Getting Ready for Heart Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Protecting Patient Confidentiality
MHS Privacy Electronic Access to Protected Health Information Protecting Patient Confidentiality TheThe purpose purpose of of this this module module is is to to explain explain to to all all Mayo Mayo Clin Clinicic and and Mayo Mayo Clinic Clinic Health Health SystemSystem employees employees and and credentialed credentialed non-Mayo non-Mayo an andd non-Mayo non-Mayo Clinic Clinic Health Health System System staff staff thethe policy policy regarding regarding electronic electronic access access to to protected protected health health information. information. TheThe privacyprivacy policypolicy forfor electronicelectronic accessaccess toto protectedprotected healthhealth informationinformation waswas revisedrevised andand approvedapproved byby thethe BoardBoard ofof GovernorsGovernors onon JanuaryJanuary 12,12, 2009.2009. MayoMayo ClinicClinic andand MayoMayo HealthHealth SystemSystem sitessites nownow havehave aa consistentconsistent privacyprivacy policypolicy forfor electronicelectronic accessaccess toto patientpatient medicalmedical informationinformation acrossacross allall sites.sites. Specific objectives include: •• ExplainExplain thethe MayoMayo andand MayoMayo ClinicClinic HealthHealth SystemSystem PrivacyPrivacy PolicyPolicy regardingregarding electronicelectronic accessaccess toto protectedprotected healthhealth information.information. •• SummarizeSummarize thethe consequencesconsequences forfor inappropriateinappropriate accessaccess toto patientpatient medicalmedical information.information. •• IdentifyIdentify situationssituations -

Health Facilities and Services Review Board
STATE OF ILLINOIS HEALTH FACILITIES AND SERVICES REVIEW BOARD 525 WEST JEFFERSON ST. • SPRINGFIELD, ILLINOIS 62761 •(217) 782-3516 FAX: (217) 785-4111 DOCKET NO: BOARD MEETING: PROJECT NO: September 14, 2021 21-016 PROJECT COST: H-04 FACILITY NAME: CITY: Original: $170,520,604 NorthShore Glenbrook Hospital Glenview TYPE OF PROJECT: Substantive HSA: VII PROJECT DESCRIPTION: The Applicant [NorthShore University HealthSystem] is asking the State Board approve establishment of an open-heart surgery category of service, the addition of 8 cardiac cath labs, and the addition of 6 surgery rooms at Glenbrook Hospital in Glenview, Illinois. The cost of the project is $170,520,604. The expected completion date is December 31, 2024. The purpose of the Illinois Health Facilities Planning Act is to establish a procedure (1) which requires a person establishing, constructing or modifying a health care facility, as herein defined, to have the qualifications, background, character and financial resources to adequately provide a proper service for the community; (2) that promotes the orderly and economic development of health care facilities in the State of Illinois that avoids unnecessary duplication of such facilities; and (3) that promotes planning for and development of health care facilities needed for comprehensive health care especially in areas where the health planning process has identified unmet needs. Cost containment and support for safety net services must continue to be central tenets of the Certificate of Need process. (20 ILCS 3960/2) The Certificate of Need process required under this Act is designed to restrain rising health care costs by preventing unnecessary construction or modification of health care facilities. -

Mesenteric Panniculitis – a Rare Diagnosis
ARC Journal of Immunology and Vaccines Volume 4, Issue 2, 2019, PP 3-6 www.arcjournals.org Mesenteric Panniculitis – A Rare Diagnosis Atanas Kundurdjiev, Iva Angelova, Milena Nikolova*, Tsvetelina Vutova, Antonia Hadjiiska, Juri Todorov, Marin Penkov, Tsvetelina Dobreva, Borislav Kochmalarski, Kalina Chupetlovska, Yordan Vlahov *Clinic of Nephrology, University Hospital St. Ivan Rilski, Medical University, Sofia, Bulgaria University Hospital St. Ivan Rilski, Medical University, Sofia, Bulgaria *Corresponding Author: Milena Nikolova, MD, Ph.D, Clinic of Nephrology, University Hospital St. Ivan Rilski, Medical University, Sofia, Bulgaria. Email: [email protected] Abstract: Mesenteric panniculitis (MP, also known as sclerosing mesenteritis, mesenterial lipodystrophy, retractile mesenteritis) is a rare immune-mediated inflammatory and fibrosing condition with unknown etiology that affects the mesenteric lipocytes. MP is characterized by degeneration and necrosis of the fat tissue, chronic inflammation and the development of fibrosis within the mesenterium. The most common clinical symptoms are abdominal discomfort and pain, nausea and vomiting, palpable tumor formation in the abdomen, weight loss, fever, and symptoms of bowel obstruction. Some patients are asymptomatic and MP is detected incidentally during imaging studies for other reasons. We present a 62-years-old male patient with tumor formation in the abdomen discovered during ultrasound examination for other reasons and diagnosed on magnetic-resonance imaging as mesenteric panniculitis -

