Mesenteric Panniculitis – a Rare Diagnosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Protecting Patient Confidentiality
MHS Privacy Electronic Access to Protected Health Information Protecting Patient Confidentiality TheThe purpose purpose of of this this module module is is to to explain explain to to all all Mayo Mayo Clin Clinicic and and Mayo Mayo Clinic Clinic Health Health SystemSystem employees employees and and credentialed credentialed non-Mayo non-Mayo an andd non-Mayo non-Mayo Clinic Clinic Health Health System System staff staff thethe policy policy regarding regarding electronic electronic access access to to protected protected health health information. information. TheThe privacyprivacy policypolicy forfor electronicelectronic accessaccess toto protectedprotected healthhealth informationinformation waswas revisedrevised andand approvedapproved byby thethe BoardBoard ofof GovernorsGovernors onon JanuaryJanuary 12,12, 2009.2009. MayoMayo ClinicClinic andand MayoMayo HealthHealth SystemSystem sitessites nownow havehave aa consistentconsistent privacyprivacy policypolicy forfor electronicelectronic accessaccess toto patientpatient medicalmedical informationinformation acrossacross allall sites.sites. Specific objectives include: •• ExplainExplain thethe MayoMayo andand MayoMayo ClinicClinic HealthHealth SystemSystem PrivacyPrivacy PolicyPolicy regardingregarding electronicelectronic accessaccess toto protectedprotected healthhealth information.information. •• SummarizeSummarize thethe consequencesconsequences forfor inappropriateinappropriate accessaccess toto patientpatient medicalmedical information.information. •• IdentifyIdentify situationssituations -

Mayo Clinic Cardiology Cardiovascular Surgery Pediatric Cardiology 2006
MAYO CLINIC CARDIOLOGY CARDIOVASCULAR SURGERY PEDIATRIC CARDIOLOGY 2006 The best interest of the patient is the only interest to be considered... –– Dr William J. Mayo Mayo Clinic Cardiology, Cardiovascular Surgery, Pediatric Cardiology 2006 T ABLE OF CONTENTS CLINICAL PRACTICE Rochester, Minnesota 2 Chest Pain and Coronary Physiology Clinic 24 Quality, Safety, and Service in the Cardiovascular Pulmonary Hypertension Clinic 25 Inpatient and Outpatient Practices 3 Valvular Heart Disease Clinic 26 Cardiac Care Unit 4 Mayo Clinic Heart Clinic in Dubai Healthcare City 26 Cardiac Catheterization Laboratory 5 Echocardiography Laboratory 6 Mayo Health System 27 Nuclear Cardiology Laboratory 7 Immanuel St. Joseph’s, Mankato, Minnesota 27 Heart Rhythm Services 8 Heart Center at Austin Medical Center, Austin, Minnesota 27 Early Atherosclerosis Clinic 10 Franciscan Skemp Healthcare, La Crosse, Wisconsin 28 Women’s Heart Clinic 10 Luther Midelfort, Eau Claire, Wisconsin 28 Hypertrophic Cardiomyopathy Clinic 11 Cardiovascular Health Clinic 11 Jacksonville, Florida 29 Cardiovascular Surgery 12 Vascular Disease 30 Congenital Heart Disease 13 Cardiopulmonary Rehabilitation Program 30 Radiation Heart Disease 13 Nuclear Cardiology Laboratory 31 Quality Control 13 Heart Transplantation and Heart Failure 32 Chronic Pulmonary Thromboembolic Disease 14 Cardiac Catheterization Laboratory 33 Healing Enhancement Program 14 Electrophysiology and Aortic Disease 15 Pacemaker/Defi brillator Services 33 Valvular Heart Disease 15 Cardiac CT/MR Imaging 34 Heart Transplantation -

