frequently than the other environments, to promote health and wellness in the six topics in their tweets. Moreover, diabetes was community. To do so, those organizations can learn consistently the least frequently used topic in the from healthcare providers that have successfully analyzed tweets. -
St. David Lutheran
St. David Lutheran TABLE OF CONTENTS MISSION STATEMENT .............................................................................................................. 1 PHOTOS OF STAFF AND CONGREGATION COUNCIL FOR 2020 .................................. 2 PHOTOS OF NEW 2021 CONGREGATION COUNCIL MEMBERS .................................. 3 ANNUAL REPORTS Council Congregation Council Annual Report 2020 ....................................................................... 4-5 Staff Pastor’s Report 2020 .............................................................................................................. 6 In Memory, New Members and Members Transferred out ........................................ 7 Committees Altar Guild Annual Report 2020 ............................................................................................ 8 Archives Committee Annual Report 2020 ............................................................................. 9 Campus Ministry Congregational Outreach Annual Report 2020 ....................................... 10 Cemetery and Memorials Committee Annual Report 2020 ................................................. 11 Cemetery and Memorials Committee Attachment 1 - 2020 ...................................... 12-13 Cemetery and Memorials Committee Attachment 2 - 2020 ..................................... 14-15 Endowment Funds 2020 ....................................................................................................... 16 Evangelism Committee Annual Report 2020 ...................................................................... -
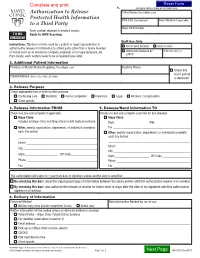
Authorization to Release Protected Health Information to a Third Party
1. (complete fields or place patient label here) Authorization to Release Patient Name (First, Middle, Last) Protected Health Information Birth Date (mm-dd-yyyy) Room Number (if applicable) to a Third Party Mayo Clinic Number Form content retained in medical record. TO BE Route to HIMS Scanning. SCANNED Staff Use Only Instructions: This form is to be used by a patient or legal representative to ROI to Send Records Scan to Chart authorize the release of information to a third party (other than a family member or friend) such as an insurance company, employer, or for legal purposes, etc. Information Released by Date (mm-dd-yyyy) LAN ID Print clearly; each section needs to be completed to be valid. 2. Additional Patient Information Previous or Maiden Name (if applies) (First, Middle, Last) Daytime Phone Check this box if patient Patient Address (Street, City, State, ZIP Code) is deceased. 3. Release Purpose Check appropriate box or write in other purpose. Continuing care Disability Forms completion Insurance Legal Workers’ compensation Other, specify ________________________________________________________________________________________________ 4. Release Information FROM 5. Release/Send Information TO Check one box and complete if applicable. Check one box and complete each line for box checked. Mayo Clinic Mayo Clinic Includes all Mayo Clinic and Mayo Clinic Health System locations Dept. ____________________ Attn. ______________________ Other, specify organization, department, or individual (complete Fax ________________________________________________ -

The Seaman Family in America Captain John Seaman
THE SEAMAN FAMILY IN AMERICA AS DESCENDED FROM CAPTAIN JOHN SEAMAN OF HEMPSTEAD, LONG ISLAND COMPILED BY MARY THOMAS SEAMAN Author of"Links in Genealogy" Life Member of The long Island Historical Society ASSISTl!I> BY JAMES HAVII.AND SEAMAN. JR. Member of the Loag Islaod Wstorial Socicly 1928 TOBlAS A. WRIGHT, INC. PRrNTERS AND PUBLISHERS NEW\"ORK SEAMAN FAMILY All.'-fS-Bal't'V wavy of six argent and a."1.1re, a c:rcscent or. CRJ;ST-A demi-sea-horse salient argent. Mono-Spcetcmur :igendo (kt us be judged by out actiot\S). CcS'aE coNTE.,'TS OF THIS BOOK ARE AUTHEllo'TIC TO THE BEST OF MY K.-.OWLEDGE. THE CONSIDEKATIO:S OF THE PUBLIC IS ASKED FOR SUCH ERRORS AS MAY J:sADVERTE.''TLY SLIP J:sTO THE MOST CAREFULLY PRE PARED MA!lo'USCRIPT. MARY THOMAS SEAMA:S ILLUSTRATIONS Coat of Arms and Crest . Frontispiece PAGE Deed of sale of land from Indians to John Seaman and others, July 4, 1657 . 16 Account of the Seaman Family, by Jordan Seaman, January, 18oo • 24 Deed of gift from John Seaman, senior, to sons Nathaniel and Richard, March 17, 1692/3 . 28 Deed of gift of Nathaniel Seaman to son Thomas, August 31, 1752 . 40 1\farriage certificate of NathaniP.1 Seaman and Rachel \Vil!is, August 9. 16g5 42 Deed of sale of land bv Richard Seaman to brother Nathaniel, September II, 1745 44 Deed of sale of land from Thomas Seaman to brothers Jacob, Nathaniel and Samuel, January 30, 1759 61 Marriage certificate of Thomas Seaman and Hannah \Villets, December 3, 174r/2 . -