Transcatheter Mitral and Pulmonary Valve Therapy
Journal of the American College of Cardiology Vol. 53, No. 20, 2009 © 2009 by the American College of Cardiology Foundation ISSN 0735-1097/09/$36.00 Published by Elsevier Inc. doi:10.1016/j.jacc.2008.12.067 FOCUS ISSUE: VALVULAR HEART DISEASE Transcatheter Mitral and Pulmonary Valve Therapy Nicolo Piazza, MD,* Anita Asgar, MD,† Reda Ibrahim, MD,‡ Raoul Bonan, MD‡ Rotterdam, the Netherlands; London, United Kingdom; and Montreal, Quebec, Canada As the percentage of seniors continues to rise in many populations around the world, the already challenging burden of valvular heart disease will become even greater. Unfortunately, a significant proportion of patients with moderate-to-severe valve disease are refused or denied valve surgery based on age and/or accompanying comorbidities. Furthermore, because of advances in pediatric cardiology, the number of adult patients with con- genital heart disease is on the rise and over time, these patients will likely require repeat high-risk surgical pro- cedures. The aim of transcatheter valve therapies is to provide a minimally invasive treatment that is at least as effective as conventional valve surgery and is associated with less morbidity and mortality. The objective of this review was to provide an update on the clinical status, applicability, and limitations of transcatheter mitral and pulmonary valve therapies. (J Am Coll Cardiol 2009;53:1837–51) © 2009 by the American College of Cardiology Foundation The prevalence of moderate-to-severe valvular heart disease ing prevalence of adults with congenital heart disease. It is is highly age-dependent, ranging from an estimated 0.7% in safe to assume that some of these patients will require 18- to 44-year-olds in the U.S. -

(12) United States Patent (10) Patent No.: US 8,187,323 B2 Mortier Et Al
USOO8187323B2 (12) United States Patent (10) Patent No.: US 8,187,323 B2 Mortier et al. (45) Date of Patent: May 29, 2012 (54) VALVE TO MYOCARDIUM TENSION 4,372,293 A 2/1983 Vijil-Rosales MEMBERS DEVICE AND METHOD 4.409,974 A 10, 1983 Freedland 4,536,893 A 8, 1985 Parravicini 4,690,134 A 9/1987 Snyders (75) Inventors: Todd J. Mortier, Minneapolis, MN 4,705,040 A 1 1/1987 Mueller et al. (US); Cyril J. Schweich, Jr., St. Paul, 4,936,857 A 6, 1990 Kulik MN (US) 4,944,753. A 7/1990 Burgess et al. 4,960,424 A 10, 1990 Grooters (73) Assignee: Edwards Lifesciences, LLC, Irvine, CA 4,997.431 A 3, 1991 Isner et al. US 5,104,407 A 4, 1992 Lam et al. (US) 5,106,386 A 4, 1992 Isner et al. 5,131,905 A 7, 1992 Grooters (*) Notice: Subject to any disclaimer, the term of this RE34,021 E 8, 1992 Mueller et al. patent is extended or adjusted under 35 5,169,381 A 12/1992 Snyders U.S.C. 154(b) by 205 days. (Continued) (21) Appl. No.: 09/981,790 FOREIGN PATENT DOCUMENTS (22) Filed: Oct. 19, 2001 DE 36 14292 c 111987 (Continued) (65) Prior Publication Data OTHER PUBLICATIONS US 20O2/OO2908O A1 Mar. 7, 2002 Dickstein et al., “Heart Reduction Surgery: An Analysis of the Impact Related U.S. Application Data on Cardiac Function.” The Journal of Thoracic and Cardiovascular (63) Continuation of application No. 08/992.316, filed on Surgery, vol. -