Endocrinologyupdate
EndocrinologyUpdate Endocrinology News from Mayo Clinic Vol. 6, No. 4, 2011 The Knowledge Synthesis Program INSIDE THIS ISSUE The Knowledge Synthesis Program, part of the incidentalomas, growth hormone deficiency, Knowledge and Evaluation Research (KER) Unit hyperaldosteronism, pediatric obesity, hirsutism, of the Division of Endocrinology at Mayo Clinic Cushing syndrome, hyperprolactinemia, and 2 Type 2 Diabetes in Rochester, Minnesota, is an active research transgender care.” and Cardiovascular program providing methodologic support to the The KER Unit team is led by M. Hassan Disease: Managing Endocrine Society Clinical Practice Guidelines Murad, MD, MPH, of the Division of Preventive One to Prevent the Other Subcommittee. Victor M. Montori, MD, MSc, of Medicine at Mayo Clinic in Rochester, and Dr the Division of Endocrinology, Diabetes, Metabo- Montori. The team includes experienced refer- lism, and Nutrition at Mayo Clinic in Rochester, ence librarians, endocrinology staff, clinical and 4 Multifactorial Basis says: “The Knowledge Synthesis Program has sup- research fellows, research assistants, and col- for Age-Associated ported numerous clinical practice guidelines over laborators who provide additional expertise in Hypoandrogenemia the past 5 years, assisting task force members with research or guideline methods or in endocrinol- in Men formulating evidence-based recommendations ogy. Dr Murad explains: “The program follows for the care of patients with diabetes mellitus, rigorous procedures that start with developing congenital adrenal hyperplasia, male hypogonad- protocols for the systematic reviews needed to 6 Clinical Guidelines ism, osteoporosis, vitamin D deficiency, pituitary support guideline panels. Systematic reviews seek for Hyperthyroidism The KER Unit team. Standing, left to right: Juan Pablo Domecq Garces, MD, Gabriela J. -

Exploring the Use of Twitter by Leading Medical Centers in the United States
Proceedings of the 52nd Hawaii International Conference on System Sciences | 2019 Exploring the Use of Twitter by Leading Medical Centers in the United States Nima Kordzadeh Worcester Polytechnic Institute [email protected] Abstract Healthcare organizations such as hospitals and more than 50% (1713/3371) of the sampled hospitals clinics increasingly use social media platforms such had Twitter accounts. Some hospitals’ twitter channels as Twitter to raise awareness in the community about have a few hundred followers (e.g., Kapiolani Medical health and wellness issues. In line with this trend, the Center for Women & Children located in Honolulu, current study seeks to understand how Cleveland Hawaii), whereas other hospitals have hundreds of Clinic, Johns Hopkins Hospital, and Mayo Clinic use thousands of followers on Twitter (e.g., Cleveland their primary Twitter accounts to post information Clinic located in Cleveland, Ohio). related to each of the following major health topics: Healthcare organizations that use Twitter, or are brain, cancer, diabetes, diet, exercise, heart, mental planning to embrace this platform, need to first health, and obesity. Nearly 6,000 tweets posted by formulate a social media strategy, decide on what those medical centers were collected and analyzed. content to post on their channels, and learn how to The results showed that the three medical centers used effectively use Twitter, among other social media diet and cancer topics more frequently than the other environments, to promote health and wellness in the six topics in their tweets. Moreover, diabetes was community. To do so, those organizations can learn consistently the least frequently used topic in the from healthcare providers that have successfully analyzed tweets. -
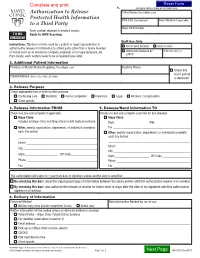
Authorization to Release Protected Health Information to a Third Party
1. (complete fields or place patient label here) Authorization to Release Patient Name (First, Middle, Last) Protected Health Information Birth Date (mm-dd-yyyy) Room Number (if applicable) to a Third Party Mayo Clinic Number Form content retained in medical record. TO BE Route to HIMS Scanning. SCANNED Staff Use Only Instructions: This form is to be used by a patient or legal representative to ROI to Send Records Scan to Chart authorize the release of information to a third party (other than a family member or friend) such as an insurance company, employer, or for legal purposes, etc. Information Released by Date (mm-dd-yyyy) LAN ID Print clearly; each section needs to be completed to be valid. 2. Additional Patient Information Previous or Maiden Name (if applies) (First, Middle, Last) Daytime Phone Check this box if patient Patient Address (Street, City, State, ZIP Code) is deceased. 3. Release Purpose Check appropriate box or write in other purpose. Continuing care Disability Forms completion Insurance Legal Workers’ compensation Other, specify ________________________________________________________________________________________________ 4. Release Information FROM 5. Release/Send Information TO Check one box and complete if applicable. Check one box and complete each line for box checked. Mayo Clinic Mayo Clinic Includes all Mayo Clinic and Mayo Clinic Health System locations Dept. ____________________ Attn. ______________________ Other, specify organization, department, or individual (complete Fax ________________________________________________ -