Mayo Clinic Female Pelvic Medicine and Reconstructive Surgery Fellowship 1St Round Interview Participant
Mayo Clinic Female Pelvic Medicine and Reconstructive Surgery Fellowship 1st Round Interview Participant Fellowship Program Director: John A. Occhino, M.D., M.S.; [email protected] Fellowship Program Coordinator: Danette Anderson; [email protected] Address: 200 First St SW Rochester, MN 55905 Telephone: 507-266-0167 Web Site: www.mayo.edu/pelvicfellowshipminnesota Description: The Department of Obstetrics and Gynecology at Mayo Clinic in Rochester, MN, has a long history of providing renowned care in the various disciplines of gynecologic surgery. We offer a three-year Female Pelvic Medicine and Reconstructive Surgery Fellowship for physicians who wish to specialize in urogynecology and pelvic reconstructive surgery. The program provides extensive exposure to management of complex pelvic surgery beyond incontinence and prolapse. It offers you the opportunity to acquire the factual knowledge and medical and surgical skills needed to identify, evaluate, and treat the spectrum of disorders affecting the lower genitourinary tract and pelvic floor. The fellowship program aim is to prepare candidates for subspecialty certification and for a career in academic medicine. The Mayo Clinic Female Pelvic Medicine and Reconstructive Surgery Fellowship offers: • Broad spectrum of experience in pelvic surgery, with an emphasis on urogynecology and reconstructive pelvic surgery. In addition, the program emphasized experience with radical pelvic surgery, complex abdominal surgery, urogenital fistula treatment and colorectal surgery. • Multispecialty approach to evaluation and treatment of urinary incontinence and pelvic-floor disorders. Specialists from gastroenterology, urology, colorectal surgery, and physical medicine and rehabilitation collaborate to form a comprehensive team for evaluation and management. • Training focused on evaluation and treatment for a wide range of urogynecologic and pelvic floor dysfunctions. -

A M P L I G H T
St. David Lutheran ___________________________________________________________________________ March 2020 Sunday, March 1 - First Sunday in Lent 9:30 am—Sunday School/Confirmation 10:30 am—Worship/Communion Wednesday, March 4 2020 6:00 pm—Soup and Sandwich Supper 7:00 pm—Lenten Vespers ARCH M Sunday, March 8 - Second Sunday in Lent 9:30 am—Sunday School/Confirmation 10:30 am—Worship/Communion HURCH C R Wednesday, March 11 6:00 pm—Soup and Sandwich Supper E 7:00 pm—Lenten Vespers UTHERAN L T Sunday, March 15 - Third Sunday in Lent 9:30 am—Sunday School/Confirmation AVID 10:30 am—Worship/Communion H . D T S Wednesday, March 18 OF G 6:00 pm—Soup and Sandwich Supper 7:00 pm—Lenten Vespers I Sunday, March 22 - Fourth Sunday in Lent L EWSLETTER 9:30 am—Sunday School/Confirmation N 10:30 am—Worship/Communion P Wednesday, March 25 ONTHLY M 6:00 pm—Soup and Sandwich Supper M 7:00 pm—Lenten Vespers HE T A Sunday, March 29 - Fifth Sunday in Lent 9:30 am—Sunday School/Confirmation 10:30 am—Worship/Communion L Dear Brothers and Sisters in Christ, Having entered into the season of Lent, we have begun our annual pilgrimage with Jesus to the cross. In the greatest display of love the world has ever seen, God humbled himself not only to become one of us in the mystery of the incarnation, but even to suffer our own death in order to destroy the power of sin, death, and the devil. What a broken and beautiful image to think about! One of the things that we hear about each year on Ash Wednesday is about the practice of Lent—a discipline of prayer, fasting, and alms giving. -