Mayo Clinic Cardiology Cardiovascular Surgery Pediatric Cardiology 2006
MAYO CLINIC CARDIOLOGY CARDIOVASCULAR SURGERY PEDIATRIC CARDIOLOGY 2006 The best interest of the patient is the only interest to be considered... –– Dr William J. Mayo Mayo Clinic Cardiology, Cardiovascular Surgery, Pediatric Cardiology 2006 T ABLE OF CONTENTS CLINICAL PRACTICE Rochester, Minnesota 2 Chest Pain and Coronary Physiology Clinic 24 Quality, Safety, and Service in the Cardiovascular Pulmonary Hypertension Clinic 25 Inpatient and Outpatient Practices 3 Valvular Heart Disease Clinic 26 Cardiac Care Unit 4 Mayo Clinic Heart Clinic in Dubai Healthcare City 26 Cardiac Catheterization Laboratory 5 Echocardiography Laboratory 6 Mayo Health System 27 Nuclear Cardiology Laboratory 7 Immanuel St. Joseph’s, Mankato, Minnesota 27 Heart Rhythm Services 8 Heart Center at Austin Medical Center, Austin, Minnesota 27 Early Atherosclerosis Clinic 10 Franciscan Skemp Healthcare, La Crosse, Wisconsin 28 Women’s Heart Clinic 10 Luther Midelfort, Eau Claire, Wisconsin 28 Hypertrophic Cardiomyopathy Clinic 11 Cardiovascular Health Clinic 11 Jacksonville, Florida 29 Cardiovascular Surgery 12 Vascular Disease 30 Congenital Heart Disease 13 Cardiopulmonary Rehabilitation Program 30 Radiation Heart Disease 13 Nuclear Cardiology Laboratory 31 Quality Control 13 Heart Transplantation and Heart Failure 32 Chronic Pulmonary Thromboembolic Disease 14 Cardiac Catheterization Laboratory 33 Healing Enhancement Program 14 Electrophysiology and Aortic Disease 15 Pacemaker/Defi brillator Services 33 Valvular Heart Disease 15 Cardiac CT/MR Imaging 34 Heart Transplantation -

Endocrinologyupdate
EndocrinologyUpdate Endocrinology News from Mayo Clinic Vol. 6, No. 4, 2011 The Knowledge Synthesis Program INSIDE THIS ISSUE The Knowledge Synthesis Program, part of the incidentalomas, growth hormone deficiency, Knowledge and Evaluation Research (KER) Unit hyperaldosteronism, pediatric obesity, hirsutism, of the Division of Endocrinology at Mayo Clinic Cushing syndrome, hyperprolactinemia, and 2 Type 2 Diabetes in Rochester, Minnesota, is an active research transgender care.” and Cardiovascular program providing methodologic support to the The KER Unit team is led by M. Hassan Disease: Managing Endocrine Society Clinical Practice Guidelines Murad, MD, MPH, of the Division of Preventive One to Prevent the Other Subcommittee. Victor M. Montori, MD, MSc, of Medicine at Mayo Clinic in Rochester, and Dr the Division of Endocrinology, Diabetes, Metabo- Montori. The team includes experienced refer- lism, and Nutrition at Mayo Clinic in Rochester, ence librarians, endocrinology staff, clinical and 4 Multifactorial Basis says: “The Knowledge Synthesis Program has sup- research fellows, research assistants, and col- for Age-Associated ported numerous clinical practice guidelines over laborators who provide additional expertise in Hypoandrogenemia the past 5 years, assisting task force members with research or guideline methods or in endocrinol- in Men formulating evidence-based recommendations ogy. Dr Murad explains: “The program follows for the care of patients with diabetes mellitus, rigorous procedures that start with developing congenital adrenal hyperplasia, male hypogonad- protocols for the systematic reviews needed to 6 Clinical Guidelines ism, osteoporosis, vitamin D deficiency, pituitary support guideline panels. Systematic reviews seek for Hyperthyroidism The KER Unit team. Standing, left to right: Juan Pablo Domecq Garces, MD, Gabriela J. -