Mayo Clinic Female Pelvic Medicine and Reconstructive Surgery Fellowship 1St Round Interview Participant
Mayo Clinic Female Pelvic Medicine and Reconstructive Surgery Fellowship 1st Round Interview Participant Fellowship Program Director: John A. Occhino, M.D., M.S.; [email protected] Fellowship Program Coordinator: Danette Anderson; [email protected] Address: 200 First St SW Rochester, MN 55905 Telephone: 507-266-0167 Web Site: www.mayo.edu/pelvicfellowshipminnesota Description: The Department of Obstetrics and Gynecology at Mayo Clinic in Rochester, MN, has a long history of providing renowned care in the various disciplines of gynecologic surgery. We offer a three-year Female Pelvic Medicine and Reconstructive Surgery Fellowship for physicians who wish to specialize in urogynecology and pelvic reconstructive surgery. The program provides extensive exposure to management of complex pelvic surgery beyond incontinence and prolapse. It offers you the opportunity to acquire the factual knowledge and medical and surgical skills needed to identify, evaluate, and treat the spectrum of disorders affecting the lower genitourinary tract and pelvic floor. The fellowship program aim is to prepare candidates for subspecialty certification and for a career in academic medicine. The Mayo Clinic Female Pelvic Medicine and Reconstructive Surgery Fellowship offers: • Broad spectrum of experience in pelvic surgery, with an emphasis on urogynecology and reconstructive pelvic surgery. In addition, the program emphasized experience with radical pelvic surgery, complex abdominal surgery, urogenital fistula treatment and colorectal surgery. • Multispecialty approach to evaluation and treatment of urinary incontinence and pelvic-floor disorders. Specialists from gastroenterology, urology, colorectal surgery, and physical medicine and rehabilitation collaborate to form a comprehensive team for evaluation and management. • Training focused on evaluation and treatment for a wide range of urogynecologic and pelvic floor dysfunctions. -

Mesenteric Panniculitis in a Patient with New Onset Dermatomyositis Pankaj Bansal,1 Emily L Gilbert ,2 Rodrigo Otavio Lami Pereira,3 Andrew R Virata4
BMJ Case Rep: first published as 10.1136/bcr-2019-232183 on 2 February 2020. Downloaded from Unusual association of diseases/symptoms Case report Mesenteric panniculitis in a patient with new onset dermatomyositis Pankaj Bansal,1 Emily L Gilbert ,2 Rodrigo Otavio Lami Pereira,3 Andrew R Virata4 1Rheumatology, Mayo Clinic SUMMARY osteoarthritis of knees and hips, Bell’s palsy, gener- Health System, Eau Claire, Mesenteric panniculitis (MP), part of the spectrum alised anxiety disorder, irritable bowel syndrome Wisconsin, USA of sclerosing mesenteritis, is an often asymptomatic and osteoporosis with T12 compression fracture. 2Internal Medicine, Mayo disorder that is characterised by chronic inflammation Four months prior to rheumatologic evaluation, she Clinic Hospital Jacksonville, of abdominal mesentery. We present a case of an Jacksonville, Florida, USA noted a pruritic, erythematous rash on her face and 3Anesthesiology and 83- year- old woman who presented with proximal upper torso in a photodistribution (figure 1). She Perioperative Medicine - FLA, muscle weakness and erythematous, photosensitive was evaluated by a dermatologist and underwent Mayo Clinic, Jacksonville, rash of the face and upper torso and was subsequently skin biopsy showing vacuolar interface dermatitis Florida, USA diagnosed with dermatomyositis based on skin with increased dermal mucin, for which, she was 4 Pathology, Mayo Clinic Health biopsy, electromyography and muscle biopsy. She had prescribed topical corticosteroids (figures 2–4). System, Eau Claire, Wisconsin, radiographic evidence of panniculitis on CT scan of the A few weeks later, she started noticing proximal USA abdomen and pelvis for malignancy surveillance, which muscle weakness in both the upper and lower improved on serial CT scan 3 months after beginning extremities. -