Mesenteric Panniculitis in a Patient with New Onset Dermatomyositis Pankaj Bansal,1 Emily L Gilbert ,2 Rodrigo Otavio Lami Pereira,3 Andrew R Virata4
BMJ Case Rep: first published as 10.1136/bcr-2019-232183 on 2 February 2020. Downloaded from Unusual association of diseases/symptoms Case report Mesenteric panniculitis in a patient with new onset dermatomyositis Pankaj Bansal,1 Emily L Gilbert ,2 Rodrigo Otavio Lami Pereira,3 Andrew R Virata4 1Rheumatology, Mayo Clinic SUMMARY osteoarthritis of knees and hips, Bell’s palsy, gener- Health System, Eau Claire, Mesenteric panniculitis (MP), part of the spectrum alised anxiety disorder, irritable bowel syndrome Wisconsin, USA of sclerosing mesenteritis, is an often asymptomatic and osteoporosis with T12 compression fracture. 2Internal Medicine, Mayo disorder that is characterised by chronic inflammation Four months prior to rheumatologic evaluation, she Clinic Hospital Jacksonville, of abdominal mesentery. We present a case of an Jacksonville, Florida, USA noted a pruritic, erythematous rash on her face and 3Anesthesiology and 83- year- old woman who presented with proximal upper torso in a photodistribution (figure 1). She Perioperative Medicine - FLA, muscle weakness and erythematous, photosensitive was evaluated by a dermatologist and underwent Mayo Clinic, Jacksonville, rash of the face and upper torso and was subsequently skin biopsy showing vacuolar interface dermatitis Florida, USA diagnosed with dermatomyositis based on skin with increased dermal mucin, for which, she was 4 Pathology, Mayo Clinic Health biopsy, electromyography and muscle biopsy. She had prescribed topical corticosteroids (figures 2–4). System, Eau Claire, Wisconsin, radiographic evidence of panniculitis on CT scan of the A few weeks later, she started noticing proximal USA abdomen and pelvis for malignancy surveillance, which muscle weakness in both the upper and lower improved on serial CT scan 3 months after beginning extremities. -

Neurological Effects of COVID-19, Brain Tumors and Regenerative Medicine
May 2020 The current environment presents many challenges. Mayo Clinic's highest priority is patient and staff safety. We are taking every precaution to manage patient safety to the highest standard through universal masking, enhanced safety protocols, robust screening and COVID-19 testing strategies. Mayo Clinic has a long-standing history of helping our community in crisis while maintaining capacity to care for patients who need it most. We will continuously evaluate the circumstances at each of our sites and follow federal and state mandates to protect the safety of our patients, staff and community. Find resources for providers and answers to questions on referrals and testing for COVID-19 on the Medical Professionals Resource Center. Patient Care Holistic approach improves care for patients with spinal tumors Mayo's spinal oncology specialists may employ proton beam therapy, carbon fiber implants or surgical alternatives ― such as decompression, stabilization, ablation technologies or cement augmentation ― to meet each patient's needs. Discussing the possible neurological signs and symptoms caused by COVID-19 Mayo Clinic discusses the findings of a study of patients with COVID-19, which found that possible neurological signs and symptoms caused by COVID-19 include loss of taste and smell, headache, impaired consciousness, and stroke. Research Patients with testicular tumors should be screened early for paraneoplastic encephalitis Testicular cancer-associated paraneoplastic encephalitis causes severe neurological symptoms in men. The disease begins with a testicular tumor, which appears to cause the immune system to attack the brain. Cellular therapy, better radiation, wider access to clinical trials could help boost survival rates for patients with glioblastoma Research confirms that, despite improvements in median and short-term survival rates in glioblastoma, the percentage of patients achieving five-year survival remains low.