Exploring the Use of Twitter by Leading Medical Centers in the United States
Proceedings of the 52nd Hawaii International Conference on System Sciences | 2019 Exploring the Use of Twitter by Leading Medical Centers in the United States Nima Kordzadeh Worcester Polytechnic Institute [email protected] Abstract Healthcare organizations such as hospitals and more than 50% (1713/3371) of the sampled hospitals clinics increasingly use social media platforms such had Twitter accounts. Some hospitals’ twitter channels as Twitter to raise awareness in the community about have a few hundred followers (e.g., Kapiolani Medical health and wellness issues. In line with this trend, the Center for Women & Children located in Honolulu, current study seeks to understand how Cleveland Hawaii), whereas other hospitals have hundreds of Clinic, Johns Hopkins Hospital, and Mayo Clinic use thousands of followers on Twitter (e.g., Cleveland their primary Twitter accounts to post information Clinic located in Cleveland, Ohio). related to each of the following major health topics: Healthcare organizations that use Twitter, or are brain, cancer, diabetes, diet, exercise, heart, mental planning to embrace this platform, need to first health, and obesity. Nearly 6,000 tweets posted by formulate a social media strategy, decide on what those medical centers were collected and analyzed. content to post on their channels, and learn how to The results showed that the three medical centers used effectively use Twitter, among other social media diet and cancer topics more frequently than the other environments, to promote health and wellness in the six topics in their tweets. Moreover, diabetes was community. To do so, those organizations can learn consistently the least frequently used topic in the from healthcare providers that have successfully analyzed tweets. -
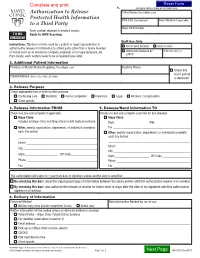
Authorization to Release Protected Health Information to a Third Party
1. (complete fields or place patient label here) Authorization to Release Patient Name (First, Middle, Last) Protected Health Information Birth Date (mm-dd-yyyy) Room Number (if applicable) to a Third Party Mayo Clinic Number Form content retained in medical record. TO BE Route to HIMS Scanning. SCANNED Staff Use Only Instructions: This form is to be used by a patient or legal representative to ROI to Send Records Scan to Chart authorize the release of information to a third party (other than a family member or friend) such as an insurance company, employer, or for legal purposes, etc. Information Released by Date (mm-dd-yyyy) LAN ID Print clearly; each section needs to be completed to be valid. 2. Additional Patient Information Previous or Maiden Name (if applies) (First, Middle, Last) Daytime Phone Check this box if patient Patient Address (Street, City, State, ZIP Code) is deceased. 3. Release Purpose Check appropriate box or write in other purpose. Continuing care Disability Forms completion Insurance Legal Workers’ compensation Other, specify ________________________________________________________________________________________________ 4. Release Information FROM 5. Release/Send Information TO Check one box and complete if applicable. Check one box and complete each line for box checked. Mayo Clinic Mayo Clinic Includes all Mayo Clinic and Mayo Clinic Health System locations Dept. ____________________ Attn. ______________________ Other, specify organization, department, or individual (complete Fax ________________________________________________ -

Heart Valve Surgery Factsheet
Heart information Heart valve surgery Contents Page 1 What are heart valves? Page 3 What is heart valve surgery? Page 3 Valve repair Page 4 Valve replacement Page 4 What happens during heart valve surgery? Page 5 Why do I need heart valve surgery? Page 6 What will happen after heart valve surgery? Page 6 Will I feel pain after the operation? Page 6 How long will I have to stay in hospital? Page 7 How long will it take to recover from heart valve surgery? Page 7 When can I start eating again? Page 8 What should I be eating? Page 8 What if I am constipated? Page 8 How active can I be? Page 9 When can I be more physically active? Page 9 When can I have sex? Page 10 Why am I so tired? Page 10 Why do I feel great one day, but dreadful the next? Page 10 When can I return to work? Page 10 Palpitations Page 11 Heart attack Page 12 Endocarditis Page 12 Will I need to take medicine? Page 13 Important things to remember about anti-coagulant medicine Page 14 Warfarin and food Page 15 What should I talk to my doctor about? Page 16 Glossary What are heart valves? For more Heart valves are like one-way doors that control the direction of blood flow between the four chambers of the heart. There are information two upper chambers (the atria) and two lower chambers (the on this topic ventricles) (see the diagram on page 2). The atria receive blood please call from the body and pump it into the ventricles. -