Neurological Effects of COVID-19, Brain Tumors and Regenerative Medicine
May 2020 The current environment presents many challenges. Mayo Clinic's highest priority is patient and staff safety. We are taking every precaution to manage patient safety to the highest standard through universal masking, enhanced safety protocols, robust screening and COVID-19 testing strategies. Mayo Clinic has a long-standing history of helping our community in crisis while maintaining capacity to care for patients who need it most. We will continuously evaluate the circumstances at each of our sites and follow federal and state mandates to protect the safety of our patients, staff and community. Find resources for providers and answers to questions on referrals and testing for COVID-19 on the Medical Professionals Resource Center. Patient Care Holistic approach improves care for patients with spinal tumors Mayo's spinal oncology specialists may employ proton beam therapy, carbon fiber implants or surgical alternatives ― such as decompression, stabilization, ablation technologies or cement augmentation ― to meet each patient's needs. Discussing the possible neurological signs and symptoms caused by COVID-19 Mayo Clinic discusses the findings of a study of patients with COVID-19, which found that possible neurological signs and symptoms caused by COVID-19 include loss of taste and smell, headache, impaired consciousness, and stroke. Research Patients with testicular tumors should be screened early for paraneoplastic encephalitis Testicular cancer-associated paraneoplastic encephalitis causes severe neurological symptoms in men. The disease begins with a testicular tumor, which appears to cause the immune system to attack the brain. Cellular therapy, better radiation, wider access to clinical trials could help boost survival rates for patients with glioblastoma Research confirms that, despite improvements in median and short-term survival rates in glioblastoma, the percentage of patients achieving five-year survival remains low. -

Wyatt Decker, M.D. Vice President, Mayo Clinic CEO, Mayo Clinic in Arizona
______________________________________________________________________________________ Wyatt Decker, M.D. Vice President, Mayo Clinic CEO, Mayo Clinic in Arizona Dr. Wyatt Decker is a Professor of Emergency Medicine at the Mayo Clinic College of Medicine. He developed and subsequently directed the Emergency Medicine Residency training Program at Mayo Clinic, served as the inaugural Chair of the Department of Emergency Medicine in Minnesota, and Chair of Emergency Medicine at Mayo Clinic Florida. Dr. Decker has held numerous leadership positions at Mayo Clinic in Rochester, which include the oversight of hospital operations; public affairs; and the recruitment, retention and leadership development of staff physicians. Dr. Decker holds an M.B.A. from Kellogg School of Management, Northwestern University, an M.D. from Mayo Medical School, and a B.S. from the University of California-Santa Cruz. He completed internal medicine residency training at Mayo Clinic Graduate School of Medicine and Emergency Medicine training at Denver Health and Hospitals. ______________________________________________________________________________________ David Hayes, M.D. Professor of Medicine, Mayo Medical School, Mayo Clinic Medical Director, Mayo Clinic Care Network Dr. Hayes is the Medical Director of the Mayo Clinic Care Network. The network is a Mayo Clinic initiative that was launched in 2011 and designed to build durable, national and international relationships with culturally aligned health care systems. The Mayo Clinic Care Network will promote the meaningful exchange of clinical information to benefit patients, accelerate innovation and increase value in health care. Dr. Hayes received his Bachelor’s degree in Biology and Doctorate of Medicine, with distinction, from the University of Missouri in Kansas City, MO. He completed his Internship and Residency in Internal Medicine, and his Residency in Cardiovascular Disease, at the Mayo Graduate School of Medicine in Rochester, Minn. -

Mayo Clinic Urology Physician Update
September 2020 COVID-19 Updates Find resources for providers on the Medical Professionals Resource Center Find answers to questions on referrals and testing on the Medical Professionals Resource Center Patient Care Mayo Clinic task force guidelines reduce opioid prescribing after urologic surgery Prescribing patterns four months after guideline implementation were reduced to a median quantity of 100 OME (roughly 13 5 mg oxycodone tablets) compared with 150 OME before implementation. Telemedicine solutions help Mayo Clinic Urology providers connect with patients The COVID-19 pandemic provided opportunities to explore telemedicine consults with adult and pediatric urology patients. Research Study analyzes cost-effectiveness of maintenance bacillus Calmette-Guerin New research supports prioritizing bacillus Calmette-Guérin for induction therapy during shortages and reserving maintenance for patients at the highest risk of progression. See all Urology Clinical Trials at Mayo Clinic Education Mayo Clinic School of Continuous Professional Development offers online CME courses and podcasts to help meet your CME needs during the COVID-19 pandemic. Medical education from Mayo Clinic experts is also available through GIBLIB, a new on-demand medical education library. GIBLIB’s extensive offerings include full-capture surgical video with live narration by Mayo Clinic surgeons, lectures by industry leaders, and GIBLIB originals featuring timely discussions on trending topics in medicine. EDGE Talks 2020: Endourology Talks & Updates — Online CME Course with Audit Option Course expires May 30, 2023 EDGE Talks provides a comprehensive overview on the latest techniques and technology surrounding endourology. Topics covered include the use of holmium lasers in urology for the management of various diseases, with a focus on the management of urolithiasis and benign prostatic hyperplasia, percutaneous nephrolithotomy, HoLEP, new lasers, BPH management, work-life balance and ureteroscopes. -