Medicare National Coverage Determinations Manual, Part 1
Medicare National Coverage Determinations Manual Chapter 1, Part 1 (Sections 10 – 80.12) Coverage Determinations Table of Contents (Rev. 10838, 06-08-21) Transmittals for Chapter 1, Part 1 Foreword - Purpose for National Coverage Determinations (NCD) Manual 10 - Anesthesia and Pain Management 10.1 - Use of Visual Tests Prior to and General Anesthesia During Cataract Surgery 10.2 - Transcutaneous Electrical Nerve Stimulation (TENS) for Acute Post- Operative Pain 10.3 - Inpatient Hospital Pain Rehabilitation Programs 10.4 - Outpatient Hospital Pain Rehabilitation Programs 10.5 - Autogenous Epidural Blood Graft 10.6 - Anesthesia in Cardiac Pacemaker Surgery 20 - Cardiovascular System 20.1 - Vertebral Artery Surgery 20.2 - Extracranial - Intracranial (EC-IC) Arterial Bypass Surgery 20.3 - Thoracic Duct Drainage (TDD) in Renal Transplants 20.4 – Implantable Cardioverter Defibrillators (ICDs) 20.5 - Extracorporeal Immunoadsorption (ECI) Using Protein A Columns 20.6 - Transmyocardial Revascularization (TMR) 20.7 - Percutaneous Transluminal Angioplasty (PTA) (Various Effective Dates Below) 20.8 - Cardiac Pacemakers (Various Effective Dates Below) 20.8.1 - Cardiac Pacemaker Evaluation Services 20.8.1.1 - Transtelephonic Monitoring of Cardiac Pacemakers 20.8.2 - Self-Contained Pacemaker Monitors 20.8.3 – Single Chamber and Dual Chamber Permanent Cardiac Pacemakers 20.8.4 Leadless Pacemakers 20.9 - Artificial Hearts And Related Devices – (Various Effective Dates Below) 20.9.1 - Ventricular Assist Devices (Various Effective Dates Below) 20.10 - Cardiac -

A Focus on Valve-Sparing Ascending Aortic Aneurysm Repair Newyork
ADVANCES IN CARDIOLOGY, INTERVENTIONAL CARDIOLOGY, AND CARDIOVASCULAR SURGERY Affiliated with Columbia University College of Physicians and Surgeons and Weill Cornell Medical College A Focus on Valve-Sparing NOVEMBER/DECEMBER 2014 Ascending Aortic Aneurysm Repair Emile A. Bacha, MD The most frequent location for aneurysms in the Chief, Division of Cardiac, chest occurs in the ascending aorta – and these Thoracic and Vascular Surgery aneurysms are often associated with either aortic NewYork-Presbyterian/Columbia stenosis or aortic insufficiency, especially when the University Medical Center aneurysm involves a bicuspid aortic valve. Director, Congenital and Pediatric Cardiac Surgery “We know that patients who have enlarged NewYork-Presbyterian Hospital aortas or aneurysms of the ascending aorta are at [email protected] great risk for one of two major life-threatening events: an aortic rupture or an aortic dissection,” Allan Schwartz, MD says Leonard N. Girardi, MD, Director of Chief, Division of Cardiology Thoracic Aortic Surgery in the Department of NewYork-Presbyterian/Columbia Cardiothoracic Surgery, NewYork-Presbyterian/ University Medical Center Weill Cornell Medical Center. “Dissection of the Valve-sparing ascending aortic aneurysm repair [email protected] inner lining of the wall of the blood vessel can also lead to rupture or other complications down last 15 years, the Aortic Surgery Program at Weill O. Wayne Isom, MD the line. For example, as the tear extends it may Cornell has been aggressively pursuing the devel- Cardiothoracic Surgeon-in-Chief NewYork-Presbyterian/ affect the vessels that supply the brain or the opment of a procedure that would enable surgeons Weill Cornell Medical Center coronary arteries or cause tremendous damage to to spare the patient’s native valve.