Mayo Alumni Magazine 2006 Summer
84899 Frontcover 8/23/06 10:35 AM Page 1 DISCONTINUED DISCONTINUED DISCONTINUED DISCONTINUED Summer 2006 MayoMayo AlumniAlumni Standing room only in classroom of the future 84899 Page 1 TOC 8/23/06 10:36 AM Page 1 Mayo Alumni Summer 2006 Volume 42 Number 3 Features 2 Standing room only Can a classroom without desks affect childhood obesity? That is what two Mayo Clinic researchers wanted to find out. With the cooperation of the Rochester, Minn. school district, the researchers created a class room to study their theory. 6 When opportunity knocks, be sure to open the door Robert Nesse, M.D. discovered early on that stepping in when something interesting came along could lead to a satisfying and multifaceted career. 12 Training in real-life situations A new simulation center in Rochester provides training opportunities for physicians, allied health staff and students in a setting where everything is real except the patients. 16 Honoring excellence in patient care, research and education The Mayo Clinic Distinguished Alumni Award was established in 1981 by the Mayo Foundation Board of Trustees to recognize and show appreciation for the exceptional contributions of Mayo alumni to the field of medicine, including medical practice, research, education and administration. This year’s honorees, Hubert Frohmüller, M.D., Robert Hyatt, M.D. and Phillip Low, M.D., are profiled. Mayo Update Mayo Clinic 22 News briefs 24 Professional meetings Distinguished 24 Postgraduate meetings Alumni 26 Alumni news Awards 27 Staff news 28 Fellow, resident and student news 28 Obituaries 32 Mayo Clinic Resource Central 84899 Page 1 TOC 8/23/06 10:36 AM Page 2 Letter from the President n the face of busy schedules, staying in touch these days with old friends is sometimes a challenge. -

Mayo Clinic Pulmonology Physician Update
August 2021 Patient Care Sleep Medicine provides options for patients with obstructive sleep apnea who are PAP intolerant Mayo Clinic offers upper airway stimulation therapy, oral appliance therapy and the expertise of a sleep surgeon for patients who are positive airway pressure (PAP) therapy intolerant. Toxicity clinic to address adverse reactions to cancer treatments involving the lung Mayo Clinic Pulmonary and Critical Care Medicine is establishing a pulmonary oncologic toxicity clinic to care for patients with lung toxicity from chemotherapy, radiation and immunotherapy. Easily make referrals to Mayo Clinic or access your patients' medical records Enroll in Mayo Clinic CareLink referring physician portal to make a referral and access your patients' medical records 24/7. CareLink may be accessed on desktop and tablet browsers. See more Pulmonary Medicine news View Pulmonary Medicine specialty videos and Grand Rounds presentations Research Pulmonary function laboratories' pandemic research improves patient and provider safety Mayo Clinic pulmonary function laboratories' updated infection control practices in response to COVID-19 allowed needed testing services to reopen quickly and personal protective measures to be de-escalated safely. See all Pulmonary Medicine Clinical Trials at Mayo Clinic Education Mayo Clinic School of Continuous Professional Development offers live courses, livestreaming courses, online continuing medical education (CME) courses and podcasts to meet your CME needs. Medical education from Mayo Clinic experts is also available through GIBLIB, a new on-demand medical education library. GIBLIB provides a free seven-day trial and a 25% discount on premium annual subscriptions including unlimited CME for Mayo Clinic learners. Simply enter code MAYOCPD2021 to access this offer.